Advanced Methods for Biosensor Calibration in Complex Samples: From Foundational Principles to Clinical Applications
Accurate biosensor calibration in complex biological matrices is paramount for reliable performance in biomedical research and drug development.
Advanced Methods for Biosensor Calibration in Complex Samples: From Foundational Principles to Clinical Applications
Abstract
Accurate biosensor calibration in complex biological matrices is paramount for reliable performance in biomedical research and drug development. This article comprehensively examines the entire calibration workflow, from foundational principles of biosensor operation and key performance metrics to advanced methodological approaches for handling sample complexity. We explore cutting-edge troubleshooting strategies to overcome interference, noise, and matrix effects, while providing rigorous validation frameworks and comparative analyses of different calibration techniques. By synthesizing current research and emerging trends, this resource equips scientists with the knowledge to implement robust calibration protocols that ensure data integrity across diverse applications, from therapeutic monitoring to diagnostic biomarker detection.
Core Principles and Performance Metrics for Biosensor Calibration
Core Concepts: Bioreceptor vs. Transducer
A biosensor is an analytical device that integrates a biological recognition element (bioreceptor) with a physicochemical transducer to detect a specific analyte [1] [2]. The bioreceptor is responsible for selective interaction with the target molecule, while the transducer converts this biological event into a measurable signal [3].
Bioreceptors provide the specificity of a biosensor. They are biological molecules or structures capable of recognizing a particular analyte with high affinity [1]. The transducer's role is to convert the biochemical response resulting from the bioreceptor-analyte interaction into an quantifiable output, such as an electrical or optical signal [1] [3].
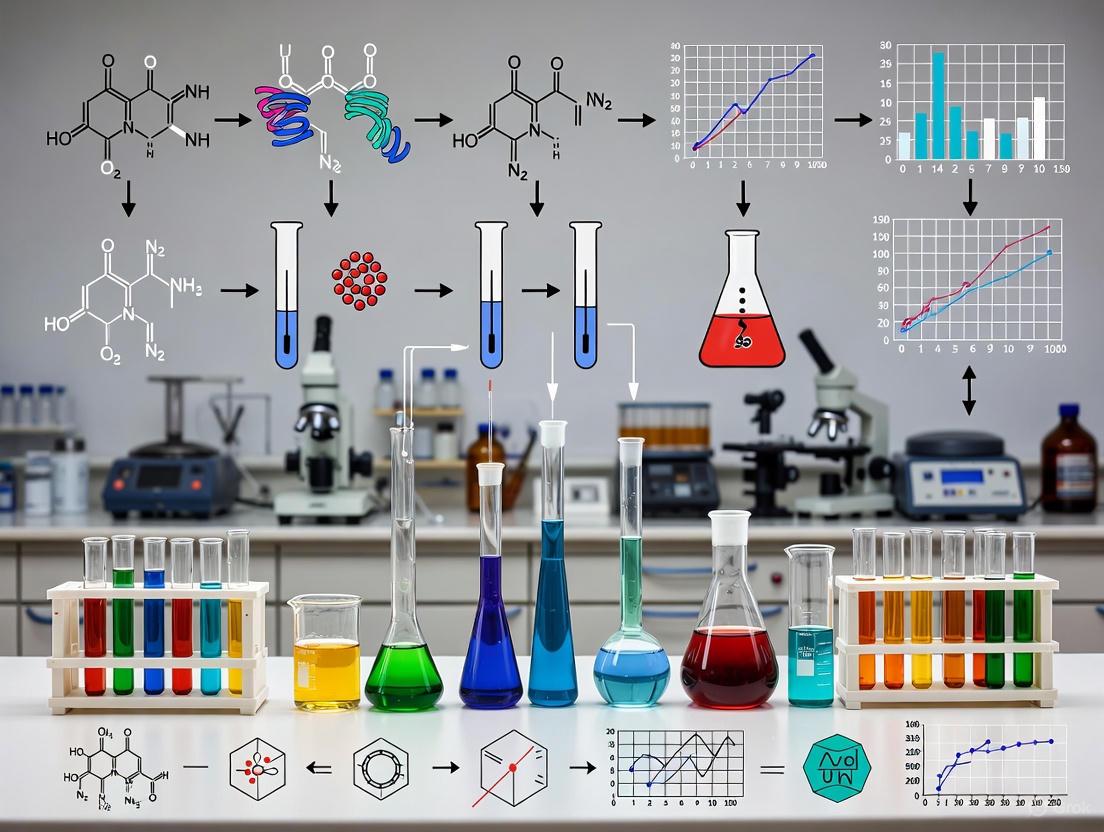
∎ Biosensor Architecture Diagram
Frequently Asked Questions & Troubleshooting Guides
∎ Biosensor Selection and Setup
What is the fundamental difference between a bioreceptor and a transducer? The bioreceptor is the biological component (e.g., enzyme, antibody, nucleic acid) that selectively binds to the target analyte. The transducer is the physical component (e.g., electrode, optical detector) that converts the binding event into a measurable signal [1] [3]. For example, in a glucose biosensor, the enzyme glucose oxidase is the bioreceptor, while the oxygen electrode is the transducer [1].
How do I select the appropriate bioreceptor for my target analyte? Choose a bioreceptor based on the required specificity and the nature of your analyte [4] [3].
- Enzymes: Ideal for substrates and catalytic reactions (e.g., glucose oxidase for glucose) [3].
- Antibodies: Excellent for specific antigen binding (e.g., immunosen sors for pathogens or proteins) [3].
- Nucleic Acids (DNA/RNA): Used for detecting complementary sequences, mutations, or specific genetic markers [3] [2].
- Whole Cells or Tissues: Provide complex responses for toxin detection or metabolic profiling [2].
What are the key characteristics of a high-performance biosensor? When selecting or designing a biosensor, optimize for these core characteristics [1]:
- Selectivity: The ability to measure the analyte in a sample containing adulterants.
- Sensitivity: The minimum amount of analyte that can be reliably detected (Limit of Detection, or LOD).
- Reproducibility: The precision and accuracy of repeated measurements.
- Stability: The susceptibility to ambient disturbances and the degradation rate of the bioreceptor.
- Linearity: The concentration range over which the sensor response is linearly proportional to analyte concentration.
∎ Troubleshooting Common Experimental Issues
My biosensor signal is unstable or drifting. What could be the cause? Signal drift often stems from bioreceptor instability or environmental factors [1] [2].
- Bioreceptor Degradation: Enzymes and antibodies can denature over time. Ensure proper storage conditions and check the shelf life of your bioreceptor components [1].
- Temperature Fluctuations: Many biological interactions are temperature-sensitive. Perform experiments in a temperature-controlled environment or use biosensors with built-in temperature compensation [1] [2].
- Calibration Error: Recalibrate the sensor regularly using fresh standard solutions. A common pitfall is using expired or contaminated buffer solutions for calibration [5].
- Fouling or Contamination: In complex samples (e.g., serum, wastewater), matrix components can non-specifically adsorb to the sensor surface. Use blocking agents or antifouling coatings to minimize this interference [2].
The sensitivity of my biosensor is lower than expected. How can I improve it? Low sensitivity can be addressed by enhancing the signal transduction or the biorecognition efficiency [2].
- Check Immobilization: The bioreceptor may be denatured or inaccessible. Optimize your immobilization method (e.g., covalent attachment, adsorption, entrapment) to maintain biological activity and orientation [2].
- Employ Nanomaterials: Integrate nanostructured materials (e.g., gold nanoparticles, graphene, MOFs) into your transducer. They increase the effective surface area, improving the loading of bioreceptors and enhancing the output signal [1] [2] [6].
- Verify Sample pH: The activity of the bioreceptor can be highly dependent on pH. Ensure the sample pH is within the optimal operating range for your specific bioreceptor [5].
- Amplification Strategies: For optical biosensors, use fluorescent labels or enzymes (e.g., horseradish peroxidase) that generate amplified products. For electrochemical sensors, consider using redox mediators [3] [2].
My biosensor shows poor selectivity in complex samples. What should I do? Poor selectivity is often due to non-specific binding or interference [1] [2].
- Optimize Blocking: After immobilizing the bioreceptor, block the remaining active surfaces on the sensor with inert proteins (e.g., BSA, casein) or other blocking agents to prevent non-specific adsorption [2].
- Sample Pre-treatment: Pre-filter, dilute, or desalt complex samples to reduce interferent concentration before analysis.
- Use a Ratiometric Design: Ratiometric biosensors, which measure the ratio of signals at two different wavelengths or potentials, provide an internal calibration that can correct for environmental interference and improve robustness in complex matrices [6].
- Check Bioreceptor Cross-reactivity: Validate the specificity of your antibody or aptamer against potential interfering compounds with similar structures.
∎ Systematic Troubleshooting Workflow
Experimental Protocols for Biosensor Calibration in Complex Samples
∎ Protocol 1: Calibration and Validation in a Simulated Complex Matrix
This protocol is designed to establish a calibration curve and validate biosensor performance in the presence of potential interferents, a critical step for research involving complex samples like serum or wastewater [2] [5].
1. Objective: To generate a standard calibration curve for the target analyte and determine the biosensor's Limit of Detection (LOD) and linear range in a controlled buffer system.
2. Materials:
- Biosensor system (with integrated bioreceptor and transducer)
- Stock solution of the pure analyte
- Appropriate assay buffer (e.g., PBS, pH 7.4)
- Standard solutions of known potential interferents
3. Methodology:
- Step 1: Preparation. Prepare a series of analyte standard solutions in assay buffer, covering the expected concentration range (e.g., from pM to μM).
- Step 2: Calibration. Measure the biosensor response for each standard solution. Perform measurements in triplicate.
- Step 3: Data Analysis. Plot the sensor response (e.g., current, fluorescence intensity) against the analyte concentration. Fit the data to determine the linear range, sensitivity (slope), and LOD (typically calculated as 3×standard deviation of the blank/slope).
4. Validation in Complex Matrix:
- Step 4: Spike-and-Recovery. Take a sample of the complex matrix (e.g., diluted serum) that is free of the analyte ("blank matrix"). Spike it with known concentrations of the pure analyte.
- Step 5: Measurement and Calculation. Measure the biosensor response for the spiked samples. Calculate the percentage recovery:
(Measured Concentration / Spiked Concentration) × 100%. Recoveries between 80-120% generally indicate good accuracy and minimal matrix interference [6].
∎ Key Research Reagent Solutions
The following reagents are essential for biosensor development and calibration experiments, particularly when working with complex samples.
| Reagent / Material | Function & Explanation |
|---|---|
| High-Affinity Bioreceptors (e.g., monoclonal antibodies, aptamers) | Provides the selectivity for the target analyte. High affinity reduces non-specific binding in complex matrices [1] [3]. |
| Blocking Agents (e.g., BSA, casein, synthetic blockers) | Reduces non-specific binding by adsorbing to unused sites on the sensor surface after bioreceptor immobilization, thereby lowering background noise [2]. |
| Nanomaterial Enhancers (e.g., gold nanoparticles, graphene, MOFs) | Increases signal strength and sensitivity by providing a high surface-to-volume ratio for greater bioreceptor loading and enhancing transduction efficiency (e.g., plasmonic effects, electrical conductivity) [1] [2] [6]. |
| Ratiometric Probes (e.g., dual-emission fluorescent dyes, reference electrodes) | Provides an internal calibration by measuring the ratio of two signals. This corrects for instrument fluctuations and environmental variability, improving accuracy in complex samples [6]. |
| Antifouling Coatings (e.g., PEG, zwitterionic polymers) | Prevents biofouling by creating a hydration layer that resists the non-specific adsorption of proteins, cells, and other biomolecules from complex samples like blood or wastewater [2]. |
In biosensor research, the accuracy and reliability of data generated from complex samples are paramount. Three fundamental metrics—Dynamic Range, Sensitivity, and Limit of Detection (LOD)—form the cornerstone of robust biosensor calibration and validation. Proper characterization of these parameters ensures that your biosensor can deliver selective, quantitative analytical information with the required precision for pharmaceutical and clinical applications [7]. The process of establishing these performance characteristics meets the requirements for the intended analytical application is often referred to as method validation [8]. This guide addresses frequent challenges researchers encounter during this critical process, providing targeted troubleshooting advice and experimental protocols to enhance your biosensor's performance.
Key Concepts and Definitions
What is the Limit of Detection (LOD) and how is it properly determined?
The Limit of Detection (LOD) is defined as the lowest concentration of an analyte in a sample that can be detected—though not necessarily quantified—with a stated probability under the stated experimental conditions [8]. It represents the smallest solute concentration that your analytical system can reliably distinguish from a blank sample (one without analyte) [8] [9].
Common Problem: Many researchers incorrectly calculate LOD by simply dividing the instrument resolution by the sensitivity, which can yield unrealistically low values that don't reflect actual performance [9].
Correct Approaches:
Method I: Using Blank Standard Deviation
- Make repeated measurements (n~20) of a blank sample to determine the mean signal (ȳB) and standard deviation (sB).
- The LOD is then calculated as: LOD = ȳB + k × sB, where k is a numerical factor chosen based on the desired confidence level [8] [9].
- For a factor of k=3, the probability of a false positive is approximately 7% [8]. IUPAC recommends this approach for LOD determination [9].
Method II: Using a Calibration Curve
- Prepare and measure a series of standard solutions at different concentrations, including some near the suspected LOD.
- Generate a linear calibration curve (y = aC + b, where 'a' is the sensitivity/slope).
- The LOD can be estimated as: LOD = 3 × sB / a, where sB is the standard deviation of the blank and 'a' is the slope of your calibration curve [10] [9].
Table 1: Comparison of LOD Determination Methods
| Method | Data Requirements | Advantages | Limitations |
|---|---|---|---|
| Blank Standard Deviation | 20+ blank measurements | Direct measurement of noise at zero concentration | Requires many replicates; may not account for matrix effects |
| Calibration Curve | Multiple low-concentration standards | Uses actual sensor response near LOD; more practical | Requires careful selection of low concentration standards |
How do I distinguish between Sensitivity and Limit of Detection?
Problem: Researchers often conflate sensitivity with LOD, leading to incorrect performance characterization.
Solution:
- Sensitivity is the analytical sensitivity defined as the slope (a) of your calibration curve (the change in sensor response per unit change in analyte concentration) [8] [9]. A steeper slope indicates higher sensitivity.
- LOD is the lowest concentration that can be reliably detected and depends on both sensitivity and the noise level of your measurement system [9].
A sensor can have high sensitivity but poor LOD if it has high background noise, or conversely, good LOD with moderate sensitivity if the system is very stable with low noise [9].
What defines the Dynamic Range of a biosensor and why is it crucial for complex samples?
The Dynamic Range (or working range) is the span of concentrations over which your biosensor provides accurate quantitative measurements. It is typically bounded at the lower end by the LOD and at the upper end by signal saturation [10].
Problem: In complex samples with unknown analyte concentrations, a narrow dynamic range may require extensive sample dilution or concentration, introducing error and increasing processing time.
Solution:
- The dynamic range is typically assessed by plotting sensor response against the logarithm of analyte concentration, which often produces a sigmoidal curve [10].
- The linear portion of this curve represents the working range where quantitative measurements are most accurate [10].
- For example, a novel GEM-based biosensor for heavy metal detection showed a linear dynamic range for Cd²⁺, Zn²⁺, and Pb²⁺ in the range of 1–6 ppb, making it suitable for detecting low concentrations of these metal ions [11].
Troubleshooting Common Calibration Issues
How can I improve my biosensor's Limit of Detection?
Problem: Unacceptably high LOD limits application for trace analysis.
Solutions:
- Signal Processing: Implement advanced signal processing techniques including noise reduction algorithms and signal amplification methods to enhance signal-to-noise ratio [10].
- Nanomaterials: Incorporate nanostructured materials (nanoparticles, nanowires) to increase surface area for biomolecule interactions and amplify sensing signals [10].
- Reference Sensors: Use a dual-sensor approach with a reference sensor to compensate for background interference, as demonstrated in fiber-optic systems where a reference oxygen optrode detected and compensated for response changes caused by bacterial growth or temperature fluctuations [7].
- Multi-Modal Sensing: Combine complementary sensing mechanisms (e.g., mechanical and optical resonances) to overcome limitations of individual techniques [10].
What strategies can extend the Dynamic Range of my biosensor?
Problem: Sensor response saturates at high analyte concentrations, requiring sample dilution.
Solutions:
- Multi-Modal Detection: Implement triple-mode biosensors that integrate three independent detection mechanisms, each covering different concentration ranges, to create an extended overall dynamic range [12].
- Surface Chemistry Optimization: Modify sensor architecture and surface chemistry to reduce steric hindrance and increase binding site availability [10].
- Array-Based Systems: Develop multiplexed resonant biosensor systems with different receptor affinities to cover a wider concentration spectrum [10].
- Data Processing: Utilize mathematical models and curve-fitting algorithms that can accurately interpret both linear and saturation regions of the sensor response [10].
How do I handle matrix effects in complex samples?
Problem: Sample matrix components interfere with biosensor response, causing inaccurate readings.
Solutions:
- Internal Standards: Use appropriate internal standard elements that are not found in your samples and don't spectrally interfere with analytes. Monitor their recovery rates to correct for matrix effects [13].
- Microfluidic Integration: Implement microfluidic systems for precise sample handling, controlled flow rates, and efficient mixing to reduce matrix interference [10].
- Sample Preparation: When possible, dilute samples to reduce concentration of interfering compounds while ensuring analytes remain above LOD [13].
Experimental Protocols for Metric Characterization
Standard Protocol for Determining LOD Using Calibration Curve Method
Prepare Solutions:
- Create a blank solution (without analyte)
- Prepare at least 5 standard solutions at concentrations spanning from below to above the expected LOD [8]
Measurement:
- Measure each solution in replicate (n ≥ 3)
- Record sensor responses for all measurements
- Maintain constant temperature, pH, and incubation time throughout [11]
Data Analysis:
The following workflow illustrates the complete LOD determination process:
Protocol for Characterizing Dynamic Range
Sample Preparation: Prepare standard solutions covering 3-5 orders of magnitude in concentration, from well below to above expected saturation point.
Measurement: Measure sensor response for each concentration in triplicate.
Data Processing:
- Plot sensor response (y-axis) against logarithm of concentration (x-axis)
- Identify the linear region where the coefficient of determination (R²) > 0.98
- Note the lower limit (typically LOD) and upper limit (where deviation from linearity exceeds 5%) [10]
Validation: Test samples with known concentrations within the dynamic range to verify accuracy.
Advanced Approaches for Enhanced Performance
Triple-Mode Biosensing for Self-Validation
Advanced triple-mode biosensors integrate three distinct detection mechanisms (e.g., colorimetric, fluorescent, and electrochemical) in a single platform. These systems provide built-in validation through cross-referencing of signals, significantly enhancing reliability in complex samples [12]. For example, combining photothermal, colorimetric, and fluorescence detection creates a robust system where each method covers different concentration ranges and provides validation for the others [12].
Microfluidic Integration for Consistent Performance
Integrating biosensors with microfluidic systems enables:
- Precise control of flow rates and sample volumes
- Reduced matrix effects through efficient mixing
- Automated calibration and sample introduction [10]
- Implementation of reference sensors to compensate for environmental fluctuations [7]
Table 2: Research Reagent Solutions for Biosensor Calibration
| Reagent/Material | Function in Calibration | Application Example |
|---|---|---|
| Internal Standards (Y, Sc) | Correct for matrix effects & sample introduction variations [13] | ICP-OES analysis of environmental samples |
| Nanomaterials (Au nanoparticles, graphene) | Signal amplification; increased surface area for biorecognition [10] | Enhanced LOD in resonant biosensors |
| Enzyme Immobilization Matrices | Stabilize biological element; maintain activity over time [7] | Enzyme-based biosensors for continuous monitoring |
| Certified Reference Materials | Validate accuracy of calibration standards [8] | Method validation and quality control |
| Surface Functionalization Reagents | Control bioreceptor orientation and density | SPR and other label-free biosensors |
Frequently Asked Questions (FAQs)
Q1: How many replicate measurements are sufficient for reliable LOD determination? For the blank measurement method, at least 20 replicates are recommended to obtain a statistically meaningful standard deviation. For the calibration curve method, a minimum of 5 concentrations with 3 replicates each is acceptable [8].
Q2: Why do I get different LOD values when using different calculation methods? This is expected, as each method accounts for different sources of error. The blank measurement method focuses on noise at zero concentration, while the calibration curve method incorporates errors across the low concentration range. Consistently report which method you used for transparency [9].
Q3: How often should I recalibrate my biosensor? Establish a regular calibration schedule based on:
- Manufacturer recommendations
- Regulatory requirements (for regulated industries)
- Observed signal drift in continuous monitoring
- When analyzing samples with markedly different matrices [7]
Q4: What acceptance criteria should I use for internal standard recovery? While some regulatory agencies suggest ±20% recovery compared to calibration solutions, the actual acceptable range should be determined based on your specific analysis requirements. More importantly, pay close attention to the precision of internal standard replicates—RSDs greater than 3% should be investigated [13].
Q5: How can I make my LOD and dynamic range characterization more reproducible?
- Always perform characterization under standardized conditions (temperature, pH, buffer composition) [10]
- Use the same reagent batches throughout characterization
- Document all instrumental parameters
- Follow established guidelines like IUPAC recommendations [9]
Proper characterization of dynamic range, sensitivity, and limit of detection is not merely a procedural requirement but a fundamental practice that determines the real-world applicability of your biosensor. By implementing these troubleshooting guidelines and experimental protocols, researchers can generate more reliable, reproducible data that stands up to scientific and regulatory scrutiny, ultimately advancing the field of biosensing in complex sample analysis.
Troubleshooting Guide & FAQs for Biosensor Calibration in Complex Samples
This technical support center addresses common challenges researchers encounter when calibrating biosensors for use in complex samples such as biological fluids, food homogenates, or environmental extracts. A deep understanding of the critical parameters—Signal-to-Noise Ratio (SNR), Selectivity, and Response Time—is essential for obtaining reliable data.
Frequently Asked Questions
1. How can I improve my biosensor's signal-to-noise ratio in turbid samples like blood serum?
A low SNR in complex matrices is often caused by light scattering (in optical sensors), fouling of the electrode surface (in electrochemical sensors), or non-specific binding. To address this:
- Use Permselective Membranes: Coat your sensor with a membrane like Nafion or cellulose acetate. These membranes block large, interfering molecules (like proteins) based on charge or size, while allowing the target analyte to pass through, thereby reducing background noise [14].
- Employ a Sentinel Sensor: Implement a reference sensor that is identical to your biosensor but lacks the biological recognition element (e.g., the enzyme is replaced with Bovine Serum Albumin). The signal from this "blank" sensor, which arises solely from matrix interferences, can be electronically subtracted from your biosensor's signal [14] [7].
- Leverage Machine Learning: Train machine learning models, such as Random Forests or Gaussian Process Regression, on the dynamic response data of your biosensor. These models can learn to distinguish the pattern of the specific analyte signal from the noise, significantly improving the fidelity of the extracted data [15] [16].
2. What are the most effective strategies to ensure selectivity for my target analyte when multiple interferents are present?
Selectivity is paramount in complex samples. Strategies can be categorized based on the biosensor generation and design.
- For First-Generation Biosensors: These are prone to interferences from electroactive compounds. The use of permselective membranes (e.g., charged polymers) is a primary defense mechanism [14].
- For Second/Third-Generation Biosensors: The use of mediators or direct electron transfer (DET) lowers the operational potential, minimizing the window for redox interferences [14] [17].
- Enzymatic Scavenging: Co-immobilize an enzyme that converts a common interferent into an inactive product. For example, ascorbate oxidase can be used to eliminate ascorbic acid interference [14].
- Multi-Sensor Arrays & Chemometrics: Use an array of sensors with slightly different specificities (e.g., enzymes from different sources or isoforms). The combined response pattern can be deconvoluted using machine learning (e.g., Linear Discriminant Analysis, Support Vector Machines) to quantify individual analytes in a mixture [14] [16] [18].
3. My biosensor has a long response time, delaying my readings. How can I speed it up without sacrificing accuracy?
Long response times can stem from slow mass transport to the sensing element or slow reaction kinetics.
- Optimize Immobilization: The enzyme immobilization method critically affects mass transfer. Ensure your 3D matrix is not too dense, which can trap the substrate and product. Physical entrapment in a porous hydrogel is often faster than thick, cross-linked polymers [17].
- Leverage Transient Response with AI: You do not need to wait for a steady-state signal. Machine learning models can be trained on the initial transient response of the biosensor to accurately predict the final analyte concentration, reducing the required data acquisition time by up to 50% or more [16].
- Use Mediators and Redox Polymers: In electrochemical biosensors, mediators shuttle electrons more efficiently from the enzyme's active site to the electrode, often resulting in a faster achievement of a measurable steady-state current [14] [17].
4. What calibration approach is best for biosensors with significant device-to-device variation, such as those based on graphene or other nanomaterials?
Variability is a known challenge in nanomaterial-based biosensors.
- High-Density Sensor Arrays: Instead of relying on a single sensor, fabricate or use chips with high-density arrays (e.g., 200+ sensing units). This provides massive redundancy [18].
- Profile-Matching Calibration: This method leverages sensor non-uniformity. Calibrate the entire array with a single, known standard solution. The unique response profile ("fingerprint") of the array to that standard can be used to calibrate subsequent measurements, eliminating the need for a full calibration curve for each sensor [18].
- Machine Learning for Inference: Train a model (e.g., Random Forest) on data from the entire array. The model will learn to ignore the variations of individual sensors and base its concentration prediction on the collective, statistically robust response of the array [18].
Performance Parameter Comparison and Methodologies
Table 1: Strategies for Optimizing Critical Biosensor Parameters
| Performance Parameter | Common Issue in Complex Samples | Recommended Solution | Key Reagents/Materials |
|---|---|---|---|
| Signal-to-Noise Ratio | Non-specific binding; sample turbidity; fouling. | Use of permselective membranes; sentinel sensors; machine learning signal processing. | Nafion; Cellulose acetate; Bovine Serum Albumin (BSA) [14]. |
| Selectivity | Electroactive interferents (e.g., ascorbate, uric acid); compounds with similar structure to the analyte. | Permselective membranes; enzymatic scavenging (e.g., ascorbate oxidase); multi-sensor arrays. | Ascorbate oxidase; charged polymers (e.g., Nafion); cross-linkers (e.g., glutaraldehyde) for array fabrication [14] [15]. |
| Response Time | Slow mass transport through immobilization matrix; slow reaction kinetics. | Optimization of immobilization matrix density; use of mediators; AI analysis of transient response. | Redox mediators (e.g., ferrocene derivatives); porous hydrogels (e.g., PVA-SbQ); glutaraldehyde [14] [17] [16]. |
Table 2: Experimental Protocol for an AI-Enhanced Calibration to Reduce Response Time and False Results
| Step | Protocol Description | Purpose |
|---|---|---|
| 1. Data Collection | Expose the biosensor to standard solutions of known analyte concentrations. Collect the full dynamic response (e.g., current vs. time, resonant frequency vs. time), not just the steady-state signal [16]. | To create a rich dataset that captures the unique kinetic "fingerprint" of the analyte binding process. |
| 2. Data Augmentation | Apply techniques like jittering, scaling, and magnitude warping to the collected dynamic response data [16]. | To artificially expand the dataset, addressing the common challenges of data sparsity and class imbalance, which improves subsequent machine learning model performance. |
| 3. Feature Engineering | Extract features from the dynamic data. Use both theory-guided features (e.g., initial rate of signal change, time constants from binding models) and traditional features (e.g., mean, variance, etc.) [16]. | To provide the machine learning model with meaningful inputs that are directly related to the underlying physico-chemical processes of sensing. |
| 4. Model Training & Validation | Train a classification model (e.g., Random Forest, Support Vector Machine) using the features from Step 3. The model learns to classify the dynamic response into the correct concentration bin [16] [18]. | To create a predictive tool that can identify the analyte concentration from a pattern of response, rather than a single point. Use k-fold cross-validation to ensure robustness. |
| 5. Deployment & Prediction | Use the trained model to predict the concentration of unknown samples based on their initial transient biosensor response. | To achieve accurate quantification with a significantly reduced data acquisition time, as the biosensor no longer needs to reach a steady-state signal [16]. |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Biosensor Development and Calibration
| Item | Function in Biosensor Research |
|---|---|
| Permselective Membranes (e.g., Nafion, Cellulose Acetate) | Coating that blocks interfering species based on charge (Nafion) or size (cellulose acetate), improving selectivity and reducing fouling [14]. |
| Enzymes for Scavenging (e.g., Ascorbate Oxidase) | Co-immobilized enzyme that converts a common electrochemical interferent (ascorbic acid) into a non-interfering product (dehydroascorbic acid) [14]. |
| Cross-linking Agents (e.g., Glutaraldehyde) | Bifunctional reagent used to covalently immobilize biorecognition elements (enzymes, antibodies) onto transducer surfaces, enhancing stability [17] [15]. |
| Redox Mediators (e.g., Ferrocene derivatives, Hexaammineruthenium(III) chloride) | Small molecules that shuttle electrons from the enzyme's active site to the electrode surface, lowering operating potential and often improving response time [14] [17]. |
| Ion-Selective Membranes (ISMs) | Lipophilic membranes containing ionophores, used to functionalize transistor-based sensors for selective ion detection (e.g., K+, Na+, Ca²⁺) in complex solutions like sweat or serum [18]. |
| Reference Sensor Components (e.g., BSA) | Used to create a "sentinel" or reference sensor that lacks specific biorecognition, allowing for signal subtraction of non-specific background effects [14]. |
Experimental Workflow and System Diagrams
The Impact of Sample Matrix Complexity on Calibration Accuracy
For researchers and scientists in drug development, achieving accurate biosensor measurements is paramount. The sample matrix—the environment in which the target analyte resides—introduces significant complexity that directly impacts calibration accuracy and reliability. Biosensors function by integrating a biological recognition element with a transducer to convert a biological event into a measurable signal [2]. However, in real-world applications, samples like blood, serum, wastewater, and food extracts are not pure solutions; they contain numerous interfering substances that can compromise the sensor's biorecognition elements, transducer signal, and overall performance [2] [19]. This technical resource center addresses the profound influence of matrix effects on biosensor calibration, providing targeted troubleshooting guidance, detailed experimental protocols, and material recommendations to enhance measurement validity for complex sample analysis within biosensor research.
