Calibration Methods for In-Vivo Biosensing: A Comprehensive Accuracy Comparison for Researchers
This article provides a comprehensive analysis of calibration method accuracy for in-vivo biosensors, a critical determinant of reliability for researchers and drug development professionals.
Calibration Methods for In-Vivo Biosensing: A Comprehensive Accuracy Comparison for Researchers
Abstract
This article provides a comprehensive analysis of calibration method accuracy for in-vivo biosensors, a critical determinant of reliability for researchers and drug development professionals. We explore the foundational challenges necessitating calibration, from sensor drift to biological variability. A detailed comparison of methodological approaches—including one-point, two-point, dual-frequency, and kinetic calibration—is presented, followed by troubleshooting strategies for environmental interference and signal attenuation. The review culminates in validation techniques and direct accuracy comparisons across biosensor platforms, including continuous glucose monitors and electrochemical aptamer-based sensors, offering evidence-based guidance for method selection to enhance data integrity in biomedical research.
The Critical Role and Fundamental Challenges of Biosensor Calibration
Why Calibration is a Significant Hurdle in Clinical Biosensor Adoption
For researchers and scientists developing in-vivo biosensing platforms, calibration is not merely a procedural step but a central determinant of clinical viability. Biosensors, defined as analytical devices that combine a biological recognition element with a physicochemical detector, have shown transformative potential for real-time monitoring of therapeutics and biomarkers directly in the living body [1]. The translation of this potential from laboratory prototypes to clinically adopted tools, however, faces a critical bottleneck: the establishment of robust, reliable calibration methods that maintain accuracy under physiologically dynamic conditions.
The clinical biochemistry laboratory represents an environment where diagnostic accuracy is paramount, with an estimated 75% of medical decisions relying on laboratory results [2]. In this context, any variance in calibration can have profound implications for patient diagnosis and treatment. This review systematically examines calibration as a significant adoption hurdle by comparing the performance of different calibration methodologies under experimental conditions relevant to in-vivo biosensing research, providing researchers with objective data to inform sensor development strategies.
Fundamental Calibration Challenges in Complex Biological Environments
The Clinical Accuracy Imperative
The transition of biosensors from research tools to clinical applications demands rigorous validation against established diagnostic standards. Clinical laboratories typically process millions of assays annually across diverse specialties including biochemistry, microbiology, and molecular biology [2]. For a biosensor to gain acceptance in this environment, its calibration must demonstrate uncompromising reliability when analyzing real clinical samples such as serum, saliva, and urine—matrices known for complex composition and potential interference factors.
A primary challenge lies in minimizing non-specific adsorption (NSA), a phenomenon where biomolecules adhere indiscriminately to sensor surfaces, potentially distorting calibration curves and compromising measurement accuracy [2]. This issue is particularly acute for in-vivo applications where sensors interface directly with complex biological fluids. Furthermore, the conservative nature of clinical adoption means that new biosensing technologies must demonstrate not just equivalence but superiority over entrenched methods from a cost-per-assay standpoint, placing additional pressure on calibration robustness as a key differentiator [2].
Environmental and Biological Matrix Effects
The calibration of biosensors for in-vivo applications must account for dynamic physiological variables that significantly impact sensor performance. Experimental studies have demonstrated that temperature differentials between calibration and measurement conditions introduce substantial error. Research on electrochemical aptamer-based (EAB) sensors revealed that calibration curves differ significantly between room and body temperature, with interrogation at 25 and 300 Hz showing up to 10% higher signal at room temperature across vancomycin's clinical concentration range [3]. This temperature dependency stems from its influence on both binding equilibrium coefficients and electron transfer rates, fundamentally altering sensor response characteristics.
Beyond temperature, the biological matrix itself introduces variability that challenges conventional calibration approaches. Studies comparing calibration in freshly collected versus commercially sourced blood have identified marked differences in sensor response. For vancomycin-detecting EAB sensors, commercially sourced bovine blood yielded lower signal gain compared to freshly collected blood, leading to potential overestimation of drug concentrations [3]. Even blood age significantly impacts sensor response, with 14-day-old blood producing different calibration curves, particularly at target concentrations above the clinical range [3]. These findings underscore the critical importance of matching calibration media to the intended measurement environment—a challenging requirement for in-vivo applications where physiological conditions constantly fluctuate.