FAQs: Core Principles of Matrix Effects on Calibration
1. What are "matrix effects" and why do they challenge biosensor calibration? Matrix effects refer to the phenomenon where components of a sample other than the target analyte influence the biosensor's signal output [2] [19]. In calibration, this is critical because a standard curve generated in a simple buffer may not accurately represent sensor behavior in a complex sample like blood or wastewater. These effects challenge calibration because they can alter the fundamental parameters of the sensor's response, including its sensitivity (gain), binding affinity, and signal stability, leading to inaccurate quantification of the analyte [20].
2. Which specific matrix variables most significantly impact calibration accuracy? Several key variables inherent to complex samples can derail calibration, as summarized in the table below.
Table 1: Key Matrix Variables Affecting Biosensor Calibration
| Variable | Impact on Biosensor Calibration | Common Sources |
|---|---|---|
| Temperature [20] | Alters binding affinity (K(_{1/2})), electron transfer rates, and signal gain. Mismatched temperatures between calibration and measurement cause significant quantification errors. | In-vivo measurements, environmental monitoring, process control. |
| pH & Ionic Strength [2] | Affects bioreceptor activity (e.g., enzyme denaturation) and binding equilibrium, shifting the calibration curve. | Blood, urine, fermented products, environmental waters. |
| Nonspecific Binding [2] | Proteins and other macromolecules adsorb to the sensor surface, causing signal drift and false positives. | Serum, plasma, whole blood, food homogenates. |
| Sample Age & Processing [20] | Degradation of sample components over time (e.g., in blood) can change the matrix and alter the sensor's response compared to fresh samples. | Stored clinical samples, environmental samples. |
| Interfering Chemicals | Redox-active species can interfere with electrochemical signals; auto-fluorescent compounds can obscure optical signals. | Biological fluids, food samples, industrial waste. |
3. How can I design a calibration protocol that accounts for matrix complexity? The most effective strategy is to perform calibration in a matrix that closely mimics the actual sample. For the highest accuracy in biological measurements, this means calibrating in freshly collected, undiluted whole blood at body temperature (37°C) [20]. When using a proxy calibration medium, its composition must be rigorously validated against the target matrix. Furthermore, employing a multi-point calibration curve within the expected analyte concentration range is superior to single-point calibration, as it can reveal non-linearities introduced by the matrix [20].
4. What is the role of Artificial Intelligence (AI) and advanced data processing in mitigating matrix effects? AI and machine learning (ML) can process complex biosensor outputs to correct for matrix-induced inaccuracies. For instance, Explainable AI (XAI) models can identify which design and environmental parameters most influence sensor performance, guiding robust design [21]. Advanced chemometric approaches, such as Least-Squares Support Vector Machines (LS-SVM), can model data from complex matrices like blood, correcting for interference and improving quantification accuracy compared to traditional calibration models [22].
Troubleshooting Guide: Addressing Common Calibration Failures
Table 2: Troubleshooting Common Calibration Issues in Complex Matrices
| Problem | Potential Root Cause | Corrective Action |
|---|---|---|
| Consistent over-/under-estimation | Mismatch between calibration matrix and sample matrix. | Re-calibrate using a matrix that matches the sample (e.g., fresh blood for in-vivo sensors) [20]. |
| High signal drift & poor repeatability | Nonspecific binding or biofouling of the sensor surface. | Implement improved surface chemistries: use blocking agents (e.g., BSA) or anti-fouling coatings like hydrogels [2]. |
| Low signal gain & sensitivity | Matrix components degrading the bioreceptor or inhibiting its function. | Optimize the immobilization method for the bioreceptor to enhance stability; incorporate a sample clean-up or filtration step [2]. |
| Poor reproducibility between sensors | Sensor-to-sensor fabrication variability exacerbated by matrix interference. | Use a standardized, out-of-set calibration curve validated for the specific sample type [20]. |
| Non-linear or distorted calibration curves | High cooperativity in analyte binding or environmental factors (pH, temp) affecting the bioreceptor. | Characterize sensor performance across the entire operating range (pH, temp); use multi-parameter calibration models (e.g., Hill-Langmuir isotherm) [20]. |
Experimental Protocols: Methodologies for Robust Calibration
Protocol: Calibration for In-Vivo or Whole Blood Measurements
This protocol is adapted from studies on Electrochemical Aptamer-Based (EAB) sensors for therapeutic drug monitoring (e.g., vancomycin) in whole blood [20].
1. Objective: To establish a calibration curve that enables accurate (<±10% error) quantification of an analyte in fresh, undiluted whole blood at body temperature.
2. Materials:
- Biosensors (e.g., EAB sensors with a known aptamer and redox reporter).
- Target analyte stock solutions.
- Freshly collected whole blood (e.g., rat or human). Note: Commercially sourced blood may yield different responses due to age and processing.
- Temperature-controlled electrochemical flow cell or chamber (maintained at 37°C).
- Potentiostat for square wave voltammetry (SWV) interrogation.
3. Methodology:
- Step 1: Sensor Interrogation. Immerse the sensor in fresh, body-temperature whole blood. Interrogate using SWV at two frequencies—one "signal-on" and one "signal-off"—to generate a Kinetic Differential Measurement (KDM) value, which corrects for drift.
- Step 2: Titration and Data Collection. Spike the blood with the target analyte at a minimum of 5 concentrations spanning the expected physiological range (e.g., for vancomycin: 6 to 42 µM). At each concentration, allow the signal to stabilize and record the KDM value.
- Step 3: Curve Fitting. Fit the averaged KDM values vs. concentration data to a Hill-Langmuir isotherm to derive the calibration parameters (KDMmin, KDMmax, K1/2, nH).
- Step 4: Validation. Test the calibrated sensor in separate samples of fresh, body-temperature blood dosed with known analyte concentrations. Calculate accuracy as the relative difference between expected and observed concentrations.
4. Visualization: Workflow for Optimal Biosensor Calibration The following diagram outlines the logical workflow for developing a matrix-robust calibration protocol.
Protocol: Mitigating Nonspecific Binding and Fouling in Optical Biosensors
This protocol is relevant for optical biosensors (e.g., Surface Plasmon Resonance imaging - SPRi) used in complex media like blood plasma or serum [23].
1. Objective: To validate biosensor selectivity and accuracy by minimizing nonspecific binding (NSB) from complex samples.
2. Materials:
- SPRi biosensor platform.
- Gold sensor chips.
- Bioreceptor (e.g., specific antibody).
- Cross-linkers (e.g., EDC/NHS protocol on thiol 11-MUA).
- Blocking agents (e.g., BSA, casein, or commercial blocking buffers).
- Complex samples (e.g., blood plasma from patients).
3. Methodology:
- Step 1: Surface Functionalization. Immobilize the specific bioreceptor (e.g., anti-YKL-40 antibody) onto the gold chip using a covalent chemistry like EDC/NHS.
- Step 2: Surface Blocking. Expose the functionalized sensor surface to a concentrated solution of a blocking protein (e.g., 1% BSA) to passivate any remaining active sites on the sensor surface.
- Step 3: Selectivity Test. Challenge the sensor with the complex sample (e.g., patient plasma) that does not contain the target analyte. A successful blocking step will result in a minimal change in the refractive index (or signal), indicating low NSB.
- Step 4: Accuracy Assessment. Test the blocked sensor with samples spiked with known concentrations of the analyte. The recovery rate (observed vs. expected concentration) should be close to 100%. High precision and a low coefficient of variation (CV) between measurements confirm the effectiveness of the protocol [23].
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagent Solutions for Matrix-Complex Calibration
| Reagent/Material | Function | Application Example |
|---|---|---|
| Fresh Whole Blood | Provides a physiologically relevant calibration matrix matching the sample environment. | Calibrating biosensors for in-vivo therapeutic drug monitoring (e.g., vancomycin) [20]. |
| Anti-Fouling Coatings (e.g., PEG, Hydrogels) | Form a physical barrier to prevent nonspecific adsorption of proteins and other macromolecules. | Modifying electrode or SPR chip surfaces for use in serum or plasma [2]. |
| Blocking Agents (e.g., BSA, Casein) | Passivate unused binding sites on the sensor surface after bioreceptor immobilization. | Reducing background noise in immunosensors and affinity-based sensors [23]. |
| Molecularly Imprinted Polymers (MIPs) | Synthetic bioreceptors with high stability in harsh chemical environments (pH, organic solvents). | Detecting small molecules in environmental samples (e.g., brominated flame retardants) [24]. |
| Ionic Liquids & Nanomaterials (e.g., MWCNTs) | Enhance electron transfer, stabilize bioreceptors, and increase electrode surface area. | Improving sensitivity and stability of electrochemical biosensors in complex matrices [22]. |
| Chemometric Software (e.g., LS-SVM, PLS) | Advanced algorithms to deconvolute the target signal from matrix interference. | Extracting accurate analyte concentration from complex biosensor data outputs [22]. |
A biosensor is an analytical device that combines a biological recognition element with a physicochemical transducer to detect a specific analyte [2] [25]. The core components include a bioreceptor (enzyme, antibody, nucleic acid, cell, etc.) that provides specificity, a transducer (electrochemical, optical, piezoelectric, etc.) that converts the biological interaction into a measurable signal, and an electronic system for signal processing and display [2] [25]. Biosensors provide significant advantages for research in complex samples, including real-time analysis, high specificity, and the potential for miniaturization and portability [26]. This guide focuses on the three primary biological recognition systems—protein-based, nucleic acid-based, and whole-cell systems—to support your research and development efforts.
Biosensor Type Classifications and Characteristics
The table below summarizes the key features, advantages, and challenges of the three main biosensor classes.
Table 1: Comparison of Biosensor Classification by Biorecognition Element
| Biosensor Class | Bioreceptor Examples | Key Advantages | Common Transduction Methods | Common Applications |
|---|---|---|---|---|
| Protein-Based | Enzymes (e.g., Glucose Oxidase), Antibodies, Allosteric Transcription Factors (aTFs) [2] [27] | High catalytic activity (enzymes); Exceptional specificity (antibodies); Can be engineered for novel functions [27] [25] | Electrochemical (amperometric, potentiometric) [2]; Optical (SPR, fluorescence) [26] | Medical diagnostics (e.g., glucose monitoring) [2] [28]; Drug discovery [29]; Environmental monitoring [27] |
| Nucleic Acid-Based | DNA, RNA, Aptamers, DNAzymes [27] [25] | High stability; Ease of synthesis and modification; Programmable (e.g., strand displacement) [30] | Fluorescence [30]; Electrochemical [31]; Surface Plasmon Resonance (SPR) [26] | Detection of nucleic acids, mutations [2]; Small molecule sensing [30]; In vitro diagnostics |
| Whole-Cell | Bacteria (e.g., E. coli), Yeast, Microalgae [2] [25] | Can detect global parameters (e.g., toxicity, stress); Provide functional/physiological response; Contains natural enzymatic pathways [25] | Optical (luminescence, fluorescence) [27]; Electrochemical (e.g., oxygen consumption) [25] | Toxicity and genotoxicity screening [2]; Environmental monitoring (e.g., herbicides, water pollution) [25]; Bioprocess monitoring |
The following diagram illustrates the fundamental architecture shared by all biosensors, highlighting the roles of the different biorecognition elements.
Troubleshooting Common Experimental Issues
Protein-Based Biosensors
Q1: My protein-based biosensor shows a significant loss of sensitivity over time. What could be causing this, and how can I prevent it? A: Loss of sensitivity is often related to the instability of the biological component. To address this:
- Check Immobilization: Ensure your immobilization method (adsorption, covalent binding, entrapment) maintains the protein's native structure and active site accessibility. Poor immobilization can lead to denaturation or steric hindrance [2].
- Prevent Fouling: In complex samples (e.g., serum, wastewater), nonspecific binding of other proteins or molecules can foul the sensor surface. Use effective blocking agents (e.g., BSA, casein) or incorporate anti-fouling coatings like polyethylene glycol (PEG) on your transducer surface [2].
- Control Environment: Protein activity is highly dependent on pH and temperature. Use buffered solutions to maintain optimal pH and, if possible, conduct experiments in a temperature-controlled environment. Consider using engineered enzyme mutants designed for greater stability if available [2].
Q2: How can I improve the specificity of my immunosensor to reduce false positives from matrix effects? A: Improving specificity requires optimizing the biorecognition interface.
- Optimize Antibody Orientation: Random antibody immobilization can block antigen-binding sites. Use site-specific immobilization techniques, such as coupling via Fc regions using Protein A or G, to ensure proper orientation [25].
- Include Robust Controls: Always run controls with samples that do not contain the target analyte to quantify and correct for nonspecific binding signals.
- Introduce Wash Steps: Implement stringent wash steps after the sample incubation to remove weakly and non-specifically bound molecules from the sensor surface before reading the signal.
Nucleic Acid-Based Biosensors
Q3: The response time of my DNA strand displacement-based biosensor is slower than theoretical predictions. How can I optimize the reaction kinetics? A: The kinetics of strand displacement circuits are highly dependent on the design of the nucleic acid components.
- Optimize Toehold Design: The toehold region initiates the strand displacement reaction. Ensure the toehold length is sufficient (typically 6-8 nucleotides) and has minimal secondary structure to facilitate rapid binding [30].
- Check Invader Strand Structure: The secondary structure of the invading RNA or DNA strand can significantly hinder its ability to bind the toehold. Redesign the invader sequence to minimize self-dimerization or hairpin formation, which can dramatically improve reaction speed [30].
- Tune Reaction Conditions: Adjust factors like magnesium ion concentration and temperature, which are critical for nucleic acid hybridization and strand exchange kinetics.
Q4: My aptasensor shows poor reproducibility between experimental batches. What are the key factors to standardize? A: Batch-to-batch variability often stems from inconsistencies in the bioreceptor or its attachment.
- Standardize Aptamer Folding: Aptamers require a specific tertiary structure to function. Implement a strict protocol for thermal annealing (heating and slow cooling) in an appropriate buffer to ensure consistent folding before each experiment.
- Characterize Immobilization Density: Reproducibly control the density of aptamers on the sensor surface. Too high a density can cause steric crowding, while too low a density reduces signal. Use quantitative methods to verify surface coverage.
- Use High-Purity Reagents: Ensure the synthetic oligonucleotides and chemical modifiers used for surface functionalization are of high purity (e.g., HPLC-purified).
Whole-Cell Biosensors
Q5: The signal from my whole-cell biosensor is unstable and drifts during long-term monitoring. How can I improve stability? A: Signal drift is a common challenge with living systems due to changing metabolic states.
- Control Cell Physiology: Maintain a consistent and healthy cell population. Use cells in the same growth phase (e.g., mid-log phase) for all experiments, as metabolic activity varies significantly between phases.
- Ensure Nutrient Stability: For prolonged assays, ensure that the test environment provides adequate nutrients and removes waste products to prevent changes in cell viability and baseline signal over time.
- Use Constitutive Promoters: Include an internal control, such as a reporter gene under a constitutive promoter, to normalize the target signal against variations in cell number and metabolic activity.
Q6: The sensitivity of my bacterial biosensor is lower when testing real environmental samples compared to clean lab standards. How can I overcome this? A: Complex sample matrices can introduce interference and toxicity.
- Dilute the Sample: Diluting the sample can reduce the concentration of interfering substances or general toxins to a level that does not inhibit the biosensor cells, while still allowing detection of the target analyte.
- Implement Sample Pre-treatment: Simple pre-treatment steps, such as filtration to remove particulate matter or solid-phase extraction to concentrate the analyte and remove inhibitors, can significantly improve performance [2].
- Engineer Tolerant Strains: If a specific inhibitor is known, consider using or engineering bacterial strains with higher tolerance to that substance or to the general conditions of the sample matrix (e.g., salinity, pH).
Essential Experimental Protocols
Protocol: Developing a Protein-Based Biosensor Using Directed Evolution
This protocol outlines the key steps for enhancing biosensor performance through directed evolution of protein components, such as allosteric transcription factors (aTFs) or fluorescent protein pairs [27].
Workflow:
- Library Creation: Generate a diverse library of mutant genes for your protein of interest using error-prone PCR or other gene mutagenesis techniques.
- Selection/Screening System: Clone the mutant library into an appropriate host system (e.g., bacteria, yeast) linked to a selectable or screenable output. For example, fuse the mutated aTF to a green fluorescent protein (GFP) reporter [27].
- High-Throughput Screening: Use a method like Fluorescence-Activated Cell Sorting (FACS) to screen millions of cells and isolate variants that show an improved response (e.g., higher fluorescence) in the presence of the target analyte [27].
- Characterization: Isplicate the genes from the best-performing clones, and characterize the kinetic parameters (sensitivity, specificity, dynamic range) of the new biosensor variant in vitro.
The following diagram visualizes this cyclical engineering process.
Protocol: Interfacing Cell-Free Transcription with Nucleic Acid Circuits
This protocol describes how to integrate a cell-free biosensing system with DNA strand displacement circuits to create programmable, "smart" diagnostics [30].
Workflow:
- System Assembly: Combine a cell-free transcription system (e.g., based on T7 RNA polymerase) with a DNA signal gate. The gate is a double-stranded DNA complex with a fluorophore and quencher on opposite strands.
- Sensor Configuration: Design a DNA template that includes a T7 promoter, an operator sequence for an allosteric transcription factor (aTF), and a sequence that encodes an "InvadeR" RNA strand.
- Target Detection: In the presence of the target ligand, the aTF activates transcription of the InvadeR RNA.
- Signal Generation: The synthesized InvadeR RNA binds to the DNA signal gate via toehold-mediated strand displacement, displacing the quencher strand and generating a fluorescent signal. The reaction kinetics can be tuned by optimizing the secondary structure of the InvadeR sequence [30].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Biosensor Development and Calibration
| Category | Reagent / Material | Function in Experiment | Example & Notes |
|---|---|---|---|
| Immobilization Chemistry | N-Hydroxysuccinimide (NHS) / EDC | Covalent coupling of biomolecules (proteins, aptamers) to sensor surfaces via amine groups [26]. | Standard for SPR chip functionalization [26]. |
| Self-Assembled Monolayers (SAMs) | Create a well-defined, ordered molecular layer on transducer surfaces (e.g., gold) for precise bioreceptor attachment [2]. | Often use alkanethiols on gold surfaces. | |
| Signal Generation | Fluorescent Proteins (CFP, YFP, mScarlet) | Serve as donor/acceptor pairs in FRET-based biosensors to monitor conformational changes [27] [32]. | Critical for live-cell imaging and genetically encoded biosensors. |
| Fluorophore & Quencher Pairs | Label nucleic acid strands for real-time monitoring of strand displacement reactions (e.g., in molecular beacons, signal gates) [30]. | e.g., FAM/TAMRA, Cy3/BHQ-2. | |
| Calibration Standards | "FRET-ON" & "FRET-OFF" Standards | Genetically encoded constructs used to normalize FRET ratios, correcting for variations in laser intensity and detector sensitivity across experiments [32]. | Enables quantitative cross-experiment comparison [32]. |
| Nanomaterials | Gold Nanoparticles / Nanostructures | Enhance signal transduction in optical (LSPR) and electrochemical biosensors by increasing surface area and providing unique plasmonic properties [2] [26]. | Can be functionalized with antibodies or aptamers. |
| Biological Elements | Allosteric Transcription Factors (aTFs) | Engineered protein scaffolds that change conformation upon binding a target small molecule, regulating transcription in cell-free systems [27] [30]. | Can be evolved for new ligand specificity [27]. |
| DNAzymes & Aptamers | Nucleic acids with catalytic activity or specific binding properties; can be combined for target recognition and signal generation in a single molecule [25]. | Selected via SELEX; offer high stability. |
Practical Calibration Techniques for Complex Sample Matrices
Reference Standard Preparation and Traceability in Biological Matrices
FAQs: Core Concepts and Challenges
Q1: What is a "matrix effect" and why is it a major problem for biosensing in biological samples?
A matrix effect refers to the phenomenon where components within a complex biological sample (such as serum, urine, or saliva) interfere with the biosensor's ability to accurately detect and measure the target analyte. These interferences can distort the sensor's signal, leading to unreliable results [33] [34]. Matrix molecules can mask the target, suppress or augment the signal, cause nonspecific binding to the sensor surface, or alter the biorecognition element's activity [33] [34]. For example, variations in ionic strength or pH can severely affect sensors that rely on charge-based detection, while autofluorescence can interfere with optical methods [35].
Q2: Why is proper calibration with traceable standards non-negotiable for biosensor research?
Calibration with traceable standards is the definitive link between your biosensor's raw signal and a quantitatively meaningful result (e.g., concentration). It establishes accuracy, precision, and allows for comparison of data across different laboratories and over time. Without it, results are unverifiable and potentially misleading. For instance, a study on magnetic nanosensors demonstrated excellent chip-to-chip and sensor-to-sensor reproducibility only after implementing rigorous calibration protocols, which was crucial for validating their claims of matrix insensitivity [35].
Q3: What are the key differences between preparing standards in a simple buffer versus a complex biological matrix?
Preparing standards in a simple buffer (like PBS) is straightforward but fails to account for the complex reality of real-world samples. While it is useful for initial sensor characterization, this approach does not validate the sensor's performance in the presence of matrix interferences. Preparing standards in a matched biological matrix (e.g., human serum for a blood test) is critical for assessing and mitigating matrix effects. This process, often called "spiking," involves adding a known quantity of the pure analyte into the matrix. It verifies that the sensor can accurately quantify the analyte within the challenging sample environment, ensuring the method's true robustness [34] [35].
Troubleshooting Guide: Common Issues and Solutions
| Problem Category | Specific Symptom | Potential Root Cause | Recommended Solution |
|---|---|---|---|
| Sensor Performance | Signal drift, increased noise, or loss of sensitivity. | Physical damage, fouling (e.g., biofilm, protein adsorption), or degradation of the biological recognition element [5] [34]. | Inspect sensor for damage. Clean with recommended solvents (e.g., distilled water). Implement antifouling surface coatings. Replace expired or degraded sensors [5]. |
| Calibration & Signal | Inaccurate quantification despite a clear signal. Improper standard preparation, sensor drift, or unaccounted matrix effects on calibration curve [5] [33]. | Calibrate regularly with fresh, matrix-matched standards if possible. Use stable, isotopically labeled internal standards (e.g., 13C, 15N) to correct for fluctuations and ionization effects in MS-based detection [33]. | |
| Sample Preparation | Inconsistent results, low recovery of the analyte. | Incomplete removal of matrix interferences (e.g., proteins, salts) or unintended reactivity of the analyte with matrix components [33]. | Optimize sample prep (e.g., Solid-Phase Extraction, filtration, centrifugation). For reactive analytes, use derivatization to "trap" the target molecule. Always use fresh, pH-matched buffers [33]. |
| Data Quality | High variability between replicates or unexpected results. | Non-specific binding, cross-reactivity, or improper data processing that ignores the impact of the complex sample design [33] [34] [36]. | Use appropriate blocking agents. Validate specificity in the target matrix. Apply specialized statistical software designed for complex sample data analysis [33] [36]. |
Experimental Protocol: Implementing a Matrix-Matched Standard Curve
This protocol outlines the methodology for generating a calibration curve in a biological matrix, a critical experiment for validating any biosensor intended for use with real samples. The following workflow visualizes the key stages of this process.
Detailed Methodology
Preparation of Primary Standard Stock Solution:
- Obtain a certified reference material (CRM) of the target analyte with a well-defined purity and concentration. This establishes traceability to international standards.
- Precisely weigh the CRM and dissolve it in an appropriate solvent to prepare a high-concentration stock solution (e.g., 1 mg/mL). This stock should be aliquoted and stored at the recommended temperature to maintain stability.
Serial Dilution and Spiking into Matrix:
- Perform a serial dilution of the primary stock solution using a compatible buffer (e.g., 0.1% BSA in PBS) to create a set of working standards covering the expected analytical range (e.g., from 1 pM to 100 nM) [35].
- Critical Step: Spike a fixed volume of each working standard into a constant volume of the biological matrix (e.g., pooled human serum, urine). The matrix should be as similar as possible to the intended test samples. This creates the matrix-matched calibration standards [35].
- Include a "blank" standard, which is the matrix spiked with only the buffer solvent.
Biosensor Analysis and Data Processing:
- Following the biosensor's standard operating procedure, analyze each matrix-matched standard (including the blank) in replicate (e.g., n=3 or more).
- Record the raw signal output for each standard.
- Plot the mean signal response (y-axis) against the known nominal concentration of the analyte in the matrix (x-axis).
- Apply a regression model (e.g., linear, logistic) to fit the data and establish the calibration function. The coefficient of determination (R²) should be >0.99 to indicate a robust fit [35].
Advanced Technique: Calibration Standards for FRET Biosensor Imaging
For live-cell imaging with FRET biosensors, traditional calibration is challenged by fluctuating imaging conditions. A robust solution is to use engineered calibration standards expressed in the cells themselves. The diagram below illustrates this calibration strategy.
- Generate Calibration Standards: Create cell lines expressing "FRET-ON" and "FRET-OFF" constructs. These are genetically encoded pairs of donor and acceptor fluorescent proteins locked in high-efficiency and low-efficiency FRET conformations, respectively.
- Barcode and Mix Cells: Use a barcoding method (e.g., with spectrally distinct blue or red fluorescent proteins targeted to specific organelles) to label cells expressing the calibration standards and cells expressing the biosensor of interest. Mix these populations for simultaneous imaging [32].
- Simultaneous Imaging and Normalization: In each imaging session, acquire the FRET signals from the biosensor cells and the calibration standard cells. Use the signals from the FRET-ON and FRET-OFF standards to normalize the biosensor's FRET ratio, compensating for variations in laser intensity and detector sensitivity. This yields a calibrated FRET ratio that is comparable across different experiments and over long durations [32].