Table 1: Impact of Environmental Variables on Biosensor Calibration
| Variable | Experimental Impact | Consequence for Calibration |
|---|---|---|
| Temperature | 10% higher KDM signal at room temperature vs. body temperature [3] | Underestimation of concentrations if calibrated at different temperature |
| Matrix Age | Lower signal gain in aged blood vs. fresh blood [3] | Overestimation of target concentrations |
| Matrix Composition | Differing responses in commercial vs. freshly collected blood [3] | Requires media-specific calibration curves |
| Electron Transfer Rate | Increases with temperature, shifting peak charge transfer [3] | Alters optimal signal-on/off frequency selection |
Comparative Analysis of Calibration Methods for In-Vivo Applications
One-Point In Vivo Calibration
The pursuit of simplified calibration methodologies has led to investigation of one-point calibration approaches, particularly for continuous monitoring applications. Early foundational research on "wired" glucose oxidase electrodes implanted in jugular veins of rats demonstrated the feasibility of one-point in vivo calibration during periods of rapid glucose fluctuation [4]. This method achieved clinically acceptable accuracy with regression analysis yielding a slope of 0.97 ± 0.07 and intercept of 0.3 ± 0.3 mM, with correlation coefficient (r²) of 0.949 ± 0.020 across the 2-22 mM range [4].
The one-point approach leverages a single reference measurement to establish baseline sensor response, assuming stable sensor sensitivity over the monitoring period. This method offers practical advantages for clinical implementation by reducing the need for multiple blood draws or reference measurements. However, its accuracy depends critically on understanding and modeling transient physiological differences between measurement compartments—such as between subcutaneous tissue and blood glucose concentrations—and assumes minimal sensor drift during the monitoring period [4]. For researchers, this approach represents a compromise between practicality and precision, suitable for applications where trends matter more than absolute values.
Multi-Point and Media-Matched Calibration
For applications requiring higher analytical precision, multi-point calibration using media-matched conditions represents the current gold standard. Research with EAB sensors for vancomycin monitoring demonstrates that calibration using freshly collected, undiluted whole blood at body temperature achieves remarkable accuracy of better than ±10% across the drug's clinical concentration range (6-42 µM) [3]. This methodology involves generating a full calibration curve across the expected concentration range using the exact media and temperature conditions encountered during measurement.
The experimental protocol for this approach involves several critical steps: (1) collection of fresh whole blood, (2) maintenance of blood at body temperature (37°C) throughout calibration, (3) sequential dosing with target analyte across the clinically relevant concentration range, and (4) fitting of the response to a Hill-Langmuir isotherm to extract calibration parameters [3]. The resulting calibration curve accounts for matrix effects, temperature dependencies, and binding characteristics specific to the measurement environment. While this approach is logistically challenging, it currently represents the most accurate method for quantifying in vivo biosensor performance in research settings.