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Standard Preparation & Traceability |
|---|---|
| Certified Reference Materials (CRMs) | The foundational source of traceability. These materials have certified purity and concentration values, providing an unbroken chain of comparison to a primary standard (e.g., from NIST) [35]. |
| Stable Isotope-Labeled Internal Standards (e.g., 13C, 15N) | Added to both standards and samples to correct for analyte loss during preparation and signal suppression/enhancement during mass spectrometric detection. They are preferred over deuterated standards due to minimal chromatographic isotope effects [33]. |
| Antifouling Surface Coatings (e.g., PEG, zwitterionic polymers) | Applied to biosensor surfaces to minimize nonspecific adsorption of proteins and other matrix components. This is crucial for maintaining sensitivity and accuracy in complex biological fluids like serum [34]. |
| Matrix-Matched Pooled Biological Fluids (e.g., charcoal-stripped serum) | Used as the background for preparing calibration standards. Pooled fluids average out individual variations, and charcoal-stripping can remove endogenous analytes to create a "blank" matrix for spiking experiments [35]. |
| Genetically Encoded FRET Standards (FRET-ON/OFF) | Serve as internal calibrants for live-cell fluorescence imaging. They allow for normalization of the FRET ratio, making the quantitative readout independent of variable imaging parameters [32]. |
Standard Curve Generation and Dose-Response Characterization in Complex Media
Frequently Asked Questions (FAQs)
FAQ 1: What are the most critical parameters to report from a dose-response curve for a biosensor assay? When publishing data from a biosensor assay in complex media, you should always report the potency (EC50 or IC50), the Hill Slope, and the upper (Top) and lower (Bottom) plateaus of the curve [37]. The EC50 (half-maximal effective concentration) or IC50 (half-maximal inhibitory concentration) represents the compound's potency. The Hill Slope describes the steepness of the curve. The Top and Bottom plateaus represent the maximum and minimum response levels, respectively [37]. For biosensors specifically, it is also critical to report the limit of detection (LOD) and any potential for false results, as biological components in complex media can interfere with the biorecognition elements [19].
FAQ 2: My dose-response curve is incomplete, lacking clear upper and lower plateaus. Can I still calculate an EC50 value? Yes, an EC50 can still be estimated, but you must be cautious about the type of value you report. For an incomplete curve, you can calculate a relative EC50 by fitting the data you have with a non-linear regression model (e.g., 4-parameter logistic (4PL)) and allowing the model to extrapolate the plateaus [37]. In contrast, an absolute EC50 requires the use of control values to define the minimum and maximum response and determines the concentration that gives a 50% inhibition from the maximum [37]. You should clearly state in your methods which approach was used.
FAQ 3: How many data points (concentrations) are sufficient for a reliable dose-response curve? It is generally recommended to use 5 to 10 concentrations distributed across a broad range [37]. This number of points allows for adequate characterization of the three critical parts of the curve: the bottom plateau, the top plateau, and the central, linear portion where the EC50 is located [37]. Using too few concentrations can lead to an unreliable fit and inaccurate parameter estimation.
FAQ 4: What are common sources of false results in biosensor-based dose-response experiments? False positives or negatives in biosensor assays can arise from multiple factors [19]. These include:
- Matrix Effects: Components in complex biological samples (e.g., serum, plasma) can non-specifically interact with the biosensor's bioreceptor or transducer, altering the signal [19].
- Sensor Fouling: Proteins or other macromolecules in the sample can adsorb to the biosensor surface, reducing its sensitivity and specificity [19].
- Cross-reactivity: The bioreceptor (e.g., antibody, aptamer) may bind to molecules structurally similar to the target analyte, generating a false positive signal [19].
- Signal Drift: Instabilities in the biosensor's physical or chemical properties over time can lead to inaccurate readings [19].
FAQ 5: How can I optimize my experimental design for dose-response studies? Statistical optimal design theory suggests that highly precise parameter estimates can be achieved with relatively few, strategically chosen dose levels. D-optimal designs for common models like the log-logistic or Weibull function often require only a control group and three distinct dose levels [38]. The optimal dose levels are typically placed near the anticipated EC10, EC50, and EC90, which maximizes the information gained about the curve's shape and parameters [38].
Troubleshooting Guides
Poor Curve Fit or Unreliable EC50
| Symptom | Possible Cause | Solution |
|---|---|---|
| Incomplete sigmoidal curve | The concentration range is too narrow. | Widen the concentration range to capture the lower and upper response asymptotes [37]. |
| EC50 at the extreme end of the concentration range | The concentration range is mispositioned. | Shift the tested concentration range up or down based on initial results to ensure the EC50 lies within the central part of your data [37]. |
| Shallow or too steep Hill Slope | High levels of non-specific binding or cooperativity in the system. | Check the assumptions of your model. For a system with low observations, consider constraining the Hill Slope to 1.0; for receptor-binding assays, a variable slope is often more appropriate [37]. |
| High variability in replicate measurements | Inconsistent sample preparation or biosensor fouling. | Standardize sample preparation protocols. Include control samples to assess and correct for background signal and matrix effects [19] [37]. |
High Background Signal or Noise in Complex Media
| Symptom | Possible Cause | Solution |
|---|---|---|
| Elevated signal in negative controls | Non-specific binding of matrix components to the biosensor surface. | Dilute the sample in a suitable buffer to reduce interference. Incorporate blocking agents (e.g., BSA, casein) in the running buffer. Perform a sample pre-treatment (e.g., filtration, extraction) to remove interferents [19]. |
| Signal drift over time | Fouling of the biosensor surface or instability of the biological element. | Implement more frequent calibration or standard addition protocols. Use regenerable biosensor surfaces if available. Ensure the biosensor is stored and operated within its specified environmental conditions [19]. |
| Inconsistent results between replicates | Heterogeneity of the complex sample or improper mixing. | Ensure samples are thoroughly homogenized before analysis. Increase the number of replicate measurements to account for sample variability [37]. |
Experimental Protocols
Standard Protocol for Generating a Dose-Response Curve
Principle: This protocol outlines the steps for treating a biological system with a serial dilution of a drug or analyte and fitting the resulting data to a four-parameter logistic (4PL) model to determine potency (EC50/IC50) and efficacy [37] [39].
Workflow Diagram:
Materials:
- Key Reagent Solutions:
- Stock Solution of Analyte/Drug: A highly concentrated, well-characterized solution of the test compound.
- Assay Buffer/Biological Media: The complex matrix in which the experiment is conducted (e.g., cell culture media, serum, artificial saliva).
- Standards/Controls: Solutions with known high and low (or zero) analyte concentration for signal normalization and quality control.
Step-by-Step Methodology:
- Prepare Serial Dilutions:
- Create a serial dilution of the drug/analyte in the complex media of interest. It is recommended to use 5-10 concentrations spaced logarithmically (e.g., 1, 10, 100, 1000 nM) to adequately define the curve [37].
- Include a negative control (vehicle only) and a positive control if available.
Apply Dilutions and Incubate:
- Apply each dilution to your biological system (e.g., cells, tissue) or biosensor. Ensure the number of replicates (typically n=3-6) is sufficient for statistical power [38].
- Incubate for the predetermined time under appropriate physiological conditions (e.g., 37°C, 5% CO₂).
Measure Response:
- At the endpoint, measure the response using your biosensor or assay readout (e.g., fluorescence, luminescence, electrical impedance).
- Record the raw signal data for all concentrations and controls.
Data Transformation and Normalization:
- Normalization: Convert the raw response values to a percentage of the control response. The minimum and maximum plateaus are often set to 0% and 100%, respectively [37].
- Formula:
Normalized Response = (Raw Response - Min Response) / (Max Response - Min Response) * 100
- Formula:
- Transformation: The X-values (concentrations) are typically transformed using a base-10 logarithm to linearize the relationship and facilitate a better sigmoidal fit [37].
- Normalization: Convert the raw response values to a percentage of the control response. The minimum and maximum plateaus are often set to 0% and 100%, respectively [37].
Non-Linear Regression Analysis:
- Fit the normalized data (Y: Response, X: log(Concentration)) to a four-parameter logistic (4PL) model using curve-fitting software (e.g., GraphPad Prism, R).
- The standard 4PL equation is:
Y = Bottom + (Top - Bottom) / (1 + 10^((LogEC50 - X) * HillSlope))where Bottom and Top are the lower and upper asymptotes, X is the log(concentration), and HillSlope describes the steepness of the curve [37].
Evaluation and Interpretation:
Protocol for Biosensor Calibration in Complex Media
Principle: This protocol details the process of generating a standard curve with a biosensor in a complex sample matrix using the method of standard addition to account for matrix interference [19].
Workflow Diagram:
Materials:
- Key Reagent Solutions:
- High-Purity Analyte Standards: For preparing spiking solutions.
- Blank Complex Matrix: The same media as the unknown sample but confirmed to be free of the target analyte.
- Biosensor Regeneration Buffer: If using a reusable biosensor, a buffer that removes bound analyte without damaging the biological element.
Step-by-Step Methodology:
- Sample Preparation:
- Prepare a consistent aliquot of the unknown sample in the complex media.
Standard Addition:
- Split the sample into multiple equal aliquots.
- Spike each aliquot with a known and increasing concentration of the analyte standard. Leave one aliquot unspiked (zero addition).
- The volume of the spike should be small enough to not significantly dilute the sample matrix.
Biosensor Analysis:
- Analyze each spiked sample with the biosensor according to the manufacturer's instructions or established lab protocol.
- Record the signal output for each spiked concentration.
Data Analysis:
- Plot the measured signal (Y-axis) against the concentration of the added standard (X-axis).
- Perform a linear regression on the data points.
- The absolute value of the X-intercept of the regression line corresponds to the concentration of the analyte in the original, unspiked sample. This method corrects for matrix effects that proportionally affect the signal [19].
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Experiment |
|---|---|
| Log-Logistic Model | A common non-linear regression model used to fit sigmoidal dose-response data. It estimates four parameters: Bottom, Top, EC50, and Hill Slope [38]. |
| Agonist/Antagonist | Agonists stimulate a response; Antagonists inhibit the action of an agonist. These are critical tools for probing pharmacological mechanisms in dose-response studies [37]. |
| Four-Parameter Logistic (4PL) Regression | The standard model for analyzing dose-response curves. It is synonymous with the Hill Equation and is used to quantify drug potency and efficacy [37]. |
| Nanoparticle-based Biosensors | Portable sensing platforms that use nanomaterials to enhance sensitivity and specificity. They are promising for point-of-care detection of biomarkers for diseases like diabetes and cancer [40]. |
| D-optimal Design | A statistical approach for designing efficient experiments. It helps determine the optimal number and placement of dose levels to maximize the precision of parameter estimates, often reducing the required number of experimental units [38]. |
Data Presentation Tables
Table 1: Key Parameters in Dose-Response Analysis
| Parameter | Symbol | Description | Interpretation |
|---|---|---|---|
| Half-Maximal Effective Concentration | EC50 | The concentration that produces a response halfway between the baseline (Bottom) and maximum (Top) plateaus [37]. | A measure of potency. A lower EC50 indicates greater potency. |
| Half-Maximal Inhibitory Concentration | IC50 | The concentration that produces a response halfway between the maximum (Top) and minimum (Bottom) plateaus in an inhibitory curve [37]. | A measure of inhibitory potency. A lower IC50 indicates a more effective inhibitor. |
| Hill Slope | - | A parameter that reflects the steepness of the curve at its midpoint [37]. | A slope >1 suggests positive cooperativity; <1 suggests negative cooperativity or a heterogeneous system. |
| Top Plateau | Top | The maximum response asymptote of the curve [37]. | Represents the efficacy or maximal effect of the agonist. |
| Bottom Plateau | Bottom | The minimum response asymptote of the curve [37]. | Represents the baseline response in the absence of a stimulatory agonist. |
| Equilibrium Dissociation Constant | Kd | The molar concentration of a ligand at which 50% of the receptors are occupied [39]. | A measure of binding affinity. A lower Kd indicates a higher affinity for the receptor. |
Table 2: Comparison of Common Dose-Response Models
| Model | Function | Typical Application |
|---|---|---|
| Log-Logistic | ( f(x)=\frac{d-c}{1+\exp(b(\log(x)-\log(e)))}+c ) [38] | A versatile standard for many toxicological and pharmacological dose-response studies [38]. |
| Weibull | ( f(x)=c+(d-c)\exp(-\exp(b(\log(x)-\log(e)))) ) [38] | Used for modeling time-to-event data or when the dose-response has an asymmetric sigmoidal shape [38]. |
| Log-Normal | ( f(x)=c+(d-c)\Phi(-b(\log(x)-\log(e))) ) [38] | Applicable when the underlying biological response is assumed to follow a log-normal distribution [38]. |
Genetically Engineered Microbial (GEM) Biosensors for Heavy Metal Detection
Genetically Engineered Microbial (GEM) biosensors represent a sophisticated analytical technology that combines biological components with physical transducers to detect specific contaminants. These biosensors are developed by integrating a designed genetic circuit into a microbial host, such as Escherichia coli, which produces a measurable signal—typically fluorescence—in the presence of a target heavy metal [11]. This technology has emerged as a promising alternative to conventional heavy metal detection methods like atomic absorption spectrometry, offering advantages such as portability, cost-effectiveness, and the unique ability to detect the bioavailable fraction of metals, which is most relevant for assessing environmental risk and toxicity [11] [41].
The core principle involves mimicking natural bacterial resistance mechanisms. A common design is the "NOT type" logic gate, where a repressor protein is constitutively expressed and binds to a promoter, suppressing the transcription of a reporter gene. When a specific heavy metal ion binds to the repressor protein, it causes a conformational change, releasing the repressor from the promoter and allowing the expression of the reporter gene, such as enhanced Green Fluorescent Protein (eGFP) [11]. This process enables the quantitative detection of heavy metal ions like Cd²⁺, Zn²⁺, and Pb²⁺ at very low concentrations.
Frequently Asked Questions (FAQs)
Q1: Our GEM biosensor shows low fluorescence signal even when exposed to known concentrations of Cd²⁺. What could be the cause? Several factors can lead to suboptimal signal output:
- Sub-optimal Physiological Conditions: Ensure the bacterial cells are growing at 37°C and the medium is at pH 7.0, as these are the optimal conditions for the host E. coli BL21. Significant deviations can impair cellular metabolism and reporter gene expression [11].
- Host Cell Physiology: Verify that the biosensor cells are growing naturally, exhibiting a typical sigmoid growth curve. If growth is stunted, the genetic circuit may not be functioning correctly [11].
- Reporter Gene Integrity: Confirm the expression of the reporter gene (e.g., eGFP) using molecular techniques like quantitative PCR (qPCR) and the production of the fluorescent protein via fluorometry [11].
Q2: The biosensor is producing a fluorescent signal in control samples without heavy metals. How can I address this high background noise?
- Promoter Leakiness: The genetic circuit might have inherent promoter leakiness, where the reporter gene is expressed even in the absence of the target metal. This can be mitigated by optimizing the genetic circuit design and using tighter repression systems [11].
- Non-Specific Binding: Calibrate the biosensor against non-specific metals. A well-calibrated biosensor should show high R² values for target metals (e.g., ~0.98 for Cd²⁺) and low values for non-specific metals like Fe³⁺ (R² ~0.04) or AsO₄³⁻ (R² ~0.38) [11] [42].
- Contamination: Ensure all reagents and labware are free from heavy metal contamination.
Q3: Can this biosensor detect multiple heavy metals simultaneously, and how do I interpret the results? Yes, certain GEM biosensors are designed to be sensitive to multiple heavy metals, such as Cd²⁺, Zn²⁺, and Pb²⁺, either singly or in combination [11]. However, this multi-sensitivity can make distinguishing between them in a mixed sample challenging.
- Interpretation Strategy: For precise identification of individual metals in a complex sample, the biosensor may need to be used in conjunction with complementary analytical techniques like Microwave Plasma-Atomic Emission Spectrometry (MP-AES) [11]. The biosensor is excellent for initial screening to detect the presence of bioavailable heavy metals from the group it targets.
Troubleshooting Guide
| Problem | Possible Cause | Suggested Solution |
|---|---|---|
| No fluorescence signal | Cell death or poor health | Check cell viability and growth conditions (37°C, pH 7.0) [11]. |
| Incorrect metal concentration | Prepare fresh metal stock solutions and confirm concentrations with a standard method like MP-AES [11]. | |
| Plasmid loss from host cells | Culture cells with appropriate antibiotics to maintain plasmid selection pressure. | |
| High background fluorescence | Promoter leakiness in genetic circuit | Use a control strain to establish a baseline and subtract background [11]. |
| Contamination from non-target metals | Use high-purity reagents and solvents. Calibrate against non-specific metals [11]. | |
| Signal is inconsistent between replicates | Inconsistent cell culture density | Standardize the optical density (OD) of the bacterial culture used in the assay. |
| Variable incubation time/temperature | Strictly control exposure time and incubation temperature for all replicates [11]. | |
| Low sensitivity | Biosensor operated outside linear range | Perform a full calibration curve to determine the operational range (e.g., 1-6 ppb for Cd²⁺, Zn²⁺, Pb²⁺) [11]. |
Experimental Protocols & Data Presentation
Protocol: Biosensor Calibration and Validation
This protocol outlines the steps for calibrating a GEM biosensor for quantitative heavy metal detection, a critical process for thesis research involving complex samples [11].
1. Preparation of Heavy Metal Solutions:
- Prepare 100 ppm stock solutions of target (Cd²⁺, Zn²⁺, Pb²⁺) and non-target (Fe³⁺, AsO₄³⁻, Ni²⁺) metal ions in ddH₂O using high-purity salts.
- Confirm stock solution concentrations using a standard method like Microwave Plasma-Atomic Emission Spectrometry (MP-AES).
- Perform serial dilutions to create standard solutions ranging from 0.1 ppm to 5.0 ppm (or 1 to 6 ppb). Store at room temperature [11].
2. Biosensor Exposure and Incubation:
- Grow the GEM biosensor strain (e.g., E. coli-BL21:pJET1.2-CadA/CadR-eGFP) to the mid-log phase.
- Expose a standardized aliquot of biosensor cells to the prepared metal standard solutions.
- Incubate at 37°C for a predetermined, optimized period to allow for gene expression [11].
3. Signal Measurement and Analysis:
- Measure the fluorescent intensity of the samples using a fluorometer, fluorescence microscope, or digital image processing tools.
- For each metal, plot the measured fluorescent intensity against the known metal concentration.
- Perform linear regression analysis to generate a calibration curve. The R² value should be close to 1.0 for target metals, indicating a strong linear relationship [11].
Quantitative Performance Data
The following table summarizes typical calibration data for a GEM biosensor specific for Cd²⁺, Zn²⁺, and Pb²⁺, which can be used as a benchmark for your own experiments [11] [42].
Table 1: Calibration Data for a GEM Biosensor Targeting Cd²⁺, Zn²⁺, and Pb²⁺
| Heavy Metal Ion | Linear Range (ppb) | Coefficient of Determination (R²) | Specificity (Compared to non-specific metals) |
|---|---|---|---|
| Cd²⁺ | 1 - 6 | 0.9809 | High |
| Zn²⁺ | 1 - 6 | 0.9761 | High |
| Pb²⁺ | 1 - 6 | 0.9758 | High |
| Ni²⁺ | - | 0.8498 | Low |
| AsO₄³⁻ | - | 0.3825 | Very Low |
| Fe³⁺ | - | 0.0373 | Very Low |
Signaling Pathways and Workflows
The following diagram illustrates the logical workflow of a NOT-type genetic circuit used in a GEM biosensor for heavy metal detection, based on the CadA/CadR operon system.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for GEM Biosensor Development and Assay
| Reagent/Material | Function/Description | Example or Specification |
|---|---|---|
| Host Organism | A genetically tractable microbial host for the biosensor circuit. | Escherichia coli BL21 strain [11]. |
| Plasmid Vector | A vehicle for cloning and maintaining the genetic circuit. | pJET1.2 plasmid [11]. |
| Genetic Circuit | The engineered DNA sequence that confers metal sensitivity and response. | Chemically synthesized CadA/CadR-eGFP circuit [11]. |
| Reporter Gene | A gene that produces a easily measurable signal. | enhanced Green Fluorescent Protein (eGFP) [11]. |
| Heavy Metal Salts | To prepare standard solutions for calibration and testing. | CdCl₂, Pb(NO₃)₂, Zn(CH₃COO)₂ (Sigma-Aldrich) [11]. |
| Culture Medium | To support the growth and maintenance of the biosensor cells. | LB broth, adjusted to optimum pH (e.g., 7.0) [11]. |
Troubleshooting Guides and FAQs
Q1: What are the most common causes of SERS signal fluctuation in LFIA strips, and how can a self-calibrating design correct for them?
Signal fluctuations in SERS-LFIA strips are frequently caused by instrumental factors (such as laser power variations or focusing differences), environmental conditions, physical properties of the nitrocellulose membrane (which can create heterogeneous flow paths and uneven nanoparticle deposition), and inherent sample complexity (such as variable viscosity or matrix effects in biological fluids like plasma or cell lysates) [43] [44].
A self-calibrating design integrates an internal standard (IS) directly into the biosensor's test line. This IS provides a stable reference signal against which the target-specific signal is measured. By calculating a ratio of the target signal to the internal standard signal, the biosensor can automatically correct for the aforementioned fluctuations, leading to more accurate and reliable quantification [43] [45] [44].
Q2: My self-calibrating SERS-LFIA shows poor reproducibility between different production batches. What steps can I take to improve this?
Batch-to-batch variation is a common challenge. Key areas to focus on include:
- Nanoparticle Synthesis Standardization: Ensure highly reproducible synthesis of the SERS-active nanoparticles (e.g., Ag Nanoflowers - AgNFs). Precisely control reaction parameters like temperature, time, and reagent concentrations. For AgNFs, using a one-pot synthesis with ethanol and sodium citrate at a controlled temperature of 50°C has been shown to produce a high enhancement factor of 2.8 × 10⁸ [43].
- Consistent Conjugation: Standardize the protocols for conjugating antibodies and Raman reporter molecules to the nanoparticle surface.
- Membrane Spotting: Optimize and control the dispensing process for both the capture antibody and the internal standard nanoparticles on the test line to ensure consistent loading and distribution [44].
Q3: The sensitivity of my biosensor is lower than expected when testing complex samples like blood plasma. How can I enhance its performance?
To improve sensitivity in complex matrices:
- Optimize the SERS Substrate: Utilize nanoparticles with high enhancement factors, such as the developed Ag Nanoflowers, which provide superior signal amplification [43].
- Employ a Robust Self-Calibration Method: The internal standard corrects for signal suppression caused by sample matrix interference, effectively restoring the assay's sensitivity and ensuring accurate quantification [45].
- Introduce a Washing Step: A gentle washing step after the sample has flowed through the strip can remove unbound substances and residual sample matrix that might contribute to background noise [46].
Research Reagent Solutions
Table 1: Essential Materials for Self-Calibrating SERS-LFIA Biosensor Construction
| Reagent/Material | Function in the Biosensor | Research Context & Examples |
|---|---|---|
| Ag Nanoflowers (AgNFs) | SERS-active substrate providing high signal enhancement (AEF of 2.8 × 10⁸) for ultra-sensitive detection [43]. | Synthesized via a one-pot method using AgNO₃, ethanol, sodium citrate, and ascorbic acid [43]. |
| Raman Reporter Molecule (e.g., MBA) | A molecule that generates a unique, intense SERS fingerprint signal; it is adsorbed onto the metal nanoparticle surface [43]. | Used to functionalize AgNFs; its characteristic peaks are used for quantification [43]. |
| Capture & Detection Antibodies | Provide immunological specificity for the target analyte (e.g., PEAK1, Aβ1-42) [43] [44]. | Immobilized on the test line (capture) and conjugated to SERS nanoprobes (detection). |
| Internal Standard (IS) Nanoparticles | Embedded in the test line to provide a stable calibration signal, correcting for fluctuations and enabling ratiometric quantification [45] [44]. | Can be SERS nanoparticles with a distinct Raman signature that does not overlap with the reporter [44]. |
| Nitrocellulose (NC) Membrane | The porous matrix that constitutes the lateral flow strip, where immunochromatography occurs [43]. | Its properties can cause signal fluctuation, which the self-calibration design specifically mitigates [44]. |
Experimental Protocol: Constructing a Self-Calibrating SERS-LFIA Biosensor
1. Synthesis of SERS Nanoparticles (Ag Nanoflowers):
- Add 40 mg of AgNO₃ to 20 mL of 50% ethanol aqueous solution.
- Introduce 150 mg of sodium citrate and react for 50 minutes at 50°C.
- Add 80 mg of ascorbic acid as a reducing agent at room temperature and let the reaction proceed for 30 minutes.
- Centrifuge the resulting AgNFs and re-suspend in deionized water. Characterize the nanoparticles using SEM and UV-Vis spectroscopy [43].
2. Preparation of SERS Nanoprobes:
- Activate the AgNF surface.
- Incubate the AgNFs with the Raman reporter molecule (e.g., 4-Mercaptobenzoic acid - MBA) to form a self-assembled monolayer.
- Conjugate specific detection antibodies to the reporter-coated AgNFs using a cross-linker like EDC/NHS. Purify the resulting nanoprobes and store them in a suitable buffer [43].
3. Fabrication of the Self-Calibrating Lateral Flow Strip:
- Sample Pad: Pre-treat the pad to ensure optimal sample flow and particle release.
- Conjugation Pad: Disperse and dry the SERS nanoprobes onto this pad.
- NC Membrane: Use an automated dispenser to create two lines:
- Test Line (T): Spot a solution containing both the capture antibody and the internal standard (IS) nanoparticles.
- Control Line (C): Spot a secondary antibody to capture excess nanoprobes.
- Absorption Pad: Assemble at the end of the strip to wick the fluid and maintain continuous flow [43] [44].
4. Assay Procedure and SERS Detection:
- Apply the liquid sample to the sample pad.
- Allow the assay to develop, typically for 10-15 minutes, as the sample migrates via capillary action.
- Place the dry strip under a Raman spectrometer.
- Focus the laser on the test line and collect SERS spectra.
- Quantify the target analyte by calculating the ratio of the Raman reporter peak intensity to the internal standard peak intensity [43] [45].
Diagram 1: Workflow of a self-calibrating SERS-LFIA biosensor, showing the integration of the internal standard for ratiometric analysis.
Performance Data of Self-Calibrating SERS-LFIA Platforms
Table 2: Analytical Performance of Documented Self-Calibrating SERS-LFIA Biosensors
| Target Analyte | Biosensor Design Key Feature | Limit of Detection (LOD) | Linear Range | Reported Applications |
|---|---|---|---|---|
| PEAK1 Kinase | AgNF nanoprobes; C dot as calibration unit [43]. | 1 fg/mL | 1 fg/mL ~ 0.1 μg/mL | Detection in spiked plasma and cellular contents [43]. |
| Amyloid-β (Aβ1-42) | Internal Standard (IS)-SERS nanoparticles embedded in the test line [45] [44]. | Not explicitly stated | Not explicitly stated | Detection in biofluids for Alzheimer's disease diagnosis [45] [44]. |
Diagram 2: Logical comparison demonstrating how a self-calibrating design corrects for signal fluctuations to yield reliable results.
Dynamic Regulation and Computer-in-the-Loop Calibration Systems
Frequently Asked Questions (FAQs)
Q1: What is dynamic regulation in metabolic engineering, and why is it superior to static optimization? Dynamic regulation uses genetic circuits to enable engineered cell factories to automatically sense and respond to fluctuating internal and environmental conditions [47]. Unlike static optimization, which fixes gene expression at a constant level, dynamic control improves robustness, scalability, and stability during industrial bioproduction, where nutrient levels, pH, and oxygen can vary [47]. This is crucial for maintaining high pathway efficiency and yield in large-scale fermenters.