Table 2: Performance Comparison of Calibration Methods for In-Vivo Biosensing
| Calibration Method | Experimental Accuracy | Precision | Implementation Complexity |
|---|---|---|---|
| One-Point In Vivo | Slope: 0.97 ± 0.07 [4] | r²: 0.949 ± 0.020 [4] | Low |
| Multi-Point (Media-Matched) | Better than ±10% in clinical range [3] | ≤14% coefficient of variation [3] | High |
| Out-of-Set Calibration | No significant change vs. individual calibration [3] | Slight reduction in precision [3] | Medium |
| Proxy Media Calibration | Varies with media similarity [3] | Dependent on media matching | Medium |
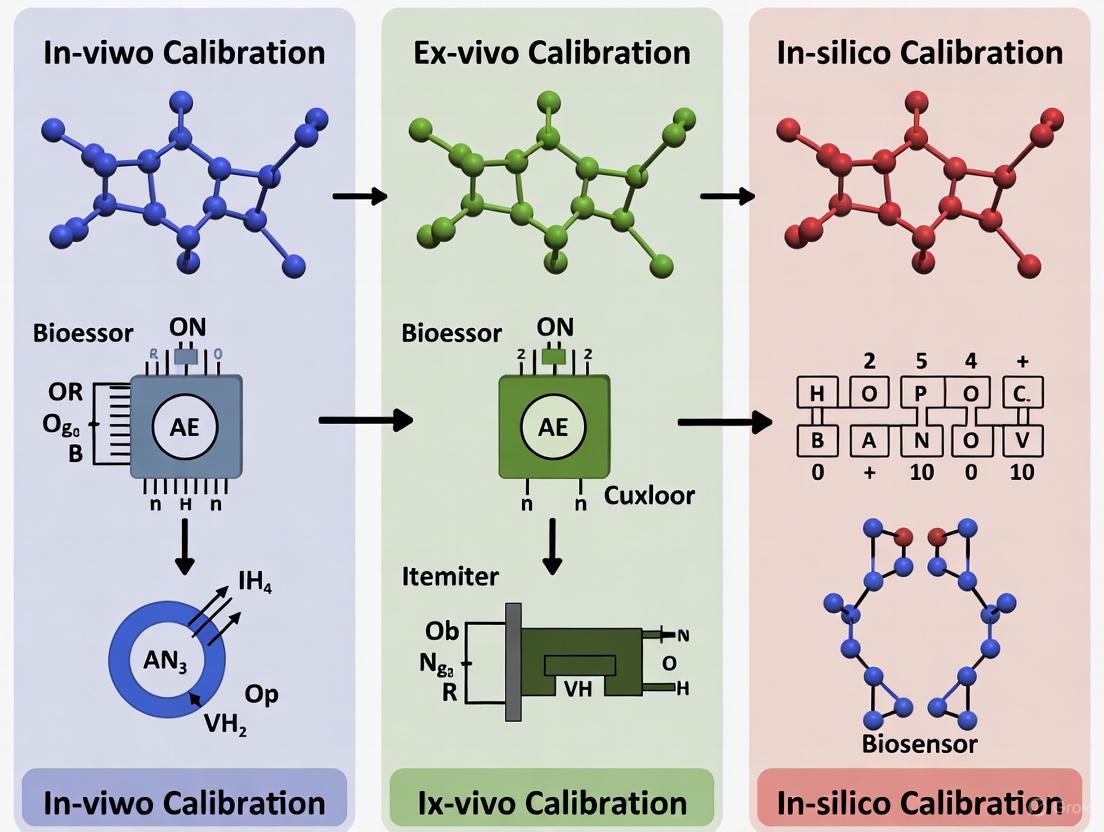
Diagram 1: Media-Matched Calibration Workflow
Advanced and Emerging Calibration Approaches
Kinetic Differential Measurement
The Kinetic Differential Measurement (KDM) approach represents a significant advancement in calibration methodology for addressing signal drift in electrochemical biosensors. This technique involves collecting voltammograms at multiple square wave frequencies—typically both "signal-on" and "signal-off" frequencies—and converting them into normalized KDM values [3]. The mathematical transformation involves subtracting the normalized peak currents observed at signal-on and signal-off frequencies, then dividing by their average [3]. This approach effectively corrects for drift and enhances gain during in vivo measurements by focusing on the kinetic aspects of the sensor response rather than absolute signal magnitude.
The experimental implementation requires careful frequency selection, as temperature changes can alter the optimal signal-on and signal-off frequencies. Research has demonstrated that a frequency functioning as a weak signal-on at room temperature may transition to a clear signal-off frequency at body temperature [3]. The resulting KDM values are fitted to a Hill-Langmuir isotherm to generate calibration parameters according to the equation:
Where nH is the Hill coefficient, K1/2 is the binding curve midpoint, and KDMmin and KDM_max represent the minimum and maximum KDM values [3]. This mathematical framework enables researchers to extract quantitative concentration data from complex in vivo environments.
Calibration-Free and AI-Enhanced Approaches
Emerging research directions focus on reducing or eliminating the need for traditional calibration through innovative technological approaches. Electrochemical DNA-based biosensors are exploring calibration-free operational strategies that leverage predictable binding kinetics and signal patterns to infer concentration without explicit calibration curves [5]. These approaches typically require extensive characterization of sensor behavior across diverse conditions to establish robust computational models.
The integration of artificial intelligence with biosensing represents a promising frontier for addressing calibration challenges. AI algorithms can process complex biosensor outputs and recognize patterns that would be difficult to discern manually, potentially compensating for calibration drift and matrix effects through computational correction [1]. Machine learning approaches can model the relationship between sensor response and target concentration while simultaneously accounting for confounding variables such as temperature fluctuations, pH changes, and interfering substances [6]. These advanced methodologies remain primarily in the research domain but offer potential pathways to simplify calibration requirements for clinical adoption.