Q2: What are the key performance metrics I should characterize for a genetic biosensor? When characterizing a biosensor, you should evaluate both its steady-state and dynamic performance metrics [47]. Key parameters are summarized in the table below.
Table 1: Key Performance Metrics for Genetic Biosensors
| Metric | Description | Impact on Performance |
|---|---|---|
| Dynamic Range | Span between minimal and maximal detectable signal [47]. | Determines the breadth of metabolite concentrations the biosensor can detect. |
| Operating Range | Concentration window for optimal biosensor performance [47]. | Defines the practical, linear range for sensing. |
| Response Time | Speed at which the biosensor reacts to a change in the target [47]. | Slow response hinders real-time control and can introduce delays. |
| Signal-to-Noise Ratio | Clarity and reliability of the output signal [47]. | High noise can obscure true concentration differences, reducing resolution. |
| Sensitivity | The minimal change in input required to produce a detectable change in output [47]. | Determines the biosensor's ability to detect small concentration variations. |
Q3: My biosensor performance varies significantly between different growth media. How can I address this context dependency? Biosensor behavior is highly dependent on the environmental context, including the growth medium, carbon source, and supplements [48]. To address this:
- Systematic Characterization: Test your biosensor construct across a matrix of the media and conditions you intend to use, as the metabolic state of the cell directly impacts RNA and protein production rates [48].
- Adopt a DBTL Cycle: Use a Design-Build-Test-Learn (DBTL) pipeline. Build a library of biosensors with varied genetic parts (promoters, RBS), characterize them under different conditions, and use machine learning to build a predictive model for optimal biosensor selection [48].
Q4: What is a "computer-in-the-loop" system, and how can it be applied to biosensor calibration? A "computer-in-the-loop" system uses real-time data and computational models to autonomously control or calibrate a biological process. This involves:
- Error Compensation: A machine learning model (e.g., a neural network) is trained to predict the error between a fast, lower-fidelity simulation (the digital twin) and real-world measurements. The model then calibrates the digital twin's outputs in real-time to match reality [49].
- Dynamic Updates: The calibration model can be continuously updated with incoming real-time data, allowing the system to adapt to new states and correct for error accumulation over time [49].
Troubleshooting Guides
Issue 1: High Signal Noise in Biosensor Output
Potential Causes:
- Cellular Context: High inherent stochasticity in gene expression, which can be influenced by the choice of genetic parts and growth conditions [47] [48].
- Sensor Design: Non-optimal biosensor design with poor signal amplification or low-affinity ligand binding [47].
Solutions:
- Tune Genetic Parts: Engineer the biosensor by swapping promoters and ribosome binding sites (RBS) to tune expression levels and improve the signal-to-noise ratio [47].
- Utilize High-Throughput Screening: Use cell sorting combined with directed evolution to screen for mutant biosensors with improved specificity and lower noise [47].
- Filtering: Apply computational filters or moving averages to the output data stream in your computer-in-the-loop system to smooth transient noise [49].
Issue 2: Slow Biosensor Response Time Affecting Real-Time Control
Potential Causes:
- Inherently Slow System: The biosensor may be based on components (e.g., certain transcription factors) with slow transcription and translation kinetics [47].
Solutions:
- Adopt Hybrid Systems: Combine slower, stable systems with faster-acting components, such as riboswitches or toehold switches, to improve overall response speed [47].
- Model-Predictive Control: Implement an algorithm that uses a dynamic model of your biosensor to predict its future state, allowing the control system to pre-emptively compensate for delays [47].
Issue 3: Poor Calibration Accuracy and Drift in Computer-in-the-Loop System
Potential Causes:
- Model-Plant Mismatch: The digital twin or computational model does not accurately represent the real biological system, leading to systematic errors [49].
- Non-Stationary Process: The system being calibrated drifts over time due to factors like cell aging or sensor degradation, which the initial calibration model cannot account for [49].
Solutions:
- Implement Dynamic Training: Use a two-stage calibration process. In the offline stage, build an initial error database and calibration model. In the online stage, continuously update the error database and recalibrate the model in real-time as new data streams in [49].
- Physics-Informed Machine Learning: Embed prior knowledge of the system's physics (e.g., mass balance, reaction kinetics) into the machine learning model to improve its extrapolation capability and robustness [49].
Experimental Protocols
Protocol 1: Characterizing a Transcription Factor-Based Biosensor
This protocol outlines the steps to obtain a dose-response curve for a TF-based biosensor.
1. Research Reagent Solutions Table 2: Essential Reagents for Biosensor Characterization
| Reagent / Material | Function |
|---|---|
| Biosensor Construct | Plasmid containing the TF and its operator/promoter fused to a reporter gene (e.g., GFP). |
| Inducer Molecule | The target metabolite or a mimic that activates the TF (e.g., Naringenin for FdeR-based sensors) [48]. |
| Culture Media & Supplements | Various media (e.g., M9, SOB) and carbon sources (e.g., Glucose, Glycerol) to test context-dependency [48]. |
| Microplate Reader | Instrument for measuring optical density (cell growth) and fluorescence (reporter output) in a high-throughput manner. |
2. Methodology
- Day 1: Inoculation. Transform the biosensor plasmid into your microbial chassis (e.g., E. coli). Pick a single colony to inoculate a small starter culture and grow overnight.
- Day 2: Dose-Response Experiment.
- Dilute the overnight culture into fresh medium in a 96-well plate.
- Add a range of inducer concentrations to the wells. Include a negative control (no inducer) and a blank (medium only).
- Place the plate in a microplate reader and incubate at the appropriate temperature.
- Measure the optical density (OD600) and fluorescence (e.g., Ex/Em for GFP) at regular intervals (e.g., every 10-30 minutes) over 6-24 hours.
- Day 3: Data Analysis.
- Normalize the fluorescence signal by the OD600 to account for cell density.
- Plot the normalized fluorescence (Y-axis) against the inducer concentration (X-axis) at a fixed time point (for steady-state) or over time (for dynamics).
- Fit a sigmoidal curve to the data to extract the dynamic range, EC50, and sensitivity [47] [48].
Protocol 2: Implementing a Computer-in-the-Loop Calibration for a Bioreactor Process
This protocol describes a machine learning-based calibration for a digital twin of a fermentation process.
1. Research Reagent Solutions
- Digital Twin: A real-time capable simulation of your bioprocess (e.g., a simplified metabolic model or a thermal-hydraulic system code for a reactor) [49].
- Data Acquisition System: Sensors to measure real-time process variables (e.g., pH, dissolved O2, metabolite concentration via inline biosensors).
- Computing Infrastructure: A computer with sufficient processing power to run the digital twin and machine learning model in parallel with the real process.
2. Methodology
- Offline Stage (Pre-experiment):
- Build Error Database: Run your digital twin under a wide range of possible operating conditions. Collect the simulated data and the corresponding measurement data (or high-fidelity data) to build a database of errors [49].
- Train Calibration Model: Use the error database to train a machine learning model (e.g., a neural network) to predict the error based on the digital twin's outputs [49].
- Online Stage (During the experiment):
- Parallel Operation: Run the digital twin in parallel with the real bioreactor, feeding it the same control inputs.
- Real-Time Calibration: Stream the real sensor data and the digital twin's outputs. Use the trained ML model to predict the current error and calibrate the digital twin's outputs:
Calibrated Value = Digital Twin Output + Predicted Error[49]. - Dynamic Update (Optional): Continuously add new data points to the error database and periodically retrain the ML model to adapt to process drift [49].
Visualizations
Diagram 1: Computer-in-the-Loop Calibration Workflow
Computer-in-the-Loop Calibration System
Diagram 2: Biosensor-Enabled Dynamic Regulation Circuit
Biosensor Dynamic Regulation Circuit
Multi-Analyte Calibration Strategies for Complex Biological Samples
Frequently Asked Questions (FAQs)
Q1: What are the main challenges in preparing calibrators for multi-analyte methods? Manually preparing spiking solutions containing a great number of analytes is tedious, time-consuming, and prone to error. This process can be difficult to maintain with sufficient robustness in the laboratory, especially when combining analytes with different physicochemical properties and required calibration ranges [50].
Q2: Can the calibration process be automated? Yes, autosampler-assisted automated preparation of calibrator spiking solutions has been demonstrated to be a viable alternative. This approach has proven comparable to manual preparation in terms of results, while overcoming the manual, error-prone steps and still allowing for customized calibration ranges [50].
Q3: How can I handle compounds with vastly different concentrations in a single run? Compromises are needed between sensitivity and avoiding saturation effects. Strategies include using less optimal MS settings or the integration of ¹³C-labeled internal standards. A suitable chromatographic separation is also crucial to reduce mutual suppression effects of co-eluting substances, particularly when using electrospray ionization (ESI) [50].
Q4: What validation criteria should a multi-analyte method meet? Method validation should be performed according to international guidelines. Parameters typically include selectivity, recovery, matrix effects, linearity, bias/imprecision, processed-sample stability, and the determination of limits of quantification. It is common for a small number of analytes (e.g., buprenorphine and some benzodiazepines) to not fulfill all validation criteria [50].
Troubleshooting Guide
| Problem Area | Specific Issue | Possible Causes | Recommended Solutions |
|---|---|---|---|
| Calibration & Data | Inaccurate quantification/Calibration drift | • Improper calibrator preparation • Infrequent calibration • Instrument drift • Unstable calibration solutions | • Implement automated calibrator preparation [50] • Calibrate regularly with fresh standards • Verify calibration with control samples [5] |
| Sensor & Sample | Low sensitivity for certain analytes | • High mutual suppression from co-eluting compounds • Suboptimal MS settings • Saturation effects | • Improve chromatographic separation [50] • Use ¹³C-labeled internal standards [50] • Adjust MS parameters for lower/higher concentration analytes [50] |
| Signal interference/Noise | • Matrix effects from complex sample • Contaminated sensor or buffer • Non-specific binding | • Use simple protein precipitation [50] • Inspect and clean sensor; replace if damaged [5] • Use fresh, matching buffer solutions [5] | |
| Method Performance | Validation criteria not met for some analytes | • Compound-specific instability • Inefficient extraction • Inherent physicochemical properties | • Modify sample preparation (e.g., enzymatic hydrolysis for conjugates) [50] • Accept a validated narrower range for problematic analytes |
Experimental Protocols & Workflows
Detailed Methodology: LC-MS/MS Multi-Analyte Quantification in Whole Blood
This protocol is adapted from a validated approach for 82 classic drugs [50].
1. Sample Preparation (Protein Precipitation):
- Pipette 200 µL of whole blood into a tube.
- Add 50 µL of the deuterated internal standard (IS) mixture.
- Add 50 µL of methanol (for consistency with calibrators).
- Slowly add 400 µL of acetonitrile under continuous vortexing.
- Shake the mixture vigorously for 10 minutes at 1400 rpm.
- Centrifuge for 10 minutes at 10,000 rpm.
- Transfer 250 µL of the supernatant to a new tube and add 10 µL of formic acid.
- Evaporate the mixture to dryness under a gentle stream of nitrogen at room temperature.
- Reconstitute the dry residue in 300 µL of a mixture of Mobile Phases A and B (95:5, v/v).
2. Liquid Chromatography (LC):
- Column: Phenomenex Kinetex PS C18 (100 x 2.1 mm, 2.6 µm).
- Mobile Phase A: 10 mM ammonium formate buffer in water with 0.1% (v/v) formic acid (pH 3.5).
- Mobile Phase B: Acetonitrile.
- Elution: Gradient elution.
- Injection Volume: 5-10 µL.
3. Mass Spectrometry (MS/MS):
- Detection: Tandem mass spectrometry with electrospray ionization (ESI).
- Mode: Advanced scheduled Multiple Reaction Monitoring (MRM).
Workflow: Automated Calibrator Preparation
The following diagram illustrates the automated workflow for preparing multi-analyte calibrators, which reduces manual error and saves time.
Research Reagent Solutions
The table below lists key materials and reagents used in the featured multi-analyte LC-MS/MS experiment, along with their specific functions [50].
| Reagent / Material | Function / Specification |
|---|---|
| Drug & Metabolite Standards | Reference analytes for identification and quantification; typically supplied as 0.1 or 1 mg/mL solutions in methanol or acetonitrile. |
| Deuterated Internal Standards (IS) | Correct for variability in sample preparation and ionization; added to all samples, calibrators, and quality controls before extraction. |
| Acetonitrile (HPLC Grade) | Organic solvent for protein precipitation, denaturing and removing proteins from the biological matrix. |
| Ammonium Formate Buffer | Mobile phase additive (with formic acid) to control pH and improve ionization efficiency in the mass spectrometer. |
| Formic Acid | Acidifying agent added to the supernatant after precipitation to stabilize analytes and aid in evaporation. |
| β-Glucuronidase (H. pomatia) | Enzyme for hydrolyzing drug-glucuronide conjugates in urine samples prior to extraction, freeing the parent drug for measurement. |
TABLE: Key Validation Parameters from an 82-Analyte LC-MS/MS Method [50]
| Validation Parameter | Summary of Results |
|---|---|
| Analytes Validated | 82 classic drugs (stimulants, opioids, benzodiazepines, antidepressants, neuroleptics, antihistamines) |
| Successful Validation | 76 out of 82 analytes met all pre-defined validation criteria. |
| Analytes with Issues | Buprenorphine and five benzodiazepines did not fulfill all validation criteria. |
| Sample Volume | 200 µL of whole blood. |
| Sample Prep Technique | Simple protein precipitation. |
| Application in Practice | >8,000 real cases measured and 35 proficiency tests successfully passed since method implementation. |
Overcoming Calibration Challenges in Complex Environments
Addressing Signal Interference and Matrix Effects in Biological Samples
FAQs: Understanding and Identifying Interference
What are the most common sources of signal interference in biosensors? Signal interference in biosensors typically originates from three main categories:
- Electronic Noise: This includes thermal (Johnson-Nyquist) noise from random charge carrier motion and 1/f (flicker) noise from electrode material imperfections, which is especially prevalent at low frequencies [51].
- Environmental Interference: Electromagnetic interference (EMI) from power lines or wireless devices can capacitively or inductively couple into the sensor system, causing baseline fluctuations [51].
- Biological Matrix Effects: Complex biological samples (serum, blood, saliva) can cause non-specific binding, biofouling, or alter the local chemical environment (pH, ionic strength), leading to false positives/negatives [51] [52] [53].
How can I determine if signal drift is from my sensor or the sample itself? First, establish a controlled baseline by testing your sensor in a simple, known buffer (e.g., PBS). If drift persists, the issue is likely sensor-related (e.g., biofouling, unstable electrode). If drift only occurs with the biological sample, matrix effects are the probable cause. Visually inspect the sensor for damage, air bubbles, or debris, and ensure proper calibration in a clean matrix before testing complex samples [54].
Why does my biosensor perform well in buffer but poorly in serum? Biological fluids like serum have a complex composition that can inhibit sensor function. Serum and plasma have been shown to inhibit cell-free protein production by over 98%, primarily due to RNase activity. Other factors include variable ionic strength that causes Debye screening, pH fluctuations, and the presence of proteases or autofluorescent compounds that interfere with optical detection [35] [53].
Troubleshooting Guides
Guide 1: Troubleshooting Electrochemical Biosensor Drift
Electrochemical biosensors are highly susceptible to drift from various sources. The following flowchart outlines a systematic diagnostic pathway.
Guide 2: Mitigating Matrix Effects in Complex Samples
Matrix effects pose a significant challenge for biosensing in real biological samples. The workflow below details key strategies to counteract these effects.
Experimental Protocols
Protocol 1: Validating Biosensor Performance Across pH and Ionic Strength
Purpose: To systematically evaluate and calibrate a biosensor's resilience to variable sample conditions [52] [35].
Materials:
- Fully functional biosensor
- Target analyte at known concentration
- Stock buffer solutions (e.g., PBS, HEPES)
- HCl and NaOH solutions for pH adjustment
- Salt solutions (e.g., NaCl, KCl) for ionic strength adjustment
- pH meter
- Data acquisition system
Procedure:
- Prepare Sample Matrixes:
- Create a series of buffers with pH values ranging from 4.0 to 10.0, using HCl/NaOH for adjustment.
- In a separate series, create buffers with ionic strengths from 0.01 M to 1.0 M using NaCl or KCl.
- Spike each buffer with an identical, known concentration of your target analyte.
Run Measurements:
- For each pH and ionic strength condition, measure the sensor response to the spiked analyte.
- Perform each measurement in at least triplicate.
- Record the output signal (e.g., current, voltage, fluorescence intensity) for each condition.
Data Analysis:
- Plot the sensor response versus pH and versus ionic strength.
- Identify the range over which the sensor response is stable (less than 10% variation is typically acceptable).
- The sensor is suitable for samples falling within the identified stable ranges. For samples outside this range, pre-adjustment of sample pH/ionic strength is necessary.
Protocol 2: Implementing a Ratiometric Self-Calibration for SERS-Based Detection
Purpose: To correct for signal fluctuations in complex samples using an internal calibration standard, as demonstrated for protein kinase detection [43].
Materials:
- SERS-active nanoparticles (e.g., Ag nanoflowers - AgNFs)
- Raman reporter molecule (e.g., 4-Mercaptobenzoic acid - MBA)
- Specific capture and detection antibodies for your target
- Nitrocellulose (NC) membrane test strip with Test (T) and Control (C) lines
- Raman spectrometer
Procedure:
- SERS Nanoprobe Preparation:
- Synthesize or acquire AgNFs.
- Conjugate the Raman reporter molecule (MBA) to the AgNF surface.
- Link the detection antibody against your target to the AgNF-MBA complex.
Assay Assembly and Execution:
- Apply the SERS nanoprobe to the conjugation pad of the lateral flow strip.
- Apply the capture antibody to the T line of the NC membrane.
- Apply a control antibody (e.g., anti-species IgG) to the C line.
- Apply the sample to the sample pad and allow it to migrate.
Reading and Data Processing:
- Use a Raman spectrometer to measure the SERS intensity at both the T line (IT) and the C line (IC).
- The target concentration is proportional to the ratiometric signal (IT / IC).
- Use a calibration curve generated from standards of known concentration to convert the ratiometric signal to a quantitative value.
Data Presentation: Biosensor Performance Comparison
Table 1: Comparison of Advanced Biosensing Platforms for Complex Sample Analysis
| Biosensor Technology | Detection Principle | Key Feature for Mitigating Interference | Reported Limit of Detection (LoD) | Linear Dynamic Range | Performance in Complex Matrices |
|---|---|---|---|---|---|
| Magnetic Nanosensor (GMR) [35] | Magnetic field detection | Matrix-insensitive magnetic transduction | 50 aM (after amplification) | 6 orders of magnitude | Virtually identical performance in PBS, serum, urine, and saliva |
| Self-calibrated SERS-LFIA [43] | Surface-Enhanced Raman Scattering | Internal calibration using C dot signal | 1 fg/mL for PEAK1 protein | 1 fg/mL ~ 0.1 μg/mL | Successful detection in cell lysates and plasma |
| Ratiometric Fluorescent Biosensor [6] | Fluorescence | Dual-emission self-calibration | 36 pM for H₂S | 0.5-100 nM and 0.5-4.0 μM | 99.7-103% recovery in beer and milk |
| Electrolyte-Gated Graphene FET (EGGFET) [52] | Field-effect transistor | Multi-channel design for in-situ calibration | ~2 nM for Human IgG | 2–50 nM | Coefficient of variation <20% for IgG detection in serum |
Table 2: Common Interference Sources and Their Mitigation Strategies
| Interference Type | Impact on Biosensor | Effective Mitigation Strategies | Key References |
|---|---|---|---|
| Biofouling | Non-specific adsorption of proteins/cells, reducing signal and sensitivity | Antifouling coatings (PEG, BSA/prGOx/GA); Use of innate antifouling carbon nanomaterials | [51] |
| Variable Ionic Strength | Debye screening, masking charge-based binding events | Use magnetic nanosensors; Sample pre-dilution/desalting; Ratiometric calibration | [52] [35] |
| RNase Contamination | Degradation of RNA-based components in cell-free systems | Addition of RNase inhibitors (ensure glycerol-free buffers); Use of engineered strains producing RNase inhibitor | [53] |
| pH Fluctuations | Alters charge states and binding affinity, causing signal drift | Use of pH-insensitive sensors (e.g., magnetic); Sample pre-adjustment; Incorporation of internal calibration | [54] [35] |
| Electromagnetic Interference (EMI) | Introduces electronic noise, leading to signal fluctuations | Shielding of electronics; Calibration away from heavy machinery/power lines | [51] [54] |
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Reagents for Mitigating Biosensor Interference
| Reagent/Material | Function | Example Application/Note |
|---|---|---|
| Polyethylene Glycol (PEG) | Antifouling polymer coating | Reduces non-specific protein adsorption on sensor surfaces [51] |
| RNase Inhibitor | Protects RNA components from degradation | Critical for cell-free biosensors in clinical samples; avoid glycerol-containing buffers [53] |
| Carbon Nanomaterials | Transducer material with high surface area and conductivity | Provides innate antifouling properties and reduces electronic noise [51] |
| Magnetic Nanoparticles | Magnetic labels for detection | Enable matrix-insensitive detection in GMR sensors [35] |
| Ag Nanoflowers (AgNF) | SERS substrate for signal amplification | High enhancement factor (2.8 × 10⁸) for ultra-sensitive detection [43] |
| Dual-Junction Reference Electrode | Stable reference potential for electrochemical sensors | Reduces precipitate formation and drift in complex samples [54] |
Strategies for Improving Signal-to-Noise Ratio at Ultralow Concentrations
Troubleshooting Guides
Guide 1: Addressing Low Signal-to-Noise Ratio (SNR) in Biosensor Measurements
Problem: Measured signals from target analytes at ultralow concentrations are only marginally higher than the intrinsic electronic and environmental background noise, leading to poor signal clarity and unreliable data.
Why this happens:
- The fundamental charge noise in the sensor's system becomes significant compared to the faint signal from a low concentration of analyte [55] [56].
- In nanoscale transistors, the presence of even a single oxide trap can cause large discrete fluctuations known as Random-Telegraph-Signal (RTS) noise, which can overwhelm the signal [56].
- Chemical noise from the sample matrix can be a dominant noise source in complex samples, which is not present in clean buffer tests [57].
Solutions:
- Optimize Sensor Design and Electronics:
- Use low-noise amplifiers and shielded circuitry to reduce electrical interference [55].
- For transistor-based biosensors, consider scaling down the gate area, as the input-referred voltage noise (a key determinant of detection limit) scales inversely with gate area [56].
- P-type transistors may, in some cases, offer lower noise than N-type due to differences in trap interactions, though this is not universal at the nanoscale [56].
Apply Signal Processing Techniques:
Employ Signal Amplification Strategies:
- Integrate biochemical amplification methods like Rolling Circle Amplification (RCA). This technique creates long, repetitive DNA strands upon target recognition, significantly enhancing the electronic response of biosensors such as silicon nanowire field-effect transistors (SiNW-FETs) [58].
Leverage Single-Entity and Digital Sensing:
- For sensors capable of single-entity detection, implement a "digital sensing" approach using large arrays of independently addressable sensors. This allows for the counting of individual binding events, which eliminates the impact of baseline drift and converts the challenge of measuring a small analog signal into the more robust task of event counting [59].
Guide 2: Managing Cross-Interference and Selectivity in Complex Samples
Problem: The sensor responds to non-target molecules or background components in the sample, leading to false positives and inaccurate concentration readings at trace levels.
Why this happens:
- Sensor receptors may have affinity for molecules structurally similar to the target analyte [55].
- In mass spectrometry-based detection, "chemical noise" from the sample matrix is a major contributor to the baseline noise if chromatography or mass spectrometry selectivity is inadequate [57].
Solutions:
- Enhance Chemical Selectivity:
- Utilize chemically selective coatings or membranes on the sensor surface to reduce interference from non-target substances [55].
- Employ tandem mass spectrometry (MS-MS). While it may reduce the absolute signal, MS-MS dramatically reduces chemical noise through its high selectivity, leading to a net improvement in the signal-to-noise ratio and a lower limit of detection for real samples [57].
Validate with Reference Methods:
- Correlate sensor outputs with independent, highly selective laboratory techniques like chromatography or mass spectrometry to confirm accuracy [55].
Optimize Assay Conditions:
- Fine-tune sensor parameters and buffer conditions to favor specific interactions between the biorecognition element and the target analyte [55].
Guide 3: Overcoming Mass Transport and Binding Kinetics Limitations
Problem: At ultralow concentrations, it takes an impractically long time for analyte molecules to diffuse to and bind with the miniaturized sensor's detection area.
Why this happens:
- The steady-state diffusive flux of analyte to a miniaturized detector is proportional to the detector's characteristic size. A smaller sensor has a lower total flux, meaning longer average waiting times between analyte arrivals [59].
- At concentrations much lower than the dissociation constant (KD), the probability of a receptor being occupied by an analyte at equilibrium is very small, making binding a rare event [59].
Solutions:
- Implement Parallelized Detection:
- Use large arrays of many single-entity detectors operating simultaneously. This overcomes the low flux limitation of a single small sensor by massively parallelizing the detection process, enabling a statistically significant number of binding events to be recorded in a reasonable time [59].
- Consider Active Transport:
- While not covered in the search results, techniques like electrophoresis or mixing can be explored to enhance analyte delivery to the sensor surface.
Frequently Asked Questions (FAQs)
FAQ 1: What is the difference between sensitivity and signal-to-noise ratio, and which is more important for detecting ultralow concentrations?
Sensitivity and SNR are related but distinct concepts. According to IUPAC, sensitivity is formally defined as the slope of the calibration curve (signal versus concentration) [57]. A steeper slope means a larger signal change for a given change in concentration. The Signal-to-Noise Ratio (SNR), however, is the ratio of the true signal amplitude to the standard deviation of the noise [60] [57].
For ultralow concentration detection, SNR is often the more critical metric. It is possible to have a system with high sensitivity (large signal change) but also very high noise, resulting in a poor SNR and an inability to reliably detect low concentrations. Conversely, a method like MS-MS might slightly reduce the absolute signal (lower sensitivity) but drastically reduce chemical noise, leading to a vastly improved SNR and a lower practical detection limit [57]. The limit of detection (LOD) is directly tied to SNR, typically requiring an SNR of 3 [57].
FAQ 2: How do I properly calculate the Signal-to-Noise Ratio for my chromatographic data?
A meaningful SNR calculation requires careful measurement. Regulatory bodies provide specific guidelines to prevent inflated results:
- The European Pharmacopoeia (EP) recommends measuring the baseline noise across a time window that is 20 times wider than the chromatographic peak's width at half height (W½) [57].
- The US Pharmacopeia (USP) defines SNR as
2H/hn, whereHis the peak height andhnis the peak-to-peak noise measured over a distance equal to at least five times the W½ on either side of the peak [57].
Avoid methods that scan the entire chromatogram for the quietest baseline region, as this does not represent the noise near the analyte peak and can artificially inflate the SNR [57].
FAQ 3: Can noise ever be useful in biosensing?
Surprisingly, yes. In nanoscale biosensors where noise is dominated by a single trap causing RTS noise, the trapping and detrapping of individual charges can be monitored. By analyzing the statistics of this process (the trap occupancy probability), it is possible to suppress noise beyond the conventional thermal limit, in an approach analogous to stochastic resonance found in biological systems [56]. In this context, the "noise" becomes the signal that is analyzed.
FAQ 4: What are the biggest challenges when calibrating sensors for ultralow-level detection?
The primary challenges are [55]:
- Low SNR: Distinguishing the faint analyte signal from system noise.
- Cross-Interference: Ensuring the sensor responds only to the target analyte.
- Contamination: Even minute contaminants can overwhelm the target signal; using inert materials like PTFE and cleanroom protocols is essential.
- Reference Standard Accuracy: Producing and maintaining reliable calibration standards at parts-per-billion (ppb) or parts-per-trillion (ppt) levels is difficult.
- Environmental Sensitivity: Tiny fluctuations in temperature and humidity can cause significant sensor drift.
Experimental Protocols
Protocol: Enhancing SNR for DNA Detection via Rolling Circle Amplification on a Silicon Nanowire Biosensor
This protocol is adapted from research demonstrating a detection limit of 50 attomolar (aM) for DNA by combining the sensitivity of a silicon nanowire field-effect transistor (SiNW-FET) with the signal amplification of RCA [58].
1. Sensor Fabrication:
- Fabricate highly responsive SiNWs using a complementary metal oxide semiconductor (CMOS) compatible anisotropic self-stop etching technique [58].
2. Functionalization:
- Immobilize probe DNA sequences on the surface of the silicon nanowire.
3. Hybridization and RCA Assembly:
- Incubate the functionalized sensor with a sample containing the perfectly matched target DNA.
- Simultaneously, hybridize an RCA primer to the target DNA. This primer is designed to also hybridize with a circular RCA template.
4. Signal Amplification:
- Initiate the Rolling Circle Amplification reaction. Using the circular template, a DNA polymerase enzyme synthesizes a long, single-stranded DNA (ssDNA) product consisting of hundreds of tandem repeats complementary to the circle [58].
- This long, highly negatively charged DNA product binds to the sensor surface, creating a significant change in surface charge.
5. Measurement and Analysis:
- Measure the conductance change of the SiNW-FET. The massive molecular weight and charge of the RCA product induce a strong electronic signal.
- Analyze the signal-to-noise ratio. This method has been shown to achieve an SNR of >20 for 1 femtomolar (fM) DNA, enabling discrimination of perfectly matched DNA from single-base mismatches [58].
Workflow Diagram: RCA-Based DNA Detection on a Nanowire Sensor
Key Research Reagent Solutions
Table: Essential Materials for Ultralow Concentration Biosensing
| Research Reagent / Material | Function in Experiment |
|---|---|
| Silicon Nanowire Field-Effect Transistors (SiNW-FETs) | The core transducer. Its conductance is exquisitely sensitive to surface charge changes, enabling label-free detection of biomolecular binding events [58] [61]. |
| Rolling Circle Amplification (RCA) Kit | A biochemical signal amplification tool. It exponentially increases the mass and charge bound to the sensor upon target recognition, dramatically boosting the signal output for nucleic acid detection [58]. |
| NIST-Traceable Calibration Standards | Certified reference materials used to calibrate sensors accurately at parts-per-billion (ppb) or parts-per-trillion (ppt) levels, ensuring measurement traceability and validity [55]. |
| Selective Membrane/Chemical Coatings | Materials applied to the sensor surface to improve specificity. They reduce non-specific binding and interference from background molecules in complex samples [55]. |
| High-k Dielectric Materials | Used in nanotransistor gates. These materials have higher dielectric constants, which can lead to larger signal amplitudes from single trapping events and lower dielectric polarization noise, improving SNR [56]. |
| Inert Flow System Materials (e.g., PTFE, Stainless Steel) | Used to construct fluidic paths for sample and standard delivery. Their inertness minimizes the sorption of target analytes and introduction of contaminants, which is critical for maintaining sample integrity at ultralow concentrations [55]. |
Table: Noise and Performance Characteristics of Different Biosensor Platforms
| Sensor Platform / Technique | Key Performance Metric | Reported Value / Scaling Law | Key Factors Influencing Performance |
|---|---|---|---|
| SiNW-FET with RCA [58] | Detection Limit (DNA) | 50 aM (attomolar) | Specificity of probe DNA, length of RCA product. Achieves SNR >20 at 1 fM. |
| Generic FET-based Biosensor [56] | Input-Referred Voltage Noise (S_VG) | Scales with 1 / (Gate Area A) |
Gate area (A), oxide trap density (Not), gate capacitance (CG). |
| Generic FET-based Biosensor [56] | Charge Noise (S_q) | Scales with Gate Area A |
Gate area (A), dielectric loss tangent (tgδ). |
| Nanotransistor with Single Trap (RTS Noise) [56] | RTS Noise Amplitude | Scales with 1 / (C_G × A)^2 |
Gate capacitance (C_G), gate area (A), effective charge (q*). |
| Dielectric Polarization (DP) Noise [56] | Charge Noise (S_q) | (2kT tgδ C_G A) / (π f) |
Temperature (T), dielectric loss (tgδ), capacitance (C_G), area (A), frequency (f). |
Diagram: Noise Scaling Laws in Nanotransistor Biosensors
Frequently Asked Questions (FAQs)
FAQ 1: What are the most common sources of interference in electrochemical biosensors? The most common sources of interference can be categorized into three main types [51]:
- Redox-Active Interferences: Species present in biological media (e.g., ascorbic acid, uric acid, acetaminophen) that are electrochemically active at the sensor's operating potential, generating a false positive signal [62].
- Biological Fouling: The non-specific adsorption of proteins, cells, or other biomolecules onto the sensor surface (biofouling). This can block the access of the target analyte to the biorecognition element and alter the transducer's properties [51] [63].
- Non-Specific Binding: Similar to fouling, this involves the weak, non-selective binding of non-target molecules to the biorecognition layer or transducer surface, reducing the sensor's specificity [63].
FAQ 2: My biosensor shows high background noise and reduced sensitivity in complex samples like serum. What strategies can I employ? This is a classic symptom of interference and fouling. A multi-pronged approach is recommended [51] [63]:
- Apply an Antifouling Coating: Surface modifications using polyethylene glycol (PEG), zwitterionic polymers, or polydopamine can create a hydration layer that physically repels biomolecules and reduces non-specific adsorption [63].
- Utilize Advanced Electrode Materials: Consider carbon nanomaterials that offer inherent antifouling properties, high conductivity, and a large active surface area, which can help reduce electronic noise and improve the signal-to-noise ratio [51].
- Implement a Physical Barrier: For electrochemical sensors, a conductive membrane can be used to encapsulate the sensor. This membrane can be held at a potential that electrochemically deactivates redox-active interferents before they reach the working electrode, while allowing the target analyte to pass through [62].
FAQ 3: How can I differentiate between signal drift caused by interferents and drift caused by bioreceptor degradation? A systematic troubleshooting protocol is essential:
- Run a Control in Analyte-Free Buffer: If the drift persists in a clean matrix, the issue is likely intrinsic to the sensor, such as bioreceptor instability or reference electrode drift.
- Spike a Known Interferent: Adding a common interferent (e.g., ascorbic acid) to the buffer. A significant signal change confirms susceptibility to that interferent.
- Check Calibration Curves Over Time: A consistent reduction in signal amplitude across all concentrations points to bioreceptor degradation or loss of activity. A rising baseline, especially in complex samples, is more indicative of fouling or interferent buildup [51].
FAQ 4: Are there computational tools to help design better anti-interference surfaces? Yes, Artificial Intelligence (AI) and Machine Learning (ML) are revolutionizing this area. AI models can analyze vast datasets to predict optimal surface architectures, material compositions, and bioreceptor configurations for maximizing selectivity and minimizing fouling. For instance, AI-guided molecular dynamics simulations can provide atomic-level insights into bioreceptor-substrate interactions and the effectiveness of antifouling coatings [63].
Troubleshooting Guides
Problem: High Background Signal in Complex Samples
Potential Cause 1: Redox-active interferents in the sample matrix. Solution:
- Use a Conductive Membrane: A recently demonstrated strategy involves encapsulating the sensor with three layers of gold-coated track-etch membranes. A potential is applied to these layers to electrochemically deactivate redox-active species. This method has shown a 72% reduction in redox-active interference and an 8-fold decrease in the detection limit for a model glucose oxidase sensor [62].
- Experimental Protocol for Conductive Membrane Integration:
- Fabricate or source porous track-etch membranes.
- Sputter-coat the membranes with a thin layer of gold to make them conductive.
- Stack and align three layers of the gold-coated membrane over the biosensor's working electrode.
- Encapsulate the assembly, ensuring electrical contact to each membrane layer.
- Apply an optimized potential to the membrane stack during measurement to pre-filter interferents while allowing the target analyte to diffuse to the sensor surface [62].
Potential Cause 2: Biofouling and non-specific binding on the transducer surface. Solution:
- Apply an Innate Antifouling Nanomaterial: Use electrode materials like certain carbon nanomaterials that possess inherent anti-biofouling properties. These materials prevent the adsorption of proteins and other biomolecules from complex matrices like blood or saliva without needing additional coatings that can slow down analyte access [51].
- Functionalize with Zwitterionic Coatings: Modify the sensor surface with zwitterionic polymers, which are highly effective at resisting non-specific protein adsorption due to their strong hydration layer [63].
Problem: Inconsistent Sensor Response and Poor Reproducibility
Potential Cause: Uncontrolled or random immobilization of bioreceptors (e.g., antibodies, enzymes), leading to inaccessible active sites and variable surface density. Solution:
- Implement Oriented Immobilization Strategies: Use advanced surface chemistry to ensure bioreceptors are attached in a consistent, oriented manner.
- For Antibodies: Utilize protein A/G or site-specific covalent binding via engineered tags.
- For Enzymes: Employ self-assembled monolayers (SAMs) with specific terminal functional groups (e.g., NHS esters) for controlled covalent attachment [63].
- Experimental Protocol for SAM-based Oriented Immobilization:
- Clean the gold electrode surface with piranha solution (Caution: highly corrosive) and oxygen plasma.
- Immerse the electrode in a 1 mM ethanol solution of a heterobifunctional thiol (e.g., COOH-terminated) for 24 hours to form a SAM.
- Rinse thoroughly with ethanol to remove physisorbed molecules.
- Activate the carboxyl groups by incubating with a mixture of EDC and NHS for 30-60 minutes.
- Expose the activated surface to the bioreceptor (e.g., antibody) in a suitable buffer (e.g., PBS, pH 7.4) for 2 hours.
- Finally, block any remaining active sites with a blocking agent like BSA or ethanolamine [63].
Performance Data of Mitigation Strategies
The table below summarizes quantitative data from recent studies on various interference mitigation strategies.
Table 1: Comparison of Cross-Interference Mitigation Strategies
| Mitigation Strategy | Target Interference | Key Performance Metric | Reported Improvement | Reference |
|---|---|---|---|---|
| Conductive Membrane Encapsulation | Redox-active species (e.g., ascorbate, urate) | Interference Reduction | 72% reduction | [62] |
| Conductive Membrane Encapsulation | Redox-active species | Limit of Detection (LoD) | 8-fold decrease | [62] |
| Carbon Nanomaterial Electrodes | Electronic Noise & Biofouling | Signal-to-Noise Ratio | Improved due to reduced thermal/flicker noise and innate antifouling | [51] |
| AI-Optimized Surface Functionalization | Non-specific Binding | Biosensor Sensitivity & Selectivity | Data-driven prediction of optimal surface architectures for enhanced performance | [63] |
| Engineered Allosteric Transcription Factors (aTFs) | Sample Matrix (in cell-free systems) | Limit of Detection for Hg2+ | 0.5 nM | [64] |
Experimental Protocols
Protocol 1: Mitigating Redox Interference with a Conductive Membrane
This protocol is adapted from a novel strategy designed to protect electrochemical biosensors [62].
- Materials:
- Polycarbonate track-etch membrane filters (e.g., 100 nm pore size).
- Sputter coater.
- Biosensor platform (e.g., screen-printed electrode).
- Potentiostat.
- Method:
- Membrane Preparation: Sputter-coat the track-etch membranes with a thin (e.g., 50 nm) layer of gold to ensure conductivity.
- Sensor Assembly: Stack three layers of the gold-coated membrane directly over the working electrode of the biosensor. Secure the assembly using a custom-designed cell that maintains electrical contact with each membrane layer.
- Electrical Connection: Connect each of the three membrane layers to the potentiostat. The biosensor's working electrode remains connected as usual.
- Electrochemical Measurement: In the measurement setup, apply a specific, optimized potential to the stack of conductive membranes. This potential is chosen to oxidize or reduce common redox-active interferents before they can reach the underlying biosensor. The target analyte, being redox-inactive at this potential, passes through the membrane unaltered and is detected at the working electrode.
- Validation:
- Perform calibration curves for the target analyte in a clean buffer with and without the membrane.
- Test sensor response in the presence of known concentrations of interferents (e.g., 0.1 mM ascorbic acid) to quantify the reduction in false signal.
Protocol 2: Enhancing Selectivity via Oriented Antibody Immobilization on SAMs
This is a standard protocol for improving immunosensor reproducibility and selectivity [63].
- Materials:
- Gold electrodes.
- 11-Mercaptoundecanoic acid (11-MUA) solution (1 mM in absolute ethanol).
- EDC (1-ethyl-3-(3-dimethylaminopropyl)carbodiimide) and NHS (N-hydroxysuccinimide), fresh prepared in MES buffer.
- Capture antibody solution (10-50 μg/mL in PBS, pH 7.4).
- Blocking solution (e.g., 1% BSA or 1 M ethanolamine, pH 8.5).
- Method:
- Surface Cleaning: Clean gold electrodes in a piranha solution (3:1 v/v H2SO4:H2O2) for 10 minutes, followed by rinsing with copious water and ethanol. (Warning: Piranha is extremely hazardous and must be handled with extreme care).
- SAM Formation: Incubate the clean electrodes in the 1 mM 11-MUA solution for 24 hours at room temperature. Rinse with ethanol and dry under a stream of nitrogen.
- Activation: Immerse the SAM-modified electrodes in a mixture of EDC (400 mM) and NHS (100 mM) in MES buffer (0.1 M, pH 5.5) for 30-60 minutes to activate the carboxyl groups to NHS esters. Rinse with MES buffer.
- Antibody Immobilization: Immediately incubate the activated electrodes with the antibody solution for 2 hours at room temperature.
- Blocking: Rinse the electrodes with PBS and then incubate in the blocking solution for 1 hour to deactivate any remaining NHS esters and prevent non-specific binding.
- Storage: The functionalized biosensors can be stored in PBS at 4°C until use.
Research Reagent Solutions Toolkit
Table 2: Essential Materials for Cross-Interference Mitigation Experiments
| Reagent/Material | Function | Example Application |
|---|---|---|
| Gold-coated Track-Etch Membranes | Conductive physical barrier for pre-filtering redox interferents. | Core component of the conductive membrane interference mitigation strategy [62]. |
| Carbon Nanomaterials (e.g., Gii) | Electrode material with high conductivity and innate antifouling properties. | Used to fabricate transducers that minimize biofouling in complex samples like serum and saliva [51]. |
| Zwitterionic Polymers (e.g., PSB) | Forms a super-hydrophilic coating that resists protein adsorption. | Applied as an antifouling layer on sensor surfaces to mitigate non-specific binding [63]. |
| Heterobifunctional Thiols (e.g., 11-MUA) | Forms a self-assembled monolayer (SAM) on gold for controlled surface chemistry. | Creates a functional interface for the oriented immobilization of bioreceptors [63]. |
| EDC and NHS Cross-linkers | Activates carboxyl groups for covalent coupling to amine groups. | Used to link bioreceptors (antibodies, enzymes) to activated SAMs or other functionalized surfaces [63]. |
Experimental Workflow and System Diagrams
The following diagrams illustrate the core mechanisms of the mitigation strategies discussed.
Conductive Membrane Interference Filtering
Surface Engineering for Selective Sensing
Optimization of Dynamic Range and Response Time Through Genetic Circuit Engineering
In the field of synthetic biology, particularly for biosensor applications in complex samples, two critical performance parameters determine practical utility: dynamic range and response time. Dynamic range quantifies the ratio between the fully induced ("ON") and uninduced ("OFF") states of a genetic circuit, determining its signal-to-noise ratio and detection sensitivity. Response time measures how quickly the circuit transitions between states upon signal detection, crucial for real-time monitoring applications. Both parameters are profoundly influenced by genetic circuit design choices, component selection, and host-cell interactions. Optimizing these characteristics enables researchers to develop more reliable biosensors for diagnostic applications, bioprocess monitoring, and therapeutic interventions in complex biological environments where background interference and time-sensitive readings are significant concerns [65] [66].
Troubleshooting Guides & FAQs
Frequently Encountered Experimental Challenges
Q: My genetic circuit exhibits insufficient dynamic range (low ON/OFF ratio). What strategies can I implement to improve this?
A: Low dynamic range typically stems from high basal expression (leakiness) in the OFF state, inadequate activation in the ON state, or both. You can implement several troubleshooting strategies:
- Promoter Engineering: Modify promoter sequences to strengthen operator-repressor binding and reduce leakage. Site-directed mutagenesis of key nucleotides in the promoter region can significantly enhance repression efficiency [65].
- RBS Tuning: Optimize the Ribosome Binding Site (RBS) strength using computational tools to balance expression levels of regulatory proteins without creating metabolic burden [66].
- Dual Repression Systems: Implement layered regulation such as CRISPRi combined with transcriptional repressors to synergistically reduce background expression [66].
- Homolog Screening: Test orthologous transcription factors from different microbial species, as natural variation can provide components with more favorable binding characteristics [65].
Q: How can I reduce the response time of my genetically encoded biosensor?
A: Slow response times limit real-time monitoring applications. Consider these approaches:
- Regulator Protein Stability: Incorporate degradation tags (e.g., ssrA) to regulatory proteins to accelerate their turnover, enabling faster state transitions [66].
- Promoter Strength Balancing: Use weaker promoters to express repressor proteins and stronger promoters for output genes – this optimization reduces the time required to overcome repression upon induction [67].
- Signal Amplification Circuits: Implement positive feedback architectures that trigger rapid, switch-like responses once a threshold metabolite concentration is detected [66].
- Direct Output Coupling: Design circuits where the detected metabolite directly regulates the output gene expression rather than through intermediate regulators, minimizing transduction steps [65].
Q: My biosensor performs well in buffer but behaves unpredictably in complex samples like serum or cell lysates. How can I improve robustness?
A: Performance discrepancies between simple and complex matrices present a common challenge in biosensor deployment:
- Orthogonal Circuit Components: Utilize genetic parts (promoters, RBSs, terminators) that minimize crosstalk with host cellular machinery to reduce context-dependent behavior [66].
- Host Strain Optimization: Use engineered chassis strains with reduced protease activity or modified metabolism to decrease non-specific circuit interference [65].
- Circuit Insulation: Incorporate insulator sequences around your genetic circuit to minimize positional effects and chromatin context influences when integrating into the host genome [67].
- Calibration References: Implement internal calibration standards, such as constitutive fluorescent proteins, to normalize for matrix effects and provide ratiometric measurements [43].
Q: The metabolic burden of my genetic circuit causes reduced host cell growth over time. How can I mitigate this?
A: Metabolic burden indicates resource competition between the circuit and essential cellular processes:
- Circuit Compression: Apply "Transcriptional Programming" (T-Pro) designs that achieve complex logic with fewer genetic components, significantly reducing cellular load [68].
- Tunable Expression: Incorporate inducible systems that keep circuit expression minimal until activation is required, conserving cellular resources during growth phases [66].
- Dynamic Regulation: Implement autonomous metabolic sensing that only activates the biosensor circuit when cellular resources are abundant [65].
- Genomic Integration: Move from high-copy plasmids to single-copy genomic integrations to create more stable, lower-burden circuit implementations [67].
Quantitative Performance Optimization Data
Table 1: Strategies for Enhancing Genetic Circuit Dynamic Range
| Optimization Method | Implementation Example | Performance Improvement | Key Considerations |
|---|---|---|---|
| Transcription Factor Engineering | Site-directed mutagenesis of PdhR biosensor [65] | Significant enhancement in sensitivity and leakage control | Requires structural knowledge of protein-DNA interactions |
| Homolog Screening | Screening PdhR homologs from various microorganisms [65] | Identified variants with improved response characteristics | Orthogonality to host machinery must be verified |
| Circuit Compression | T-Pro design with anti-repressors [68] | 4x smaller circuits with maintained function | Computational design expertise needed |
| Layered Regulation | CRISPRi + transcriptional repression [66] | Synergistic reduction in background leakage | Potential for increased metabolic burden |
Table 2: Approaches for Improving Genetic Circuit Response Time
| Optimization Strategy | Technical Implementation | Impact on Response Time | Trade-offs |
|---|---|---|---|
| Protein Degradation Tags | Adding ssrA degrons to repressor proteins [66] | Faster turnover of regulatory elements | Potential for increased expression noise |
| Promoter Strength Tuning | Weaker promoters for repressors, stronger for outputs [67] | Reduced transition time between states | Requires careful balancing to maintain function |
| Positive Feedback Loops | Auto-regulatory architectures [66] | Switch-like response acceleration | Risk of hysteresis and unintended activation |
| Direct Regulation | Eliminating intermediate steps [65] | Minimal signal transduction delay | Limited opportunities for signal amplification |
Experimental Protocols for Critical Optimizations
Protocol: Dynamic Range Enhancement Through TF Engineering
This protocol describes the optimization of transcription factor properties to enhance biosensor dynamic range, based on methodologies successfully applied to the PdhR pyruvate-responsive system [65].
Materials Required:
- E. coli BW25113 or similar laboratory strain
- Plasmid system with modular cloning capability (e.g., Golden Gate, Gibson Assembly)
- Site-directed mutagenesis kit
- Flow cytometer for fluorescence measurements
- Microplate reader for growth and induction assays
Procedure:
- Homolog Identification: Perform protein BLAST to identify natural transcription factor homologs from diverse microbial species. Select 5-10 candidates with 40-80% sequence identity to balance diversity with functional conservation.
- Circuit Assembly: Clone each homolog into your biosensor backbone, replacing the native transcription factor while maintaining consistent regulatory elements.
- Initial Characterization: Measure the ON and OFF states of each variant using fluorescence output. Calculate dynamic range as ON/OFF ratio.
- Computational Analysis: Perform molecular modeling of promising candidates to identify amino acid residues critical for DNA binding affinity and ligand response.
- Site-Directed Mutagenesis: Create targeted mutations at identified residues to optimize binding characteristics. Focus on positions known to affect allostery or DNA interaction.
- Validation: Test mutant libraries for reduced leakage and enhanced induced expression. Select leads showing >2-fold improvement in dynamic range over native system.
- Context Testing: Validate performance in final application conditions (e.g., complex media, relevant metabolites).
Troubleshooting Notes:
- If all homologs show poor expression, consider codon optimization while preserving key functional residues.
- If dynamic range plateaus, combine beneficial mutations from different homologs.
- Always include the original system as a control throughout optimization.
Protocol: Response Time Acceleration via Degradation Tagging
This protocol describes the implementation of degradation tags to reduce regulator half-life, thereby accelerating biosensor response kinetics [66].
Materials Required:
- Degradation tag sequences (ssrA, other degrons)
- PCR equipment and high-fidelity polymerase
- Chromosomal integration system if needed
- Real-time monitoring equipment (e.g., microfluidic microscopy, plate reader with kinetic capabilities)
Procedure:
- Tag Design: C-terminally fuse degradation tags (e.g., ssrA: AANDENYALVA) to your repressor protein using flexible linkers (e.g., GSG repeated 2-4x).
- Circuit Modification: Replace native regulator with tagged version in your genetic circuit.
- Half-Life Validation: Perform cycloheximide chase experiments or use inducible promoters to measure protein degradation rates.
- Kinetic Profiling: Monitor biosensor activation and deactivation kinetics after rapid metabolite pulses.
- Titration Testing: Test multiple repressor expression levels (via RBS tuning) to identify optimal concentration that balances response speed with adequate repression.
- Feedback Implementation: For additional acceleration, incorporate positive feedback by having the output activate its own expression.
- System Characterization: Quantify response time as time to reach 50% and 90% of maximum output (T50 and T90).
Troubleshooting Notes:
- If degradation is too rapid, leading to high leakage, try milder degradation tags or adjust linker length.
- If response becomes noisy, consider intermediate repressor expression levels or negative feedback stabilization.
- Verify that degradation machinery (e.g., ClpXP) is functional in your host strain.
Signaling Pathways and Workflow Visualizations
Diagram 1: Comprehensive workflow for optimizing genetic circuit performance, integrating both dynamic range and response time considerations.
Diagram 2: Genetic circuit architecture highlighting key intervention points for dynamic range and response time optimization.
Research Reagent Solutions
Table 3: Essential Research Reagents for Genetic Circuit Optimization
| Reagent/Category | Specific Examples | Function in Optimization | Implementation Notes |
|---|---|---|---|
| Transcription Factor Toolkit | PdhR (pyruvate-responsive), CelR (cellobiose-responsive), LacI variants [65] [68] | Provide sensing capability for dynamic regulation | Screen homologs for improved characteristics; engineer DNA binding specificity |
| Synthetic Promoter Libraries | T-Pro promoters, operator-modified constitutive promoters [68] [67] | Regulate circuit component expression levels | Balance strength to minimize burden while maintaining function |
| Degradation Tags | ssrA tag, custom degrons [66] | Accelerate protein turnover for faster response times | Position at C-terminus with flexible linkers; verify functionality in host |
| Circuit Assembly Systems | Golden Gate, Gibson Assembly, BioBricks [66] | Enable rapid iteration of circuit variants | Standardize parts for modular testing of different configurations |
| Modeling Software | ROSETTA3, T-Pro enumeration algorithms [65] [68] | Predict mutation effects and identify minimal circuit designs | Combine structural and circuit-level modeling for comprehensive optimization |
| Characterization Tools | Flow cytometry, microfluidics, plate readers [65] [66] | Quantify dynamic range and response time with statistical power | Use high-throughput methods to screen multiple variants in parallel |
Frequently Asked Questions (FAQs)
Q1: What are the most common environmental factors that cause biosensor calibration drift? The primary environmental stressors that trigger calibration drift are temperature fluctuations, humidity variations, and dust/particulate accumulation [69]. Temperature changes can cause physical expansion or contraction of sensor components, while high humidity can lead to condensation, causing short-circuiting or corrosion. Dust accumulation physically obstructs sensor elements, directly altering measurements and sensitivity [69].
Q2: How can I identify the early signs of calibration drift in my biosensor? Early signs include unexpected changes in data trends or inconsistencies in readings over time without a corresponding change in the environment [69]. A persistent mismatch between your sensor's readings and values from a known reference instrument is a key indicator. Changes in sensor response time, such as becoming sluggish or erratic, also suggest potential drift [69].
Q3: What is the recommended frequency for recalibrating biosensors used in complex samples? Calibration intervals are not fixed and depend heavily on the operating environment and sample matrix complexity [69] [70]. Environments with high levels of dust, extreme temperature swings, or high humidity necessitate more frequent checks. A best practice is to establish a schedule based on initial performance validation under your specific conditions and to perform regular verification against a standard [69].
Q4: How does the complexity of a food or biological sample matrix affect biosensor performance? Complex matrices like meat extracts or serum can introduce nonspecific binding and sensor fouling, which reduce reliability and reproducibility [71] [2]. Components in the sample can interfere with the biorecognition element or physically block the transducer surface. Strategies to mitigate this include using blocking agents, antifouling coatings, and sample pre-filtration or dilution [2].
Troubleshooting Guide: Common Issues and Solutions
| Problem | Possible Environmental Cause | Recommended Solution |
|---|---|---|
| Gradual Signal Deterioration | Dust accumulation on the sensing surface [69] | Implement routine cleaning with soft brushes or air blowers; use protective housings or filters [69]. |
| Erratic or Noisy Readings | Temperature fluctuations causing component misalignment or electronic variability [69] | Use sensors with temperature-compensating materials; allow sensor to stabilize in the test environment; employ temperature correction algorithms [2]. |
| Sudden Signal Drops or Inaccurate Data | High humidity leading to condensation and corrosion [69] | Ensure sensors are not exposed to 100% humidity; use protective housings with integrated dehumidifiers for extreme conditions [69]. |
| Loss of Sensitivity/Specificity | Fouling from complex sample matrices (e.g., proteins, cells) [71] [2] | Incorporate sample clean-up steps; use irreversible immobilization methods for bioreceptors; apply antifouling coatings to the sensor surface [72] [2]. |
| Irreproducible Results Between Tests | Degradation of the biological element (enzyme, antibody) due to improper storage or pH [2] | Follow strict storage protocols; recalibrate regularly; use robust bioreceptor immobilization techniques to enhance stability [72] [2]. |
Experimental Protocols for Mitigating Environmental Sensitivities
Protocol 1: Establishing a Baseline and Assessing Temperature Influence
This protocol outlines the steps to characterize how temperature affects your biosensor's signal.