Experimental Protocols for Biosensor Calibration
Media-Matched Calibration Protocol
For researchers requiring high-accuracy quantification in vivo, the following experimental protocol for media-matched calibration has demonstrated superior performance in controlled studies [3]:
Fresh Blood Collection: Draw whole blood immediately before calibration (or use preservative-treated blood validated for minimal signal impact). Commercial blood sources should be avoided or validated due to observed differences in sensor response.
Temperature Equilibrium: Maintain blood at 37°C throughout calibration using a precision-controlled heating block or water bath. Temperature control should extend to all fluid handling components.
Sensor Pre-conditioning: Condition sensors in the target matrix without analyte for 30-60 minutes to establish stable baseline signals before calibration.
Sequential Dosing: Introduce target analyte sequentially across the clinically relevant concentration range, allowing sensor stabilization at each concentration point. For vancomycin, this typically spans 0-100 μM.
Signal Acquisition: Collect square wave voltammograms at both signal-on and signal-off frequencies. Optimal frequency pairs should be determined empirically at the calibration temperature.
KDM Calculation: Convert voltammogram peak currents to KDM values using the formula: KDM = (Isignal-off - Isignal-on) / ((Isignal-off + Isignal-on)/2) [3].
Curve Fitting: Fit averaged KDM values to a Hill-Langmuir isotherm to extract KDMmin, KDMmax, K_1/2, and nH parameters.
Validation: Validate calibration parameters using out-of-set samples not included in the original curve fitting.
This protocol, while resource-intensive, has demonstrated accuracy better than ±10% for drug monitoring applications when both calibration and measurement are performed under matched conditions [3].
One-Point Calibration Validation Protocol
For researchers validating one-point calibration approaches, the following methodology provides rigorous assessment:
Reference Measurement: Obtain a precise reference measurement of target concentration using established laboratory methods.
Sensor Measurement: Concurrently record sensor output at the known concentration.
Sensitivity Calculation: Determine sensor sensitivity (signal per unit concentration) from the single point.
Assumption of Linearity: Assume linear response across the clinical range, validated through previous characterization.
Tracking Application: Apply the calculated sensitivity to subsequent sensor measurements.
Accuracy Assessment: Compare sensor estimates with periodic reference measurements to assess calibration stability.
This approach requires thorough preliminary characterization of sensor linearity and drift properties but offers practical advantages for extended monitoring applications.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for Biosensor Calibration
| Reagent/Material | Function in Calibration | Critical Specifications |
|---|---|---|
| Fresh Whole Blood | Physiologically relevant calibration matrix | Collected same day, anticoagulant-treated [3] |
| Temperature-Controlled Chamber | Maintain physiological temperature during calibration | ±0.5°C stability at 37°C [3] |
| Target Analytic Standards | Generation of concentration response curve | Pharmaceutical grade (>95% purity) [3] |
| Hill-Langmuir Fitting Software | Extraction of calibration parameters | Nonlinear regression capabilities [3] |
| Electrochemical Station | Signal acquisition and processing | Square wave voltammetry capability [3] |
| Anti-fouling Coatings | Reduction of non-specific adsorption | PEG-based or zwitterionic polymers [2] |
Calibration remains a significant adoption hurdle for clinical biosensors due to the complex interplay between sensor elements and dynamic physiological environments. The comparative analysis presented here demonstrates that while media-matched multi-point calibration achieves the highest accuracy (>90% in clinical range), it presents substantial practical challenges for routine clinical implementation [3]. One-point calibration offers simplified workflow but depends critically on sensor stability and well-characterized response patterns [4].
For researchers and drug development professionals, the selection of calibration methodology involves balancing analytical requirements with practical constraints. Emerging approaches including kinetic differential measurement, calibration-free strategies, and AI-enhanced signal processing offer promising pathways to reduce the calibration burden while maintaining analytical validity [5] [6] [1]. The ultimate resolution of the calibration hurdle will likely involve continued sensor development alongside computational innovation, creating systems that either resist environmental interference or automatically compensate for it through integrated intelligence.
As biosensor technology continues its trajectory toward clinical adoption, calibration methodologies must evolve from specialized laboratory procedures to robust, standardized protocols that ensure reliability across diverse patient populations and clinical settings. Through continued research focusing on the fundamental challenges outlined in this review, the scientific community can overcome this significant adoption hurdle and realize the full potential of in-vivo biosensing for therapeutic monitoring and personalized medicine.