- Objective: To determine the optimal operating temperature and quantify the temperature coefficient of the biosensor.
- Materials:
- Biosensor unit
- Thermostatic chamber or water bath
- Precision thermometer
- Standard analyte solutions at known concentrations
- Data acquisition system
- Methodology:
- Step 1: Place the biosensor in the thermostatic chamber with a fixed concentration of the standard analyte solution.
- Step 2: Starting from a low temperature (e.g., 15°C), record the stable sensor signal.
- Step 3: Incrementally increase the temperature (e.g., in 5°C steps) up to a maximum (e.g., 40°C), allowing for equilibration at each step and recording the signal.
- Step 4: Plot the sensor response versus temperature. The plateau region indicates the optimal temperature range.
- Step 5: Calculate the temperature coefficient (e.g., % signal change per °C) outside the optimal range for future data correction.
- Data Interpretation: A sharp change in signal outside a specific range indicates high temperature sensitivity, necessitating tight environmental control or algorithm-based correction [69] [2].
Protocol 2: Evaluating and Minimizing Matrix Interference in Complex Samples
This protocol helps validate biosensor performance in complex sample matrices like serum or food homogenates.
- Objective: To assess the extent of matrix interference and establish a standard addition method for accurate quantification.
- Materials:
- Biosensor unit
- Complex sample matrix (e.g., diluted serum, ground meat extract)
- Standard analyte stock solution
- Buffer for dilution
- Methodology:
- Step 1 (Calibration in Buffer): Perform a standard calibration curve by measuring the sensor response to a series of known analyte concentrations in a clean buffer solution.
- Step 2 (Standard Addition):
- Take several equal aliquots of the unknown complex sample.
- Spike these aliquots with increasing known amounts of the standard analyte.
- Measure the sensor response for each spiked sample.
- Step 3: Plot the sensor response against the concentration of the added standard. The x-intercept of this line corresponds to the concentration of the analyte in the original, unspiked sample.
- Data Interpretation: This method accounts for the multiplicative and additive effects of the sample matrix, providing a more accurate measurement than direct extrapolation from a buffer-based calibration curve [73] [2].
Research Reagent Solutions and Essential Materials
The following table details key reagents and materials critical for developing and stabilizing biosensors against environmental challenges.
| Item | Function/Benefit |
|---|---|
| NIST-Traceable Standards | Provides an unbroken chain of comparisons to a primary standard, ensuring measurement accuracy and fulfilling regulatory requirements [70]. |
| Enzyme Mutants (Robust Variants) | Engineered enzymes offer enhanced stability against temperature and pH variations, improving biosensor reliability in non-ideal conditions [2]. |
| Antifouling Coatings (e.g., PEG) | Polyethylene glycol (PEG) and similar coatings create a hydrophilic barrier on the sensor surface, reducing nonspecific protein adsorption and fouling from complex samples [2]. |
| Blocking Agents (e.g., BSA) | Proteins like Bovine Serum Albumin (BSA) are used to cover non-specific binding sites on the sensor surface, minimizing background noise and interference [2]. |
| Stabilizing Buffers | Specially formulated buffers maintain the correct pH and ionic strength, preserving the activity and longevity of the immobilized biological recognition element [11] [2]. |
Workflow and Signaling Pathways
The following diagram illustrates the logical workflow for managing biosensor calibration and troubleshooting in the face of environmental sensitivities.
Biosensor Environmental Management Workflow
Advanced Signal Processing and Digital Filtering Techniques
Technical Support Center
Troubleshooting Guides
Issue 1: Poor Signal-to-Noise Ratio (SNR) in Ultralow-Level Measurements
- Problem: The target analyte signal is barely higher than the intrinsic electronic noise or environmental background, leading to poor signal clarity and unreliable measurements [55].
- Solution:
- Hardware: Integrate low-noise amplifiers and use shielded circuitry to reduce electrical interference [55].
- Signal Processing: Apply digital filtering and time-based averaging to extract meaningful signals from noisy data [55].
- Sensor Design: Employ redundant sensing to confirm real signals across multiple sensor elements [55].
Issue 2: Signal Drift and Environmental Sensitivity
- Problem: Sensor readings are unstable due to fluctuations in temperature, humidity, or electromagnetic interference, a critical issue for ultralow-level detection [55].
- Solution:
- Environmental Control: Calibrate and operate sensors in a controlled environment with stable temperature and humidity [55].
- Software Compensation: Implement real-time compensation algorithms that adjust for environmental drift [55].
- Reference Sensors: Use a dual-sensor approach with a reference sensor to detect and compensate for changes caused by side events like temperature fluctuations [7].
Issue 3: Cross-Interference and Selectivity in Complex Samples
- Problem: The sensor responds to non-target, chemically similar molecules, leading to false positives or inaccurate concentration readings [55] [74].
- Solution:
- Surface Chemistry: Utilize chemically selective coatings or membranes to reduce interference from non-target substances [55].
- Data Validation: Validate sensor outputs with independent laboratory techniques like chromatography where possible [55].
- Optimize Settings: Fine-tune sensor parameters to favor specific chemical interactions of the target analyte [55].
Issue 4: Calibration Standard Accuracy and Contamination
- Problem: Trace-level calibration standards are unstable or impure, and minute contaminants can overwhelm the target analyte [55].
- Solution:
- Traceable Standards: Use reference standards certified by national metrology institutes (e.g., NIST) for calibration [55].
- Inert Materials: Construct calibration systems from inert materials like stainless steel or PTFE to minimize contamination risks [55].
- Automation & Purity: Employ ultra-high-purity gases and implement automated sampling to reduce human-induced contamination [55].
Frequently Asked Questions (FAQs)
Q1: What are the primary digital signal processing techniques used to enhance biosensor signals? Advanced techniques include parametric spectral analysis (e.g., LPC, Lattice), adaptive signal processing algorithms (e.g., LMS, NLMS), and model-based processing (e.g., Kalman filters) [75]. For practical implementation, finite impulse response (FIR) and infinite impulse response (IIR) digital filters are fundamental, alongside the discrete and fast Fourier transform for frequency domain analysis [76].
Q2: How can I validate the performance of a new biosensor in a complex sample matrix? A new sensor must be tested on various unmodified, unspiked real-world samples and cross-validated with an established reference method (e.g., validating a gas sensor with GC-MS) [74]. It is critical to test the biosensor not only with the target analyte but also with body fluids or other complex matrices that contain all possible interfering compounds [74].
Q3: What are the key stability challenges for biosensors, and how can they be addressed? Challenges include both shelf stability (retention of activity of biological elements during storage) and operational stability (reusability and performance during use) [74]. For single-use biosensors, shelf-stability is key and can be managed through strict control of the storage environment. For multi-use biosensors, immobilization strategies that maintain biological activity are crucial [7] [74].
Q4: Why are optical biosensors sometimes preferred over electrochemical ones in certain applications? Optical biosensors (e.g., those based on fluorescence, luminescence, or SPR) offer advantages such as immunity to electrical or magnetic interference, multiplex capability (guiding light of different wavelengths), and suitability for in-vivo measurements [7]. They are particularly useful when measurements are required in harsh environments or when no analytes are consumed during detection [7].
Experimental Protocols and Data
Detailed Methodology: SERS-Based Immunoassay for Biomarker Detection
This protocol is adapted from a study on a surface-enhanced Raman scattering (SERS) platform for detecting the α-fetoprotein (AFP) biomarker [77].
- Nanostar Synthesis and Concentration: Synthesize spiky Au-Ag nanostars. Concentrate the nanostars via simple centrifugation, evaluating different durations (e.g., 10, 30, and 60 minutes) to tune the final concentration [77].
- SERS Performance Evaluation: Incubate the nanostars with probe molecules like methylene blue (MB) or mercaptopropionic acid (MPA). Evaluate the SERS signal intensity to confirm it scales with nanostar content [77].
- Sensor Functionalization:
- Functionalize the optimized nanostars with MPA.
- Activate the carboxyl groups using 1-Ethyl-3-(3-dimethylaminopropyl) carbodiimide (EDC) and N-Hydroxy succinimide (NHS) chemistry.
- Covalently attach monoclonal anti-α-fetoprotein antibodies (AFP-Ab) to the activated surface [77].
- Antigen Detection and Calibration:
- Expose the functionalized platform to samples containing AFP antigen.
- Detect the intrinsic vibrational modes of the captured AFP.
- Generate a calibration curve across the concentration range of 500–0 ng/mL. The limit of detection (LOD) for this protocol was determined to be 16.73 ng/mL [77].
Table 1: Performance Metrics of Featured Biosensing Techniques
| Biosensor Type / Component | Key Performance Metric | Reported Value / Range | Application Context |
|---|---|---|---|
| SERS Immunoassay [77] | Detection Range | 0 - 500 ng/mL | Cancer biomarker (AFP) detection |
| Limit of Detection (LOD) | 16.73 ng/mL | ||
| Enzyme-free Glucose Sensor [77] | Sensitivity | 95.12 ± 2.54 µA mM⁻¹ cm⁻² | Wearable health monitoring |
| THz SPR Biosensor [77] | Phase Sensitivity (Liquid) | 3.1043 × 10⁵ deg RIU⁻¹ | Chemical detection & medical diagnostics |
| Phase Sensitivity (Gas) | 2.5854 × 10⁴ deg RIU⁻¹ | ||
| DirectSens Maltose & Glucose [78] | Measuring Range (Maltose) | 6 – 120 g/L | Food quality control (oat/rice drinks) |
| Measuring Range (Glucose) | 2 – 120 g/L | ||
| Repeatability (Glucose) | < 7 % (std. dev.) | ||
| Repeatability (Maltose) | < 10 % (std. dev.) |
Table 2: Research Reagent Solutions for Biosensor Development
| Reagent / Material | Function / Explanation |
|---|---|
| Au-Ag Nanostars [77] | Plasmonic nanoparticles with sharp-tipped morphology that provide intense signal enhancement for optical sensing techniques like SERS. |
| Mercaptopropionic Acid (MPA) [77] | A self-assembled monolayer (SAM) molecule used to functionalize gold surfaces, providing carboxyl groups for subsequent biomolecule immobilization. |
| EDC/NHS Chemistry [77] | A cross-linking system used to activate carboxyl groups, enabling covalent and stable immobilization of antibodies or other biorecognition elements. |
| Glucose Oxidase [74] | A highly stable and specific enzyme that serves as the biorecognition element in the vast majority of commercial glucose biosensors. |
| Polydopamine/Melanin-like Materials [77] | Biocompatible, versatile coatings that emulate mussel adhesion proteins, useful for surface modification and fabrication of electrochemical sensors. |
| Selective Coatings/Membranes [55] | Engineered surfaces or layers applied to the sensor to improve selectivity by reducing interference from non-target substances in complex samples. |
Workflow Visualization
Biosensor Signal Processing Workflow
Ultralow-Level Sensor Calibration Protocol
Validation Frameworks and Comparative Analysis of Calibration Methods
Validation Protocols for Biosensor Performance in Clinical Samples
Core Validation Principles & FAQs
This section addresses foundational concepts and common challenges in biosensor clinical validation.
FAQ 1: What constitutes a complete clinical validation strategy for investors and regulators? A well-staged validation strategy is crucial for securing funding and regulatory approval. It should follow an "evidence ladder" that systematically de-risks the technology [79]:
- Analytical Validation: Assesses basic performance parameters like limit of detection (LOD), linearity, and repeatability in a controlled lab setting (2-8 weeks).
- Technical/Engineering Verification: Includes hardware/software stress tests, electromagnetic compatibility (EMC), and electrical safety per standards like IEC 60601.
- Controlled Clinical Accuracy: Compares biosensor performance against a gold standard in ideal, often retrospective, sample sets.
- Prospective Clinical Validation: Conducted in the intended-use population under real-world conditions; this is critical for winning investor confidence.
- Real-World Performance & Utility: Deploys the device in its target environment to demonstrate impact on clinical decisions and health economics [79].
FAQ 2: How do I select an appropriate gold-standard comparator for my clinical study? The choice of comparator is a critical design decision that must align with the biosensor's intended use [79]:
Table 1: Gold-Standard Comparator Selection Guide
| Biosensor Measurement Target | Recommended Gold Standard | Key Considerations |
|---|---|---|
| Cardiac Rhythm/Arrhythmia | 12-lead ECG, interpreted by at least two cardiologists | Adjudicate disagreements; continuous Holter monitoring for longer observations [79]. |
| Heart Rate | Clinical-grade ECG | Ensure time-synchronized, beat-to-beat comparison [79]. |
| Blood Pressure (Cuffless) | Validated automated upper-arm sphygmomanometer (per ISO 81060) or Ambulatory BP Monitoring (ABPM) | Follow established ISO protocols for validation [79]. |
| SpO₂ | Clinical-grade Masimo or hospital pulse oximeter | Explicitly test for performance bias across different skin tones [79]. |
FAQ 3: My biosensor shows significant signal drift in complex samples. What are the primary causes? Signal drift can stem from multiple factors related to the sample and sensor interface:
- Insufficient Surface Equilibration: The sensor surface may not be optimally equilibrated with the running buffer, often requiring extended flushing (e.g., overnight) or multiple buffer injections before the experiment [80].
- Bulk Effects: Differences in composition between the flow buffer and the sample can cause shifts. Always match the flow and analyte buffers to minimize this [80].
- Biofouling: In complex samples like plasma, nonspecific adsorption of proteins or other biomolecules to the sensor surface can alter signal and cause drift. Implementing robust antifouling strategies is critical for long-term stability [81].
FAQ 4: How can I improve the reproducibility of my biosensor readings across diverse patient populations?
- Explicit Subgroup Testing: Proactively test and report device performance stratified by skin tone (using Fitzpatrick scale or measured reflectance), BMI, age, and motion levels [79].
- Self-Calibration Designs: Integrate a self-calibration mechanism to correct for signal fluctuations. For instance, a SERS-based biosensor can use an internal standard (e.g., the C dot signal on a test strip) to normalize the target signal, correcting for instrument variability and sample matrix effects [43].
- Usability Studies: If healthcare workers or patients apply the device, conduct real-user training and monitor error rates to identify and mitigate use-related inconsistencies [79].
Troubleshooting Common Experimental Issues
This guide helps diagnose and resolve specific technical problems.
Table 2: Troubleshooting Common Biosensor Issues
| Problem | Potential Causes | Solutions & Diagnostic Steps |
|---|---|---|
| High Background Noise/ Low Signal-to-Noise | 1. Non-specific binding2. Fluorescent impurity in reagents3. Suboptimal laser power/detection settings | 1. Include blocking agents (e.g., BSA, serum)2. Purify reagents or use higher purity grades3. Perform signal-to-noise optimization experiments [81] |
| Low Sensitivity/ High Limit of Detection | 1. Inefficient biorecognition element immobilization2. Signal amplification strategy failure3. Calibration drift | 1. Optimize surface chemistry and immobilization protocol2. Employ additional amplification (e.g., nanozymes, enzymatic amplification)3. Use a self-calibrating biosensor design [43] |
| Poor Reproducibility (High CV%) | 1. Inconsistent sample preparation2. Sensor surface heterogeneity3. Fluctuations in environmental conditions (temp, humidity) | 1. Standardize and automate sample prep protocols2. Characterize surface uniformity; use quality-controlled production batches3. Control the assay environment; use internal calibration standards [43] [81] |
| Spikes or Sudden Signal Drops During Injection | 1. Sample carry-over2. Air bubbles in the microfluidic system3. Sample dispersion | 1. Add extra wash steps between injections2. Degas buffers; include bubble traps in fluidic path3. Check and optimize instrument routines that separate sample from flow buffer [80] |
Detailed Experimental Protocols
Protocol for a Self-Calibrated SERS-LFIA Biosensor
This protocol outlines the development of a surface-enhanced Raman scattering lateral flow immunoassay (SERS-LFIA) for detecting protein kinase biomarkers, incorporating a self-calibration mechanism for superior accuracy in complex samples [43].
1. Principle The biosensor uses SERS nanoprobes functionalized with antibodies and a Raman reporter. As the sample migrates, the target antigen (e.g., PEAK1) binds the nanoprobes, forming a complex captured at the test line. The control line captures excess nanoprobes. The key innovation is using the SERS signal from the control line as an internal standard to normalize the test line signal, correcting for fluctuations from flow rate variability, environmental changes, or instrument settings [43].
2. Reagents and Materials
- SERS Substrate: Silver nanoflowers (AgNFs) synthesized from AgNO₃, sodium citrate, and ascorbic acid.
- Raman Reporter: Molecules like 4-mercaptobenzoic acid (MBA).
- Biological Reagents: Capture antibody, detection antibody, and target antigen.
- Lateral Flow Components: Sample pad, conjugate pad, nitrocellulose (NC) membrane, and absorbent pad.
- Equipment: Raman spectrometer.
3. Step-by-Step Procedure A. Preparation of SERS Nanoprobes:
- Synthesize AgNFs via a one-pot method using AgNO₃, sodium citrate, and ascorbic acid.
- Functionalize AgNFs with the Raman reporter (e.g., MBA).
- Conjugate the MBA-labeled AgNFs with the detection antibody to form the SERS nanoprobes.
- Dispense the nanoprobes onto the conjugate pad and dry.
B. Assembly of the Test Strip:
- Dispense the capture antibody at the Test (T) line of the NC membrane.
- Dispense the appropriate ligand (e.g., a secondary antibody) at the Control (C) line.
- Assemble the sample pad, conjugate pad, NC membrane, and absorbent pad on a backing card.
C. Detection and Quantification:
- Apply the clinical sample (e.g., plasma, cell lysate) to the sample pad.
- Allow the sample to migrate and react for a predetermined time (e.g., 15-20 minutes).
- Scan the T and C lines with a Raman spectrometer to collect their respective SERS signals (IT and IC).
- Calculate the normalized signal (IT / IC) for quantification.
4. Data Analysis
- Plot the normalized signal (IT / IC) against the logarithm of the target antigen concentration.
- Fit the data to a logistic or linear function to create a calibration curve.
- The self-calibrating ratio corrects for internal and external interferences, enabling highly accurate and reproducible quantification in complex matrices [43].
Protocol for Electrochemical Impedance Spectroscopy (EIS) of Epithelial Barriers
This protocol uses EIS to provide a more comprehensive assessment of epithelial barrier integrity than traditional transepithelial electrical resistance (TEER) alone, yielding parameters like transepithelial capacitance (TEC) [82].
1. Principle Galvanostatic EIS applies a small, sinusoidal alternating current across an epithelial tissue and measures the voltage response. The impedance spectrum reveals resistive and capacitive properties of the transcellular and paracellular pathways, providing insights into barrier function and cell membrane properties [82].
2. Reagents and Materials
- Epithelial Cells: Grown on commercially available cell culture inserts.
- Electrophysiology Chamber: Compatible with the cell culture inserts.
- Instrumentation: Potentiostat or impedance analyzer capable of galvanostatic EIS.
3. Step-by-Step Procedure
- Culture epithelial cells on permeable supports until they form a confluent monolayer.
- Place the cell culture insert into the electrophysiology chamber.
- Add the appropriate buffer to both the apical and basolateral chambers.
- Set the instrument to galvanostatic mode with a sinusoidal current amplitude of 4 μA and a frequency sweep from 2 Hz to 50 kHz.
- Acquire the impedance data.
4. Data Analysis
- Fit the obtained impedance spectra to a suitable equivalent circuit model (e.g., a resistor representing the paracellular path in parallel with a capacitor, both in series with the solution resistance).
- From the fit, extract parameters including Transepithelial Resistance (TER), Transepithelial Capacitance (TEC), and the membrane ratio (ratio of electrical time constants).
- A successful fit should have a mean absolute error of less than 10 Ω [82].
Essential Research Reagent Solutions
Table 3: Key Reagents for Biosensor Calibration and Validation
| Reagent/Material | Function/Purpose | Example Application |
|---|---|---|
| Silver Nanoflowers (AgNFs) | SERS substrate providing massive signal enhancement (AEF ~10⁸) for ultra-sensitive detection. | Signal amplification in SERS-LFIA biosensors for biomarker detection [43]. |
| Europium Complex-Loaded Albumin Nanoparticles | Long-lifetime luminescent labels for time-resolved immunoassays, eliminating background fluorescence. | Used as labels in solid-phase immunoassays for protein detection (e.g., IgG) [81]. |
| Covalent Organic Frameworks (COFs) | Porous, tunable structures that enhance electrochemiluminescence (ECL) via mass transport and electron transfer. | Serving as ECL emitters or scaffolds in high-performance ECL biosensors [81]. |
| Clinical-Grade Gold Standard Devices | Provide the reference measurement for clinical validation studies. | 12-lead ECG for cardiac rhythm, validated sphygmomanometer for blood pressure [79]. |
| Fitzpatrick Scale or Reflectance Spectrometer | Objectively categorize skin tones to test for and mitigate performance bias across populations. | Equity and usability testing for optical biosensors (e.g., pulse oximeters) [79]. |
Workflow and Signaling Pathway Diagrams
What is the fundamental role of calibration in biosensor performance? Calibration is a critical process that establishes the relationship between the biosensor's signal and the concentration of the target analyte. It defines the sensor's slope (responsiveness) and zero point (baseline), which are essential for converting raw signal data into meaningful quantitative measurements. Since both parameters can drift over time due to environmental factors and sensor aging, frequent calibration is necessary to maintain data integrity [83].
How does this technical support center address researcher needs? This support center provides a structured framework for troubleshooting calibration issues, comparing established methods against innovative approaches, and offering practical protocols. The content is specifically designed for researchers working with biosensors in complex sample matrices, where interference and matrix effects pose significant challenges to measurement accuracy.
Comparative Analysis: Traditional vs. Novel Approaches
The table below summarizes the core differences between traditional calibration methodologies and emerging novel strategies, highlighting their respective applications and limitations.
| Feature | Traditional Calibration Approaches | Novel Calibration Approaches |
|---|---|---|
| Core Principle | Establishes slope and zero point using standard solutions [83]; Often requires manual intervention and recalibration. | Leverages advanced algorithms [84], genetic circuits [11], and AI [85] for automated and intelligent calibration. |
| Primary Applications | Routine measurements in lab and field settings (e.g., pH meters [83]). | Robotic TMS systems [84], GEM biosensors for heavy metals [11], smartphone-based point-of-care diagnostics [85]. |
| Key Advantages | Well-understood, standardized protocols, widely applicable. | Enhanced accuracy in dynamic environments [84], specificity for novel analytes [11], potential for continuous self-calibration. |
| Key Limitations/Challenges | Performance variability in complex samples; Requires frequent recalibration; Susceptible to environmental drift [85] [83]. | Computational complexity; Requires specialized equipment or materials (e.g., genetically engineered cells [11]); Can be application-specific. |
| Representative Data Output | Linear calibration curve (e.g., mV vs. pH) [83]. | Multi-parameter linear models (e.g., for Cd²⁺, Zn²⁺, Pb²⁺ with R² > 0.97) [11]. |
| Error Reduction | Highly dependent on user technique and buffer freshness [83]. | Demonstrated significant reduction in robotic positioning errors (34% position, 19% orientation) [84]. |
Detailed Experimental Protocols
Protocol 1: Traditional 2-Point Electrochemical Calibration
This protocol is fundamental for calibrating sensors like pH electrodes and forms the basis for many quantitative biosensors [83].
- Step 1: Preparation. Gather fresh, unexpired pH buffer solutions. pH 7 buffer MUST be used as one calibration point. The second buffer should differ by at least two pH units and bracket your expected sample pH (e.g., pH 4 and pH 7 for acidic samples, or pH 7 and pH 10 for basic samples). Never re-use buffers for calibration, as they become contaminated [83].
- Step 2: Initial Rinse. Rinse the electrode with deionized (DI) water. Gently dab it dry with a clean, lint-free tissue to avoid scratching the glass bulb. Do not wipe, as this can generate static electricity and affect readings [83].
- Step 3: Calibration in Buffer 7. Immerse the electrode in the first container of pH 7 buffer. Allow the reading to stabilize. The response time should typically be less than 60 seconds for a healthy electrode. Once stable, record the calibration point on your instrument [83].
- Step 4: Rinse and Calibrate in Second Buffer. Rinse the electrode again with DI water. For the best practice, rinse the electrode with a small amount of the second buffer you are about to use (e.g., pH 10 buffer). Immerse it in the second buffer solution, allow the reading to stabilize, and record the calibration point [83].
- Step 5: Verification and Troubleshooting. Check the calibrated slope and zero point. A slope of 95-105% and a zero point within ±50 mV of the theoretical value indicate a well-functioning probe. Never accept an out-of-range calibration, as it will not yield usable data [83].
Protocol 2: Calibration of a Novel GEM Biosensor for Heavy Metals
This protocol outlines the calibration of a genetically engineered microbial (GEM) biosensor for detecting heavy metal ions like Cd²⁺, Zn²⁺, and Pb²⁺, demonstrating a modern bio-calibration approach [11].
- Step 1: Stock Solution Preparation. Prepare 100 ppm stock solutions of heavy metal ions (e.g., Cd²⁺, Pb²⁺, Zn²⁺) using high-purity salts like CdCl₂, Pb(NO₃)₂, and Zn(CH₃COO)₂ dissolved in ddH₂O. Confirm the exact concentration using a reference method like Microwave Plasma-Atomic Emission Spectrometry (MP-AES) [11].
- Step 2: Serial Dilution. Perform serial dilutions from the stock solutions to create a standard curve. The study used a range of 0.1 ppm to 5.0 ppm (which is 1 to 50 ppb), covering low-concentration detection limits [11].
- Step 3: Biosensor Incubation. Inoculate the GEM biosensor cells (e.g., E. coli-BL21 containing the CadA/CadR-eGFP genetic circuit) into culture media. Expose these cultures to the different concentrations of heavy metal standards. Incubate under optimal physiological conditions for the biosensor (e.g., 37°C, pH 7.0) for a specified period to allow for reporter gene expression [11].
- Step 4: Fluorescence Measurement. After incubation, measure the fluorescent intensity of the eGFP reporter protein expressed in the biosensor cells. This can be done using fluorometry, fluorescence microscopy, or other plate-reading instruments [11].
- Step 5: Calibration Curve Generation. Plot the measured fluorescent intensity against the known concentration of each heavy metal ion. The biosensor is considered successfully calibrated when it generates a linear response with a high coefficient of determination (R²), such as 0.9809 for Cd²⁺, as reported in the study [11].
Workflow Visualization
Logical Pathway of a NOT Gate GEM Biosensor
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key materials and their functions for implementing the calibration methodologies discussed.
| Item Name | Function / Role in Calibration |
|---|---|
| pH Buffer Solutions | Provides known, stable pH references for establishing the slope and zero point of electrochemical sensors like pH electrodes. Must be fresh and unexpired [83]. |
| Genetically Engineered Microbial (GEM) Biosensor | Contains a synthetic genetic circuit (e.g., CadA/CadR-eGFP) that responds to specific analytes (e.g., heavy metals) by producing a measurable signal (e.g., fluorescence) [11]. |
| Enhanced Green Fluorescent Protein (eGFP) | A reporter protein that emits green fluorescence when expressed. Its intensity is quantitatively measured to correlate with analyte concentration in GEM biosensors [11]. |
| Chloride Salts (e.g., CdCl₂) | Source of heavy metal ions (e.g., Cd²⁺) for preparing standard stock solutions used in calibrating heavy metal biosensors [11]. |
| 3 M KCl (Ag⁺ free) Solution | Storage and rehydration solution for laboratory pH electrodes. Prevents the electrode from drying out and maintains stable reference junction potential [83]. |
| Impedance Control Algorithm | A sophisticated robot control strategy that guarantees both high positioning accuracy and safe physical interaction during robotic TMS calibration procedures [84]. |
Frequently Asked Questions (FAQs)
Q1: My pH probe is responding slowly during calibration and failing to stabilize. What could be wrong? A slow response time (longer than 60 seconds) often indicates an aged or dirty probe. Electrodes have a typical lifespan of 12-18 months. Check the manufacturing lot code to determine its age. Routine maintenance is also critical; soak the electrode in a 1:1 bleach solution for 15-30 minutes to clean a clogged reference junction, or in 0.1M HCL for 5 minutes for lab electrodes. Also, ensure you are using fresh, unused buffer solutions for calibration, as reused or expired buffers are a common cause of poor performance [83].
Q2: Why is the calibration of my smartphone-based biosensor inconsistent across different devices? Inconsistency often stems from a lack of standardized components and interoperability between different smartphone models. Variations in cameras, sensors, and processing units can lead to signal processing differences. Furthermore, environmental variability (temperature, humidity) and complex calibration procedures that are not user-friendly can distort readings. Developing a unified calibration framework and using explainable AI for signal interpretation are strategies being researched to overcome these challenges [85].
Q3: What does a failed calibration on my instrument typically indicate, and what should I check first? A failed calibration usually indicates the sensor's slope and/or zero point are outside acceptable ranges. Your first steps should be:
- Check Probe Age: Probes older than 18 months likely need replacement [83].
- Inspect for Damage: Look for cracks in the glass bulb or body [83].
- Verify Buffer Quality: Confirm you are using fresh, unexpired buffers and have not reused them [83].
- Check mV Values: If your instrument allows, check the millivolt (mV) reading in pH 7 buffer. It should be 0 ±50 mV. The reading in pH 4 should be +165 to +180 mV from the pH 7 value, and in pH 10 it should be -165 to -180 mV. Significant deviations confirm a probe issue [83].
Q4: How can I improve the accuracy of my robotic biosensor positioning system? Employing an application-specific calibration methodology can significantly enhance accuracy. For example, in robotic TMS, a calibration strategy constrained to the specific spherical shell workspace around a subject's head reduced calibration errors by 34% in position and 19% in orientation compared to general-purpose algorithms. This tailored approach, combined with a robust impedance controller, ensures both high accuracy and user safety [84].
Q5: My GEM biosensor shows a high background signal even without the target analyte. What might be the cause? A high background signal, or lack of specificity, can be due to "leaky" expression of the reporter gene in your genetic circuit. This means the promoter is active even in the absence of the target inducer. To address this, review the design of your genetic logic gate (e.g., the NOT gate in the CadA/CadR system). Optimizing the operator/promoter sequences and the binding affinity of the repressor protein (e.g., CadR) can minimize non-specific expression and improve the signal-to-noise ratio [11].
Troubleshooting Guides
ELISA Troubleshooting Guide
Problem: High Background Signal
| Possible Cause | Recommended Solution |
|---|---|
| Insufficient washing | Follow protocol washing procedures precisely. Add a 30-second soak step between washes and ensure plates are drained thoroughly [86] [87]. |
| Contaminated buffers | Prepare fresh wash and assay buffers [87]. |
| Plate sealers reused or not used | Use a fresh plate sealer for each incubation step to prevent well-to-well contamination [86] [87]. |
| Substrate exposed to light | Store substrate in the dark and limit light exposure during the assay [86]. |
Problem: Weak or No Signal
| Possible Cause | Recommended Solution |
|---|---|
| Reagents not at room temperature | Allow all reagents to sit at room temperature for 15-20 minutes before starting the assay [86]. |
| Incorrect reagent storage or expired reagents | Check storage conditions and confirm all reagents are within their expiration dates [86]. |
| Capture antibody did not bind to plate | Ensure an ELISA plate (not a tissue culture plate) is used. Dilute the capture antibody in PBS without carrier proteins [86] [87]. |
| Not enough detector antibody | For in-house assays, optimize detector antibody concentration. For kits, follow the recommended dilutions [86]. |
Problem: Poor Replicate Data (High Variation Between Wells)
| Possible Cause | Recommended Solution |
|---|---|
| Inconsistent pipetting technique | Check pipette calibration and technique. Ensure all dilutions are calculated correctly [86]. |
| Uneven coating or plate quality | For in-house assays, ensure consistent coating procedure and use high-quality plates [87]. |
| Inconsistent washing | Calibrate automated plate washers. Manually, ensure equal wash buffer volume across all wells [87]. |
| Edge effects (evaporation) | Always use plate sealers during incubations and avoid stacking plates [86]. |
Problem: Poor Standard Curve
| Possible Cause | Recommended Solution |
|---|---|
| Incorrect standard dilutions | Double-check calculations and pipetting when preparing serial dilutions [86] [88]. |
| Standard has degraded | Use a new vial of standard, prepared according to instructions [87]. |
| Capture antibody did not bind well | Use an ELISA plate and ensure correct coating incubation time [86]. |
HPLC-MS/MS Troubleshooting Guide
Problem: Low Sensitivity or Poor Peak Response
| Possible Cause | Recommended Solution |
|---|---|
| Sample loss during preparation | Review extraction efficiency (e.g., liquid-liquid extraction, SPE). Ensure proper reconstitution in a solvent compatible with the mobile phase [89]. |
| Ion suppression from matrix effects | Improve sample clean-up, optimize chromatographic separation to shift analyte retention time away from matrix interferences, or use a stable isotope-labeled internal standard [90]. |
| MS source contamination | Clean the ion source and spray needle according to the manufacturer's guidelines. |
Problem: Poor Chromatography (Peak Tailing or Broad Peaks)
| Possible Cause | Recommended Solution |
|---|---|
| Column degradation | Flush and regenerate the column. If performance does not improve, replace the column. |
| Inappropriate mobile phase pH/buffer | Ensure mobile phase pH is appropriately controlled (e.g., with ammonium acetate or formate) for the analytes of interest [89]. |
| Sample solvent stronger than mobile phase | Reconstitute the sample in a solvent that is weaker than or similar to the initial mobile phase composition. |
Problem: Inconsistent Retention Times
| Possible Cause | Recommended Solution |
|---|---|
| Mobile phase not equilibrated | Ensure the HPLC system is sufficiently equilibrated with the starting mobile phase before starting a sequence. |
| Fluctuations in mobile phase composition or flow rate | Prepare mobile phases consistently and check for pump malfunctions. |
| Temperature fluctuations | Use a column heater to maintain a consistent temperature [89]. |
Frequently Asked Questions (FAQs)
Q1: When benchmarking a new biosensor, why is it crucial to use a reference method like LC-MS/MS instead of just ELISA? While ELISA is a robust and high-throughput technique, it can suffer from matrix effects where components in complex samples (like serum or saliva) interfere with antibody binding, leading to inaccurate quantification [35] [91]. LC-MS/MS offers superior specificity by separating analytes chromatographically and identifying them based on their unique mass-to-charge ratio, making it less susceptible to such interferences. A 2025 study on salivary hormones concluded that LC-MS/MS was superior to ELISA, which showed poor performance for estradiol and progesterone, highlighting the importance of a more definitive reference method for validation [92].
Q2: What are the key advantages of MS-based methods over HPLC-UV for biosensor calibration in complex samples? MS detection provides significantly higher selectivity and sensitivity compared to UV detection. In complex samples, many compounds co-elute and absorb at similar UV wavelengths, leading to inaccurate results. MS/MS, especially using Multiple Reaction Monitoring (MRM), can distinguish the target analyte from these interferences based on its specific parent and product ions. Furthermore, MS methods can achieve detection limits in the nanogram-per-liter (ng/L) or even lower range, which is often necessary for measuring biomarkers in biological matrices at clinically relevant levels [89] [90].
Q3: My biosensor results in saliva do not match my ELISA results. What could be the cause? Saliva is a complex matrix containing mucins, enzymes, and bacteria that can interfere with immunoassays [35]. The antibodies in an ELISA kit might cross-react with structurally similar molecules or be sterically hindered by other components in saliva, leading to inaccurate readings. Your biosensor might be experiencing different matrix effects. To resolve this, benchmark both your biosensor and the ELISA against a reference LC-MS/MS method using the same saliva samples to determine which technology provides the more accurate result [93] [92].
Q4: What metrics should I compare when benchmarking my biosensor against a reference method? A comprehensive benchmark should include both analytical and practical metrics. The table below summarizes the key parameters for comparison.
Table: Key Metrics for Biosensor Benchmarking Against Reference Methods
| Metric | Description | Ideal Outcome |
|---|---|---|
| Sensitivity | Lowest concentration of analyte that can be reliably detected (LOD) and quantified (LOQ). | Biosensor LOD/LOQ should be fit-for-purpose, ideally comparable to the reference method [35] [93]. |
| Dynamic Range | The range of analyte concentrations over which the sensor provides a quantifiable response. | A linear range covering the expected physiological or target concentrations. |
| Accuracy | The closeness of the biosensor's measurement to the "true value" (from the reference method). | High correlation and a slope close to 1 in a scatter plot vs. the reference method [92]. |
| Precision | The repeatability (within-run) and reproducibility (between-run) of the biosensor's output. | Low coefficient of variation (%CV) for repeated measurements of the same sample. |
| Selectivity/Specificity | The ability of the biosensor to measure only the target analyte in the presence of potential interferents in the matrix. | Minimal signal change when interferents are present. Should be validated against the reference method in the target matrix [35] [91]. |
| Matrix Effect | The impact of sample components on the assay's ability to quantify the analyte. | Compare biosensor performance in a simple buffer versus the complex biological matrix (e.g., serum, saliva) [35]. |
Q5: How can I minimize matrix effects when validating a biosensor for blood-derived media? Blood, serum, and plasma are highly complex and are known to cause nonspecific binding and signal interference [91]. Several strategies can help:
- Sample Dilution: Diluting the sample can reduce the concentration of interfering substances, but this may also dilute the analyte below the detection limit.
- Surface Blocking: Functionalize the biosensor surface with effective blocking agents (e.g., BSA, casein) to minimize nonspecific adsorption of other proteins.
- Sample Pre-treatment: Incorporate simple filtration or centrifugation steps to remove cells or particulate matter.
- Use of a Robust Reference Method: Employ a matrix-insensitive reference method, such as LC-MS/MS with a stable isotope-labeled internal standard, which can correct for recovery losses and ion suppression [89] [90].
Experimental Protocols for Reference Methods
Protocol 1: Validating an LC-MS/MS Method for Biomarker Quantification in Plasma
This protocol is adapted from a validated method for quantifying compound K in human plasma [89].
1. Sample Preparation (Liquid-Liquid Extraction)
- Pipette 100 µL of plasma (calibration standard, quality control, or unknown sample) into a microcentrifuge tube.
- Add 100 µL of 10 mM potassium phosphate buffer (pH 7.4).
- Add 900 µL of ethyl acetate (extraction solvent).
- Vortex the mixture vigorously for 5 minutes.
- Centrifuge at high speed (e.g., 10,000-14,000 x g) for 10 minutes to separate the phases.
- Transfer the upper organic layer to a new tube.
- Evaporate the organic solvent to dryness under a gentle stream of nitrogen or using a speed vacuum concentrator.
- Reconstitute the dry residue in 100 µL of mobile phase (e.g., 10 mM ammonium acetate/methanol/acetonitrile) and vortex to mix.
- Transfer to an injection vial for LC-MS/MS analysis.
2. Instrumentation and Analytical Conditions (Example)
- HPLC System: Agilent 1200 series.
- Mass Spectrometer: API 4000 tandem mass spectrometer with ESI source.
- Column: Phenomenex Luna C18 (100 x 2.0 mm, 3 µm).
- Mobile Phase: 10 mM ammonium acetate : methanol : acetonitrile (5:47.5:47.5, v/v/v).
- Flow Rate: 0.5 mL/min.
- Injection Volume: 10 µL.
- Ionization Mode: Electrospray Ionization (ESI), positive mode.
- MRM Transitions: Optimize for your specific analyte (e.g., m/z 621.4→161.0 for compound K).
Protocol 2: Standard ELISA for Protein Detection
This protocol outlines the general steps for a sandwich ELISA, commonly used for detecting proteins like hormones or cancer biomarkers [93].
1. Coating
- Dilute the capture antibody in PBS (phosphate-buffered saline) to the recommended concentration.
- Add 100 µL/well to a 96-well ELISA plate.
- Seal the plate and incubate overnight at 4°C (or 1-2 hours at room temperature).
- Wash the plate 3 times with wash buffer (e.g., PBS with 0.05% Tween-20).
2. Blocking
- Add 200-300 µL/well of blocking buffer (e.g., 1-5% BSA in PBS) to all wells.
- Incubate for 1-2 hours at room temperature.
- Wash the plate 3 times as before.
3. Sample and Detection Antibody Incubation
- Add 100 µL/well of standards, samples, and controls diluted in an appropriate diluent.
- Incubate for 2 hours at room temperature (or as per kit instructions).
- Wash the plate 3 times.
- Add 100 µL/well of the detection antibody (biotinylated or enzyme-conjugated), diluted in diluent.
- Incubate for 1-2 hours at room temperature.
- Wash the plate 3 times.
4. Signal Development and Detection
- If using a biotinylated detection antibody, add Streptavidin-HRP (diluted in diluent) and incubate for 30 minutes. Wash the plate 3 times.
- Add 100 µL/well of substrate solution (e.g., TMB). Incubate in the dark for 10-30 minutes.
- Add 50-100 µL/well of stop solution (e.g., sulfuric acid).
- Read the absorbance immediately using a plate reader at the appropriate wavelength (e.g., 450 nm for TMB).
Essential Research Reagent Solutions
Table: Key Reagents for Biosensor Calibration and Validation Experiments
| Reagent / Material | Function | Example & Notes |
|---|---|---|
| Capture Antibody | Binds the target analyte specifically to the solid phase (plate or sensor). | Monoclonal HER2 antibody [93]. Critical for assay specificity. |
| Detection Antibody | Binds a different epitope on the captured analyte, enabling detection. | Biotinylated polyclonal antibody; allows signal amplification [35]. |
| Magnetic Nanoparticles | Magnetic tags for detection in magnetonanosensors. | Streptavidin-coated nanoparticles; provide a matrix-insensitive signal [35]. |
| Chromatographic Column | Separates analytes from matrix components in LC-MS/MS. | Phenomenex Luna C18 column [89]. Choice of column is analyte-dependent. |
| Solid-Phase Extraction (SPE) Cartridge | Extracts and concentrates analytes from complex samples while removing interfering matrix. | Used for environmental water samples [90]; applicable to biological fluids. |
| Stable Isotope-Labeled Internal Standard | Corrects for sample loss during preparation and ion suppression in MS. | e.g., 13C- or 2H-labeled analyte; essential for accurate LC-MS/MS quantification [90]. |
| ELISA Plate | Solid surface for antibody binding and the immunoassay reaction. | Polystyrene plates with high protein-binding capacity. Not tissue culture plates [86] [87]. |
| Blocking Agent | Prevents nonspecific binding of proteins to the assay surface. | Bovine Serum Albumin (BSA) or casein dissolved in PBS [87]. |
Signaling Pathways and Experimental Workflows
ELISA Sequential Steps
LC-MS/MS Analysis Process
Biosensor Validation Logic
Long-Term Stability Assessment and Recalibration Requirements
Frequently Asked Questions (FAQs)
Q1: What are the most common factors that degrade biosensor performance over time? Biosensor performance degrades due to a combination of factors affecting the biological and physico-chemical components. The biological recognition element (e.g., enzymes, antibodies) can denature or lose activity, a process known as biofouling, where nonspecific adsorption of proteins or other molecules from complex samples blocks the active sensing surface [94] [2]. The transducer component is also susceptible to signal drift caused by environmental variability such as temperature fluctuations, changes in pH, and humidity, which can corrode components or alter their electrical properties [94] [95].
Q2: How can I determine the optimal recalibration frequency for my biosensor? The optimal recalibration frequency is not universal and must be determined empirically for your specific application. Key factors to consider are the sensor's inherent drift rate and the required accuracy of your measurements [94]. For applications demanding high precision, such as clinical diagnostics, frequent calibration might be necessary [4]. The sensor's operational history, including exposure to harsh conditions or complex sample matrices that accelerate fouling, will also necessitate more frequent recalibration [94] [2]. Establishing a routine schedule based on initial stability tests and monitoring for signs of signal attenuation is recommended.
Q3: What is the difference between recalibration and validation? Recalibration is the active process of adjusting the biosensor's output by measuring its response to known standard concentrations and updating the calibration function to restore accuracy [96]. Validation, conversely, is the process of verifying that the sensor's measurements fall within an acceptable error margin against a reference method without making any adjustments to the sensor itself [4]. Regular validation checks can help determine when a formal recalibration is needed.
Q4: My biosensor shows unstable readings in complex samples like blood or wastewater. What can I do? Instability in complex samples is often due to matrix effects and biofouling. Strategies to mitigate this include:
- Sample Pre-treatment: Simple dilution, filtration, or centrifugation can reduce interferents [2].
- Surface Engineering: Using anti-fouling coatings (e.g., polyethylene glycol) on the sensor surface can minimize nonspecific binding [43] [2].
- Advanced Biosensor Design: Employ ratiometric or self-calibrating biosensor designs. These devices have built-in reference signals that automatically correct for matrix effects and environmental variability, significantly improving reliability in complex samples [43] [6].
Q5: What are the best practices for storing biosensors to maximize their shelf life? Proper storage is critical for preserving the activity of the biological element. Best practices include storing biosensors in a dry, dark environment at controlled, cool temperatures (often 4°C) to slow down enzymatic degradation and microbial growth [97]. The storage solution should be specified by the manufacturer, which is typically a pH-buffered solution that maintains the biorecognition element's stability. Always refer to the manufacturer's instructions for specific storage conditions [2].
Troubleshooting Guides
Problem 1: Gradual Signal Drift
Symptoms
- A consistent downward or upward trend in the baseline signal over time, even when measuring a standard or blank solution.
- Decreasing sensitivity (slope of the calibration curve).
Diagnosis and Solutions
| Potential Cause | Diagnostic Steps | Corrective Actions |
|---|---|---|
| Biological Component Degradation [97] | Check sensor age and storage history. Perform a fresh calibration and note sensitivity loss. | Recalibrate the sensor. If sensitivity is not restored, replace the biosensor or its biological element. Ensure proper storage conditions. |
| Transducer Fouling [94] [2] | Inspect the sensor surface for visible deposits. Compare signal stability in buffer vs. complex samples. | Clean the sensor surface according to manufacturer protocols (e.g., gentle polishing, enzymatic cleaning). Use anti-fouling agents in the sample or on the sensor surface. |
| Environmental Variability [94] | Monitor laboratory temperature and humidity. Check for drafts or proximity to heat sources. | Perform measurements in a climate-controlled environment. Use biosensors with built-in temperature compensation [43]. |
Problem 2: Loss of Sensitivity and Selectivity
Symptoms
- Reduced response to the target analyte.
- Increased response to non-target substances (cross-sensitivity).
Diagnosis and Solutions
| Potential Cause | Diagnostic Steps | Corrective Actions |
|---|---|---|
| Deactivation of Biorecognition Element [97] [11] | Test with a high-concentration standard. A low maximum response indicates deactivation. | Replace the biosensor cartridge or membrane. For lab-built sensors, re-immobilize the enzyme, antibody, or DNA probe. |
| Sensor Surface Contamination [2] | Visually inspect the sensor. Run a calibration curve; a non-linear response at high concentrations can indicate fouling. | Implement a rigorous cleaning regimen between measurements. For electrochemical sensors, apply conditioning potentials. |
| Matrix Interference [11] [6] | Spike a known analyte concentration into the sample matrix and check for recovery. | Incorporate a sample purification or dilution step. Switch to a biosensor with a different recognition element that is less prone to the specific interferents. |
Experimental Protocols for Stability Assessment
Protocol 1: Accelerated Shelf-Life Testing
Purpose: To predict the long-term storage stability of a biosensor. Principle: By exposing the biosensor to elevated temperatures, the degradation processes are accelerated, allowing for a quicker estimation of shelf life. Materials:
- Biosensors from the same production batch
- Controlled temperature incubators (e.g., 4°C, 25°C, 37°C)
- Standard analyte solutions for calibration
- Data recording system
Methodology:
- Baseline Measurement: Calibrate a set of biosensors (n≥3) and record their initial sensitivity (e.g., slope of the calibration curve) and response time. Store them according to recommended conditions.
- Accelerated Aging: Divide the biosensors into groups. Store each group at different elevated temperatures (e.g., 25°C, 37°C) for a defined period (e.g., 1, 2, 4 weeks).
- Periodic Testing: At predetermined time intervals, remove biosensors from each storage condition, allow them to equilibrate to room temperature, and perform a full calibration.
- Data Analysis: Plot sensitivity and response time against storage time for each temperature. Use models like the Arrhenius equation to extrapolate degradation rates and predict stability at standard storage temperatures (e.g., 4°C).
Protocol 2: Operational Stability and Recalibration Scheduling
Purpose: To determine the biosensor's stability during continuous or repeated use and establish a recalibration schedule. Materials:
- Biosensor and its reader unit
- Standard solutions of known concentrations (Low, Medium, High)
- Complex sample matrix (e.g., serum, wastewater)
- Timer and data sheet
Methodology:
- Initial Calibration: Perform a full calibration curve using standard solutions.
- Continuous or Repeated Measurement: Operate the biosensor continuously in a flow-through system or take repeated measurements at fixed intervals (e.g., every 30 minutes for 8 hours).
- Drift Monitoring: For continuous operation, record the baseline signal and the signal from a standard solution introduced periodically.
- Data Analysis: Calculate the coefficient of variation (CV) for repeated measurements of the same standard. Plot signal vs. time to visualize drift. A common acceptance criterion is a CV < 5-10% and a drift of less than 5% of the signal per hour. The point at which these thresholds are exceeded defines the required recalibration interval.
Key Research Reagent Solutions
The following table details essential materials and their functions for developing and calibrating robust biosensors.
| Reagent/Material | Function in Biosensor Development & Calibration |
|---|---|
| Reference Standard Solutions [11] | Used to construct the calibration curve. Their known, precise concentrations are essential for determining the accuracy of the biosensor. |
| Immobilization Matrices (e.g., Nafion, PEG, Hydrogels) [7] [2] | Entrap or covalently bind the biological element (enzyme, antibody) to the transducer surface, crucial for stability and reusability. |
| Enzyme Inhibitors/Activators [11] | Used in selectivity tests to confirm the biosensor's response is specific to the target analyte and not influenced by other sample components. |
| Blocking Agents (e.g., BSA, Casein) [2] | Applied to the sensor surface to cover any non-specific binding sites, thereby reducing background noise and interference from complex samples. |
| Ratiometric Probes (e.g., dual-emission dyes) [6] | Provide an internal reference signal that self-calibrates for environmental fluctuations and matrix effects, greatly enhancing accuracy. |
Stability Assessment and Calibration Workflows
Biosensor Calibration and Validation Workflow
The following diagram illustrates the core iterative process for establishing and maintaining biosensor accuracy through calibration and validation.
Troubleshooting Signal Instability
This decision tree guides the systematic diagnosis of common signal instability issues.
FAQs on Fundamental Statistical Concepts
Q1: What is the difference between accuracy and precision in the context of biosensor calibration?
Accuracy refers to how close a sensor's measurement is to the true or target value. Precision, on the other hand, refers to the consistency and repeatability of measurements when the same quantity is measured multiple times. A sensor can be precise (giving similar results each time) but not accurate (all results are far from the true value), and vice versa [98]. In calibration, both are crucial; accuracy ensures correct concentration readings, while precision ensures reliability across repeated tests.
Q2: Is a high R² value sufficient to validate my calibration curve?
No, a high R² value alone is not sufficient to validate a calibration curve. While R² indicates the proportion of variance in the response variable explained by the model, it does not guarantee the model's adequacy or accuracy [99]. It is recommended to also use the standard error of the estimate (s) and residual plots for qualitative assessment. The s value, which has the same unit as the response, is a particularly useful criterion. Furthermore, the Prediction Sum of Squares (PRESS) statistic should be used to compare the prediction ability of different calibration models [99].
Q3: My sensor responses are non-linear. What are my options for a calibration model?
Linear and polynomial equations are common, but many biosensor responses are inherently non-linear [99]. You should consider several forms of calibration equations and select the best based on statistical criteria. Suitable non-linear models can include:
- Exponential Rise to Maximum [99]
- Power Equations [99]
- Hill-Langmuir Isotherm (for affinity-based biosensors) [20]
- Logarithmic Transformations of the response or concentration to stabilize non-constant variance [99]
Q4: How can I handle non-constant variance (heteroscedasticity) in my calibration data?
Heteroscedasticity, where the variance of measurement data increases with concentration, is common. A weighted regression can address this problem. The weights are typically calculated using the reciprocal standard deviation of the error for the measurement data at each concentration [99]. However, this requires multiple replicates at each concentration level (more than nine samples are recommended for validity) [99]. Alternatively, a logarithmic transformation of the response can be used to stabilize the variance [99].
Troubleshooting Guides
Issue 1: High Device-to-Device Variation in Sensor Array
Problem: Significant device-to-device variation in a sensor array makes quantitative analysis difficult and unreliable [100] [18].
Solution: Implement a physics-based calibration method to suppress variation.
- Root Cause: Inherent non-uniformity in material synthesis and device fabrication, leading to variations in properties like conductance and transconductance [100] [18].
- Actionable Steps:
- Identify the Sensing Mechanism: Confirm the dominant sensing mechanism (e.g., electrostatic gating for nanowire FET sensors) [100].
- Discover Correlation: Find a correlation between the absolute sensor response (e.g., ΔI) and a fundamental device property (e.g., gate dependence, dI~ds~/dV~g~) [100].
- Apply Calibration: For each device, divide the absolute response by the identified device property (e.g., dI~ds~/dV~g~). This calibrated response will show markedly reduced variation across devices [100].
- Advanced/Alternative Approach: Leverage the sensor redundancy and variation within a large array itself. Use machine learning models (e.g., Random Forest algorithm) trained on multi-dimensional information from the entire multiplexed sensor array to enhance functionality and accuracy in classification and quantification, effectively using the variation to an advantage [18].
Issue 2: Poor Accuracy Due to Nonspecific Binding in Complex Samples
Problem: Label-free biosensor assays in complex media like serum suffer from nonspecific binding (NSB) of matrix constituents, leading to inaccurate readings [101].
Solution: Use an optimized reference (negative control) probe and subtraction method.
- Root Cause: Nonspecific interactions (electrostatics, hydrogen bonding, van der Waals) between serum proteins and the sensor surface or bioreceptor [101].
- Actionable Steps:
- Select a Panel of Candidate Controls: Assay performance can be subtle and analyte-specific. Test a panel of negative control probes. Common choices include [101]:
- Isotype-matched control antibody
- Bovine Serum Albumin (BSA)
- Non-matched isotype controls
- Anti-fluorescein isothiocyanate (anti-FITC)
- Cytochrome c (a charged non-antibody protein)
- Systematic Analysis: Evaluate control probes using bioanalytical parameters of linearity, accuracy, and selectivity to determine the optimal control for your specific assay and analyte [101].
- Reference Subtraction: Immobilize the capture probe and the optimal negative control probe on the same sensor chip. Subtract the signal from the reference channel from the active capture channel to faithfully report the specific binding signal [101].
- Select a Panel of Candidate Controls: Assay performance can be subtle and analyte-specific. Test a panel of negative control probes. Common choices include [101]:
Issue 3: Sensor Drift and Environmental Dependence in Real-Time Monitoring
Problem: Sensor calibration is affected by environmental factors like temperature and sample matrix age, compromising the accuracy of real-time, in-situ measurements [20].
Solution: Calibrate under conditions that match the measurement environment as closely as possible.
- Root Cause: Environmental factors (temperature, pH, ionic strength) influence sensor parameters such as binding affinity (K~1/2~), cooperativity (n~H~), and signal gain (KDM~max~) [20].
- Actionable Steps:
- Match Temperature: Always collect calibration curves at the same temperature used during measurements (e.g., body temperature for in-vivo sensing). Temperature shifts can significantly alter the calibration curve and lead to substantial concentration underestimates or overestimates [20].