Addressing Sensor-to-Sensor Fabrication Variation and Signal Drift
For researchers and drug development professionals, achieving high-fidelity data from in-vivo biosensing is often hampered by two persistent technical challenges: sensor-to-sensor fabrication variation and signal drift. Fabrication variation introduces inconsistencies between sensors, compromising the reproducibility of data, while signal drift causes a sensor's output to change over time independently of the target analyte, leading to inaccurate readings. The choice of calibration method is critical to overcoming these hurdles and ensuring data accuracy. This guide objectively compares the performance of emerging calibration strategies—from sophisticated hardware designs to innovative software and material-based approaches—framed within the broader thesis that effective calibration is the cornerstone of reliable in-vivo biosensing research.
Comparative Analysis of Calibration Methods
The table below summarizes the quantitative performance data and key characteristics of contemporary calibration methods designed to mitigate fabrication variation and signal drift.
Table 1: Performance Comparison of Biosensor Calibration Methods
| Calibration Method | Reported Performance Metric | Target Application | Key Advantage for Drift/Fabrication Variation | Experimental Limit of Detection |
|---|---|---|---|---|
| Self-Calibration PEC Platform [7] | Improved stability & anti-interference | In-vitro trypsin detection | Dual-channel differential measurement eliminates common-mode background signal and drift. | Not Specified |
| Skin Surface pH Calibration [8] | MARD decreased from 34.44% to 14.78% | Non-invasive ISF glucose detection | Compensates for drift in ISF extraction caused by variable skin surface pH. | - |
| FRET Standards Calibration [9] | Enables cross-experimental and long-term studies | Live-cell molecular activity imaging | Calibrated FRET ratio is independent of imaging conditions (laser power, detector sensitivity). | - |
| D4-TFT with Rigorous Testing [10] | Achieved attomolar (aM) detection in 1X PBS | Ultrasensitive biomarker detection in point-of-care format | Mitigates signal drift via a stable electrical configuration and infrequent DC sweeps. | Sub-femtomolar to attomolar |
| Calibration-Free eDNA Sensors [5] | Advancements in TDM and personalized therapy | Continuous in-vivo molecular monitoring | Eliminates the need for repeated calibration in complex biological environments. | - |
| Carbon Nanomaterial Platform [11] | Improved signal precision and stability | General biosensor performance | High manufacturability reduces sensor-to-sensor variation; stable signal minimizes drift. | Ultra-low (e.g., femtomolar) |
Detailed Experimental Protocols and Data
Self-Calibration Photoelectrochemical (PEC) Biosensing
This method employs a hardware-based, self-calibration system to address baseline drift and background signal interference simultaneously [7].
- Core Principle: The platform uses two independent PEC test channels—a test channel and a blank channel—processed by a dual-channel data acquisition unit. The signal difference between the two channels is used for quantification, effectively subtracting the background and drift common to both [7].
- Protocol Workflow:
- Probe Preparation: A peptide-recognition element is assembled onto a carbon-rich plasmonic hybrid (C–Mo2C) probe.
- Sensor Assembly: The probe is anchored onto a TiO₂ nanoparticle substrate to form the photoanode. Identical photoanodes are used in both test and blank channels.
- Target Incubation: The target analyte (e.g., trypsin) is introduced only to the test channel. Its interaction causes a change in the probe on the electrode.
- Signal Acquisition & Calibration: Under NIR light, the PEC signals from both channels are recorded simultaneously. The final, calibrated signal is the difference between the blank channel (background/drift) and the test channel (background/drift + target response) [7].
The following diagram illustrates the logical relationship and workflow of this self-calibration system:
Drift Mitigation in Carbon Nanotube (CNT) BioFETs
This approach combines material science with a stringent testing methodology to achieve ultra-stable sensing in biologically relevant ionic strength solutions [10].
- Core Principle: Signal drift in CNT-based field-effect transistors (BioFETs) is mitigated by maximizing sensitivity through passivation, using a stable testing configuration, and relying on infrequent DC sweeps instead of continuous static measurements [10].
- Protocol Workflow:
- Device Fabrication: Create a thin-film transistor using printed CNTs. A non-fouling polymer brush interface (POEGMA) is grown above the device to act as a Debye length extender, allowing detection in high ionic strength solutions [10].
- Antibody Printing: Capture antibodies are printed into the POEGMA layer.
- Control Design: A control device with no antibodies printed over the CNT channel is fabricated and tested alongside the active sensor to confirm specific detection [10].