- Use Fresh Calibration Matrix: For in-vivo measurements, calibrate using the freshest possible blood. Blood age impacts the sensor response, and commercially sourced aged blood can yield different signal gain [20].
- Validate with Proxy Media: If using a convenient proxy medium (e.g., buffer), validate its performance against the gold-standard matrix (e.g., fresh whole blood) to ensure quantification accuracy [20].
Essential Metrics for Calibration Curve Assessment
The following table summarizes key metrics for evaluating the quality of your calibration model. R² should not be used in isolation [99].
| Metric | Description | Interpretation and Use |
|---|---|---|
| R² (Coefficient of Determination) | Proportion of variance in the response explained by the model. | Insufficient alone. A high value does not guarantee model adequacy. Can be misleading [99]. |
| s (Standard Error of the Estimate) | Average distance that the observed values fall from the regression line. Same units as the response. | Primary criterion for fit. A lower value indicates a better fit. More reliable than R² [99]. |
| Residual Plots | Graph of residuals (observed - predicted) vs. predicted values or concentration. | Qualitative criterion. Used to check for non-linearity, heteroscedasticity, and outliers. Should show random scatter [99]. |
| PRESS (Prediction Sum of Squares) | Measure of a model's prediction ability. | Criterion for prediction performance. A lower PRESS statistic indicates better predictive ability [99]. |
| Accuracy | Closeness of a measurement to the true value. | For biosensors, aim for better than ±10% in complex samples like whole blood [20]. |
| Precision (Coefficient of Variation) | Consistency of repeated measurements. | Reported as CV (100 * standard deviation / mean). Should be as low as possible (e.g., <14%) [20]. |
Experimental Protocol: Theory-Guided RNN for Dynamic Biosensor Calibration
This protocol is adapted from a study on improving biosensor accuracy and speed using dynamic signal change and theory-guided deep learning [102].
1. Objective: To rapidly and accurately quantify target analyte concentration (e.g., microRNA) using the initial transient dynamic response of a biosensor, thereby reducing time delay and minimizing false results.
2. Materials and Reagents:
- Biosensor Platform: Cantilever biosensors with a gold pad for functionalization [102].
- Biorecognition Element: Thiolated-DNA probe specific to the target microRNA (let-7a) [102].
- Analyte: Target microRNA (let-7a) in standard solutions across a wide concentration range (nM to fM) [102].
- Flow Cell: A custom flow cell for continuous buffer flow and sample introduction [102].
3. Procedure:
- Step 1: Sensor Functionalization. Immobilize the thiolated-DNA probe on the gold pad of the cantilever biosensor by continuous flow of a probe solution in the flow cell [102].
- Step 2: Dynamic Response Data Acquisition. For each standard solution, record the biosensor's dynamic response (e.g., resonant frequency shift, Δf, vs. time, t). Ensure data acquisition captures the initial transient phase [102].
- Step 3: Data Preprocessing & Augmentation.
- Structure the data, considering target analyte concentration as a categorical variable.
- Perform data augmentation (e.g., using jittering and scaling) to address data sparsity and class imbalance common in calibration data [102].
- Step 4: Model Training with Theory-Guiding.
- Construct a Recurrent Neural Network (RNN) classifier.
- Implement cost function supervision based on the consistency of model predictions with the theory of surface-based biosensors. This ensures predictions are explainable and physically plausible [102].
- Step 5: Validation.
- Validate the Theory-Guided RNN (TGRNN) classifier using separate test data.
- Evaluate performance using F1 score, precision, and recall to quantify accuracy and the probability of false-negative and false-positive results [102].
Experimental Workflow Diagram
Research Reagent Solutions for Biosensor Calibration
This table details key reagents and materials used in the featured experiments for calibrating biosensors in complex samples.
| Item | Function/Application in Calibration |
|---|---|
| Ion-Selective Membranes (ISMs) | Functionalization chemistry for graphene transistor arrays to confer selectivity towards specific ions (K+, Na+, Ca²⁺) in complex solutions [18]. |
| Isotype-Matched Control Antibodies | Optimal reference (negative control) probes for label-free biosensors to correct for nonspecific binding in complex media like serum [101]. |
| Saturated Salt Solutions | Used to generate standard relative humidity (RH) environments for the calibration of RH sensors, demonstrating principles of fixed-point calibration [103]. |
| Fresh Whole Blood | The gold-standard calibration matrix for in-vivo electrochemical aptamer-based sensors; ensures accuracy by matching the measurement matrix and temperature [20]. |
| Thiolated-DNA Probe | Biorecognition element immobilized on cantilever biosensors for specific capture of target microRNA, enabling dynamic response measurement [102]. |
Regulatory Considerations for Clinical and Diagnostic Applications
Frequently Asked Questions (FAQs)
Q1: Why is calibration so critical for biosensors used in clinical diagnostics? Accurate calibration is fundamental because it establishes the relationship between the biosensor's signal and the analyte concentration, directly impacting diagnostic reliability. Inaccurate calibration can lead to false positives or false negatives, which in a clinical setting can result in misdiagnosis, inappropriate treatment, and serious risks to patient safety [104] [19]. Calibration compensates for device-to-device variations, sensor drift over time, and interference from complex sample matrices, ensuring results are both precise and reproducible [100] [5].
Q2: What are the common causes of false results in biosensor diagnostics? False results can arise from multiple sources. False positives may be caused by non-specific binding of interfering substances, cross-reactivity of the bioreceptor, or contamination of the sample or sensor surface [19]. False negatives often result from the hook effect (analyte concentration exceeding the sensor's dynamic range), degradation of the biological recognition element (e.g., enzymes or antibodies), or the presence of inhibitors in the sample matrix that block the sensing reaction [19]. Proper sample preparation and rigorous calibration are key to mitigating these risks.
Q3: How does complex sample preprocessing improve biosensor accuracy? Complex clinical and food samples contain substances like proteins, fats, and salts that can interfere with biosensor signals. Preprocessing steps, such as filtration, separation, or dilution, are essential to remove these interferents and isolate the target analyte. For example, a filter-assisted system was shown to separate bacteria from food residues, enabling a detection limit of 10¹ CFU/mL for pathogens like E. coli O157:H7 in various food matrices, which would not be possible with raw samples [105]. This step reduces nonspecific signals and is often a prerequisite for reliable detection.
Q4: What is the role of a reference sensor in a biosensing system? A reference sensor is used to monitor and correct for environmental noise and non-specific signals that are not related to the target analyte. For instance, in a flow-through system using optical sensors, a reference oxygen "optrode" can detect and compensate for signal changes caused by temperature fluctuations, bacterial growth, or variations in oxygen concentration, thereby isolating the specific signal produced by the target analyte [7]. This significantly improves the robustness and accuracy of measurements in complex, real-world samples.
Troubleshooting Guides
Problem 1: Inconsistent Results and High Device-to-Device Variation
- Symptoms: Significant differences in signal output or calculated concentrations between sensors of the same type, even when measuring identical samples.
- Possible Causes:
- Solutions:
- Implement Advanced Calibration Protocols: Move beyond simple normalization. For nanosensors, use a calibration method that leverages the correlation between the absolute sensor response (ΔI) and the gate dependence (dI~ds~/dV~g~). Dividing the absolute response by the gate dependence for each device can suppress variation, reducing the coefficient of variance (CV) significantly [100].
- Use Multi-Point Calibration: Always perform at least a 2-point calibration using standard solutions that bracket the expected sample concentration range. A 1-point calibration is insufficient for most quantitative applications [106] [107].
- Validate with Certified Reference Materials (CRMs): Regularly test your calibrated biosensor against CRMs to verify the accuracy of the entire analytical process [107].
Problem 2: Signal Drift or Slow Response Time
- Symptoms: The sensor output does not stabilize or continuously drifts over time during measurement; the time to reach a stable signal is excessively long.
- Possible Causes:
- Sensor Aging or Fouling: The biological element may be degrading, or the transducer surface may be coated with contaminants from complex samples [85] [5].
- Improper Storage: Allowing the biosensor probe to dry out can permanently damage it [106].
- Unstable Environmental Conditions: Fluctuations in temperature or buffer ionic strength can affect sensor performance [7].
- Solutions:
- Routine Maintenance and Cleaning: Follow manufacturer guidelines for cleaning. This may involve soaking the sensor in mild acids (e.g., 0.1M HCl), bleach solutions, or specific enzymatic cleaners to remove debris and biofilms [106].
- Proper Storage: Always store biosensor probes in the recommended storage solution (often a pH 4 buffer) and never let them dry out [5] [106].
- Incorporate a Reference Sensor: As discussed in FAQ A4, use a reference sensor in flow-through systems to correct for drift caused by environmental factors [7].
- Check Sensor Age: Biosensor probes have a finite lifespan (typically 12-18 months). An old electrode will have a slower response and may need replacement [106].
Problem 3: Poor Accuracy in Complex Sample Matrices
- Symptoms: The biosensor performs well with standard solutions in clean buffers but fails to accurately quantify analytes in real samples like blood, serum, or food homogenates.
- Possible Causes:
- Solutions:
- Integrate Sample Preparation: Develop a robust preprocessing step. For pathogen detection in food, a filter-assisted sample preparation (FASP) method can separate target bacteria from food residues, drastically improving accuracy [105]. The table below summarizes other techniques.
- Use the Standard Addition Method: This calibration technique involves adding known quantities of the analyte directly to the sample. It accounts for matrix effects by measuring the response within the sample itself, making it highly reliable for complex matrices [107].
- Match Calibration and Sample Conditions: Prepare your calibration standards in a matrix that mimics the sample as closely as possible (e.g., synthetic urine, artificial serum) [107].
Problem 4: Calibration Failure or Out-of-Range Error
- Symptoms: The instrument refuses to accept the calibration, or the calculated slope and zero point are outside the acceptable range.
- Possible Causes:
- Use of Expired or Contaminated Buffers: Buffer solutions have a limited shelf life and can absorb CO₂ from the air, altering their pH [106].
- Physical Sensor Damage: Cracks in the glass membrane or a clogged reference junction [106].
- Low Electrolyte Level: In refillable electrodes, the electrolyte level can be too low [106].
- Solutions:
- Use Fresh, Unexpired Buffers: Always use fresh, unused buffers for calibration. Never reuse buffers from a previous calibration [106].
- Inspect for Damage: Visually inspect the sensor for any cracks, chips, or leaks. Replace the sensor if physical damage is found [5].
- Check Electrolyte and Temperature Probe: For refillable electrodes, ensure the electrolyte level is correct. Also, verify that the instrument's temperature probe is functioning, as an inaccurate temperature reading will lead to a faulty slope calculation [106].
Experimental Protocols for Complex Samples
Protocol 1: Filter-Assisted Sample Preparation for Pathogen Detection
This protocol is adapted from a study on detecting foodborne pathogens and demonstrates a key preprocessing step for complex matrices [105].
- Objective: To separate and concentrate bacterial cells from complex food matrices (e.g., vegetables, meat, cheese brine) for subsequent detection with an immunoassay-based biosensor.
- Materials:
- Stomacher or homogenizer.
- Double filtration system: Primary filter (e.g., GF/D) and secondary cellulose acetate filter (0.45 μm pore size).
- Vacuum pump.
- Appropriate enrichment broth or buffer.
- Procedure:
- Homogenize: Weigh 25 g of the food sample and homogenize it with 225 mL of a suitable buffer using a stomacher for 1-2 minutes.
- Primary Filtration: Pass the homogenate through the primary filter under vacuum. This step removes large particulate matter and food residues.
- Secondary Filtration: Pass the filtrate from step 2 through the 0.45 μm secondary filter. This step captures the target bacteria on the filter surface.
- Recovery: Recover the bacteria from the secondary filter (e.g., by back-flushing or dissolving the filter) into a small, defined volume of buffer.
- Analysis: The resulting solution, now significantly free of matrix interferents, can be applied to the biosensor. This method achieved a detection limit of 10¹ CFU/mL for target pathogens after a total preprocessing time of under 3 minutes [105].
Protocol 2: Standard Addition Calibration in Complex Liquids
This method is recommended when analyzing samples with significant matrix effects [107].
- Objective: To accurately determine the concentration of an analyte in a complex sample by accounting for matrix-induced signal modulation.
- Materials:
- Biosensor and readout instrument.
- Stock standard solution of the analyte with known, high concentration.
- Identical, aliquoted samples of the unknown complex matrix.
- Procedure:
- Divide the sample into four equal aliquots.
- To three of the aliquots, add increasing, known volumes of the analyte stock standard. The fourth aliquot is left unspiked.
- Dilute all aliquots to the same final volume.
- Measure the biosensor response for each of the four solutions.
- Plot the measured signal versus the added analyte concentration. The line of best fit is extrapolated to the left until it intercepts the x-axis. The absolute value of this x-intercept gives the concentration of the analyte in the original, unspiked sample.
Research Reagent Solutions and Essential Materials
The following table lists key reagents and materials crucial for successful biosensor calibration and operation in complex sample analysis.
| Item | Function/Brief Explanation |
|---|---|
| Certified Reference Materials (CRMs) | Solutions with a certified concentration of the analyte, used for method validation and verifying calibration accuracy [107]. |
| High-Purity Buffer Solutions | Used for sample reconstitution, dilution, and calibration. They provide a stable pH and ionic strength background. Must be fresh and unexpired [106] [107]. |
| Filter Membranes (various pore sizes) | For sample preprocessing to remove particulate interferents and, in some cases, to capture and concentrate the target analyte [105]. |
| Immobilization Reagents | Chemicals (e.g., glutaraldehyde, EDC/NHS) used to covalently attach biological recognition elements to the transducer surface, ensuring stability and reusability [7]. |
| Reference Electrode / Substance | Provides a stable, known potential for electrochemical biosensors, allowing for the calibration of the working electrode's response [7] [107]. |
| Cleaning & Storage Solutions | Specific solutions (e.g., 0.1M HCl, 1:1 bleach water, pH 4 storage buffer) for maintaining sensor integrity, preventing fouling, and ensuring a long operational lifetime [106]. |
Workflow and Relationship Diagrams
Biosensor Calibration and Validation Workflow
Conclusion
Effective biosensor calibration in complex samples requires an integrated approach that combines robust foundational principles with advanced methodological innovations. The convergence of genetically engineered biological components, self-calibrating architectures, and computer-assisted systems represents the future of reliable biosensing in biomedical applications. As the field advances, the integration of machine learning for automated calibration, development of multi-analyte sensing platforms, and creation of standardized validation protocols will be crucial for translating laboratory biosensors into clinically validated tools. These advancements will ultimately enhance their reliability in critical applications such as therapeutic drug monitoring, disease diagnostics, and personalized medicine, bridging the gap between technical innovation and practical clinical implementation.
References
- 1. Introduction to biosensors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4986445/]
- 2. A Closer Look at Biosensors: A Practical Tutorial for ... [https://www.spectroscopyonline.com/view/a-closer-look-at-biosensors-a-practical-tutorial-for-spectroscopists]
- 3. Advances in biosensors: Principle, architecture and ... [https://www.sciencedirect.com/science/article/abs/pii/S1214021X13000082]
- 4. Leveraging biosensors in clinical and research settings [https://www.nature.com/articles/s44277-025-00037-w]
- 5. How to Troubleshoot pH Biosensor Problems in 6 Steps [https://www.linkedin.com/advice/1/what-do-you-your-ph-biosensors-working-properly-zkpkf]
- 6. MOF-based ratiometric fluorescent biosensors for selective ... [https://pubmed.ncbi.nlm.nih.gov/41028285/]
- 7. Calibrating Biosensors in Flow-Through Set-Ups: Studies ... [https://www.intechopen.com/chapters/43507]
- 8. On the Determination of Uncertainty and Limit of Detection in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6068557/]
- 9. Detection limits of chemical sensors: Applications and ... [https://www.sciencedirect.com/science/article/abs/pii/S0925400512006466]
- 10. How to Characterize Limit of Detection (LOD) and Dynamic ... [https://eureka.patsnap.com/report-how-to-characterize-limit-of-detection-lod-and-dynamic-range-for-resonant-biosensors]
- 11. Validation and calibration of a novel GEM biosensor for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10709830/]
- 12. Triple-mode biosensing strategies: A critical review of ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25023550]
- 13. Key Points to Remember When Using Internal Standards ... [https://www.spectroscopyonline.com/view/key-points-to-remember-when-using-internal-standards-for-sample-analysis-by-icp-oes]
- 14. Addressing the Selectivity of Enzyme Biosensors: Solutions and Perspectives - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8123588/]
- 15. Machine learning-based prediction and interpretation of ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25030048]
- 16. Reduction of Biosensor False Responses and Time Delay Using Dynamic Response and Theory-Guided Machine Learning - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10683760/]
- 17. A Review on Xanthine Oxidase-Based Electrochemical ... [https://www.mdpi.com/2227-9040/13/5/159]
- 18. Integrated biosensor platform based on graphene transistor arrays for real-time high-accuracy ion sensing | Nature Communications [https://www.nature.com/articles/s41467-022-32749-4]
- 19. Biosensors, Artificial Intelligence Biosensors, False Results ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025796/]
- 20. Improved calibration of electrochemical aptamer-based ... [https://www.nature.com/articles/s41598-022-09070-7]
- 21. Design optimization of high-sensitivity PCF-SPR biosensor using... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0330944]
- 22. Smart chemometrics-assisted electrochemical biosensor ... [https://www.sciencedirect.com/science/article/pii/S1452398125002494]
- 23. Matrix Optical Biosensor for Determining YKL-40/CHI3L1— ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562298/]
- 24. Status and trends of biosensor technologies for ... [https://www.frontiersin.org/journals/analytical-science/articles/10.3389/frans.2025.1527655/full]
- 25. Biosensor [https://en.wikipedia.org/wiki/Biosensor]
- 26. Optical biosensors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4986466/]
- 27. Protein, Nucleic Acid, and Nanomaterial Engineering for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293380/]
- 28. Biosensor-Integrated Drug Delivery Systems as New ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9496590/]
- 29. Startup's biosensor makes drug development and ... [https://news.mit.edu/2025/startup-biosensor-makes-drug-development-and-manufacturing-cheaper-0615]
- 30. Programming cell-free biosensors with DNA strand ... [https://www.nature.com/articles/s41589-021-00962-9]
- 31. Biosensors and Bioelectronics | Vol 271, 1 March 2025 [https://www.sciencedirect.com/journal/biosensors-and-bioelectronics/vol/271/suppl/C]
- 32. Robust calibration and quantification of FRET signals using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595091/]
- 33. Overview of Methods and Considerations for Handling ... [https://www.chromatographyonline.com/view/overview-methods-and-considerations-handling-complex-samples]
- 34. Transformative biomedical devices to overcome biomatrix ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566325002477]
- 35. Matrix-insensitive protein assays push the limits of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4165514/]
- 36. Problems of analyzing complex sample design data with ... [https://research.google/pubs/problems-of-analyzing-complex-sample-design-data-with-common-statistical-software-packages/]
- 37. How Do I Perform a Dose-Response Experiment? [https://www.graphpad.com/support/faq/how-do-i-perform-a-dose-response-experiment/]
- 38. Optimal experimental designs for dose–response studies with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4655015/]
- 39. How to Interpret Dose-Response Curves [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/protein-biology/interrogation-protein-pathways/how-to-interpret-dose-response-curves?srsltid=AfmBOoqSZwOq_GD69LiLJONsB774sAwKnpTVN6X92f056NgC3SdpbCt_]
- 40. Nanoparticle-enabled portable biosensors for early ... [https://www.sciencedirect.com/science/article/pii/S2590137025001025]
- 41. Electrochemical Sensors for Heavy Metal Ion Detection in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11190924/]
- 42. Validation and calibration of a novel GEM biosensor for ... [https://pubmed.ncbi.nlm.nih.gov/38066557/]
- 43. Self-calibrated SERS-LFIA biosensor based on AgNF for in ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566325006608]
- 44. Self-calibrating surface-enhanced Raman scattering-lateral ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566323007820]
- 45. Self-calibrating surface-enhanced Raman scattering-lateral ... [https://pubmed.ncbi.nlm.nih.gov/37988777/]
- 46. Surface-enhanced Raman spectroscopy for bioanalysis and ... [https://pubs.rsc.org/en/content/articlehtml/2021/nr/d1nr00708d]
- 47. Challenges and Opportunities in Smart Biosensing for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12455640/]
- 48. Context-Aware Biosensor Design Through Biology-Guided ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12186671/]
- 49. Online autonomous calibration of digital twins using ... [https://www.sciencedirect.com/science/article/abs/pii/S0306261922012521]
- 50. Multianalyte Approach—Including Automated Preparation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12209705/]
- 51. A guide to reducing noise and increasing sensitivity in ... [https://blog.igii.uk/a-guide-to-reducing-noise-and-increasing-sensitivity-in-biosensors]
- 52. Matrix Effect Study and Immunoassay Detection Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6187333/]
- 53. Evaluating and mitigating clinical samples matrix effects on ... [https://www.nature.com/articles/s41598-022-17583-4]
- 54. The Guide to Fixing pH Drift [https://www.phionics.com/2020/11/05/the-guide-to-ph-drift/]
- 55. Sensor Calibration at Ultralow Levels: Challenges and Solutions [https://www.environics.com/2025/07/07/sensor-calibration-at-ultralow-levels-challenges-and-solutions/]
- 56. suppression beyond the thermal limit with nanotransistor... Noise [https://www.nature.com/articles/s41598-020-69493-y?error=cookies_not_supported&code=9d73fc36-e026-4c9d-99fa-6ab79e7d3b67]
- 57. What’s the Most Meaningful Standard for Mass... | Spectroscopy Online [https://www.spectroscopyonline.com/view/what-s-most-meaningful-standard-mass-spectrometry-instrument-detection-limit-or-signal-noise-ratio-0]
- 58. - Signal - to enhancement of silicon nanowires noise ... ratio biosensor [https://pubmed.ncbi.nlm.nih.gov/23937430/]
- 59. Single-Entity Electrochemistry for Digital Biosensing at ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8264825/]
- 60. sciencedirect.com/topics/materials-science/ signal - to - noise - ratio [https://www.sciencedirect.com/topics/materials-science/signal-to-noise-ratio]
- 61. Biosensor nanoengineering: Design, operation, and ... [https://www.sciencedirect.com/science/article/pii/S2666351120300401]
- 62. A novel conductive membrane sensor protection technique ... [https://www.sciencedirect.com/science/article/pii/S2590137023000638]
- 63. AI-Enhanced Surface Functionalization in Biosensors [https://www.sciencedirect.com/science/article/abs/pii/S0165993625003887]
- 64. Recent Advances in Developing Cell-Free Protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12385134/]
- 65. Engineering genetic circuits for dynamic control of central ... [https://www.sciencedirect.com/science/article/abs/pii/S109671762500093X]
- 66. Review Genetic circuits for metabolic flux optimization [https://www.sciencedirect.com/science/article/abs/pii/S0966842X24000040]
- 67. Principles of Genetic Circuit Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4230274/]
- 68. Engineering wetware and software for the predictive ... [https://www.nature.com/articles/s41467-025-64457-0]
- 69. which environmental stressors trigger calibration drift [https://www.clarity.io/blog/which-environmental-stressors-most-often-trigger-calibration-drift-and-necessitate-shorter-calibration-intervals]
- 70. Equipment Calibration: The Ultimate Guide for Managers (2025) [https://f7i.ai/blog/equipment-calibration-isnt-a-chore-its-your-competitive-edge-the-strategic-guide-for-2025]
- 71. Biosensing Strategies to Monitor Contaminants and Additives ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293825/]
- 72. Biosensors, Volume 15, Issue 5 (May 2025) – 69 articles [https://www.mdpi.com/2079-6374/15/5]
- 73. Harnessing the power of biosensors for environmental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11991957/]
- 74. The Example of Blood Glucose Meters [https://www.mdpi.com/2227-9040/13/8/300]
- 75. Advanced Signal Processing (2025/2026) [https://moduler.aau.dk/course/2025-2026/ESNESK1K3?lang=en-GB]
- 76. Advanced Digital Signal Processing module [https://www.sussex.ac.uk/study/modules/postgraduate/2025/102475-advanced-digital-signal-processing]
- 77. Biosensors, Volume 15, Issue 9 (September 2025) [https://www.mdpi.com/2079-6374/15/9]
- 78. Maltose & Glucose [https://www.directsens.com/biosensors/maltoseglucose/]
- 79. Clinical Validation of Biosensors: Protocols That Investors ... [https://medstartups.org/clinical-validation-biosensors-protocols-investors-expect]
- 80. Troubleshooting [https://www.sprpages.nl/troubleshooting]
- 81. Biosensors, Volume 15, Issue 11 (November 2025) [https://www.mdpi.com/2079-6374/15/11]
- 82. 生物物理学 [https://cn.bio-protocol.org/Category.aspx?c=1&fl1=26]
- 83. pH Meter Calibration Problems? Check Out These 12 Tips! [https://www.ysi.com/ysi-blog/water-blogged-blog/2013/04/ph-meter-calibration-problems-check-out-these-12-tips?srsltid=AfmBOopKXocSkzAQzigNVPdfjmULhfWvQFXUUq5ofpdUohZoGTzhvSOo]
- 84. Development and validation of a novel calibration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7616920/]
- 85. Smartphone-Based Biosensors: Current Trends ... [https://www.mdpi.com/2673-4591/106/1/10]
- 86. ELISA Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/elisa-troubleshooting-guide.html]
- 87. Troubleshooting Guide: ELISA [https://www.rndsystems.com/resources/troubleshooting-guide-elisa-development]
- 88. Troubleshooting a Faulty ELISA [https://bitesizebio.com/37935/troubleshooting-faulty-elisa/]
- 89. Development and validation of an LC-MS/MS method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3659617/]
- 90. Development and validation of a green/blue UHPLC-MS ... [https://www.nature.com/articles/s41598-025-15614-4]
- 91. Biosensing solutions for protein measurement in blood ... [https://www.sciencedirect.com/science/article/pii/S0263224125011157]
- 92. Comparing immunoassay and mass spectrometry ... [https://www.sciencedirect.com/science/article/pii/S0306453025001027]
- 93. A Rapid, Non-Invasive Approach to Breast Cancer Screening [https://www.mdpi.com/2079-6374/15/6/386]
- 94. What Are the Challenges in Sensor Calibration? → Question [https://climate.sustainability-directory.com/question/what-are-the-challenges-in-sensor-calibration/]
- 95. Sensor fault diagnosis and calibration techniques in ... [https://www.sciencedirect.com/science/article/abs/pii/S0360132324012071]
- 96. Challenges and Opportunities in Calibrating Low-Cost ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11175279/]
- 97. Stability in biosensors derived from domain map analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11077358/]
- 98. How to Quantify the Performance of a Sensor [https://www.airgradient.com/blog/sensor-performance-precision-reproducibility-accuracy/]
- 99. Evaluation of Calibration Equations by Using Regression ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8780995/]
- 100. A Calibration Method for Nanowire Biosensors to Suppress ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2805439/]
- 101. Everything's under Control: Maximizing Biosensor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11840803/]
- 102. Improving biosensor accuracy and speed using dynamic ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566323007716]
- 103. Determination of Optimal Measurement Points for ... [https://www.mdpi.com/1424-8220/19/5/1213]
- 104. Biomedical Sensor Calibration Procedure Guidelines [https://www.meegle.com/en_us/advanced-templates/bioelectronics/biomedical_sensor_calibration_procedure_guidelines]
- 105. An Integrated System Combining Filter-Assisted Sample ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428675/]
- 106. pH Meter Calibration Problems? Check Out These 12 Tips! [https://www.ysi.com/ysi-blog/water-blogged-blog/2013/04/ph-meter-calibration-problems-check-out-these-12-tips?srsltid=AfmBOoq9_QEiJTwTw8q2_uvB5SjnoVt0hiwfYsYvXulVJsgoHbDJ9Q74]
- 107. How to Calibrate a Biosensor for Environmental Monitoring [https://www.linkedin.com/advice/0/how-can-you-calibrate-biosensor-environmental-monitoring-1lzhc]