- Stable Measurement: The D4-TFT device uses a palladium pseudo-reference electrode and a printed circuit board for automated testing. The key to drift mitigation is collecting data via infrequent DC voltage sweeps rather than continuous monitoring at a fixed voltage [10].
Calibration Using FRET Standards
This method is critical for optical biosensors, where fluctuations in imaging parameters can mimic or obscure genuine biosensor responses [9].
- Core Principle: The FRET ratio (acceptor-to-donor signal) is calibrated by imaging engineered "FRET-ON" and "FRET-OFF" standard cells under the same conditions as the experimental biosensor cells [9].
- Protocol Workflow:
- Sample Preparation: A mixed population of cells is prepared, expressing either the biosensor of interest or the calibration standards (FRET-ON and FRET-OFF) [9].
- Cell Barcoding: Cells are labeled with distinct pairs of barcoding proteins (e.g., blue or red FPs targeted to different locations) to allow for multiplexed identification during imaging [9].
- Simultaneous Imaging: All cells—biosensor and both standards—are imaged simultaneously in the same session.
- Signal Normalization: The FRET ratio from the biosensor cells is normalized against the signals obtained from the FRET-ON and FRET-OFF standards. This calibration produces a value independent of laser intensity and detector sensitivity, enabling accurate cross-experimental comparisons [9].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and their functions for implementing the discussed calibration methods.
Table 2: Essential Research Reagents and Materials for Advanced Biosensor Calibration
| Item Name | Function in Experiment | Application Context |
|---|---|---|
| C–Mo2C Carbon-Rich Plasmonic Hybrid [7] | Acts as a photoactive element; enables NIR-driven sensing and provides signal amplification via plasmonic and photothermal effects. | Self-calibration PEC biosensing. |
| Poly(OEGMA) Polymer Brush [10] | Coated on the sensor surface to extend the Debye length and reduce biofouling, enabling detection in physiological fluids. | CNT-BioFETs for point-of-care diagnostics. |
| FRET-ON/FRET-OFF Standard Cells [9] | Genetically encoded calibration standards used to normalize the FRET ratio against variations in imaging conditions. | Live-cell imaging with FRET biosensors. |
| Palladium (Pd) Pseudo-Reference Electrode [10] | Provides a stable reference potential in a miniaturized form factor, replacing bulky Ag/AgCl electrodes. | Portable and point-of-care electrochemical sensors. |
| Bipolar Silica Nanochannel Array Film [12] | Used to stably immobilize ECL emitters like Ru(bpy)₃²⁺, enhancing the stability of solid-phase electrochemiluminescence sensors. | Enzyme-based solid-phase ECL sensors. |
| High-Performance Carbon Nanomaterial [11] | A 3D porous carbon scaffold that provides high surface area, conductivity, and manufacturability, improving sensitivity and reducing sensor-to-sensor variation. | General platform for high-performance electrochemical biosensors. |
The accurate comparison of calibration methods reveals that no single solution is universally superior; the optimal choice is dictated by the specific biosensing platform and research question. Hardware-level self-calibration [7] is powerful for direct drift rejection but adds system complexity. Material-driven approaches [10] [11] address the root causes of variation and drift, offering a more foundational solution that enhances multiple performance metrics simultaneously. For optical biosensors, the use of internal standards [9] is indispensable for quantitative accuracy.
Future research is poised to integrate artificial intelligence to dynamically model and correct for drift in real-time [5] [1]. Furthermore, the convergence of advanced biofabrication techniques [13] with high-precision nanomaterials [11] promises to minimize fabrication variation at the source, ultimately leading to a new generation of robust, calibration-free, and highly reliable biosensors for demanding in-vivo research and drug development applications.
In the field of in-vivo biosensing, the selection of a biological matrix is a fundamental decision that directly influences the accuracy, relevance, and temporal resolution of measurements. Blood has traditionally been the gold standard for clinical diagnostics, providing a direct window into systemic circulation. However, the quest for continuous monitoring and minimally invasive techniques has brought interstitial fluid (ISF) and other biofluids like sweat to the forefront [14] [15]. This guide objectively compares the performance of blood and ISF as biological matrices, focusing on their metabolite dynamics and the implications for sensor calibration and data interpretation. Understanding the kinetic equilibrium and physiological lag between these compartments is critical for developing reliable biosensors for applications ranging from diabetes management to therapeutic drug monitoring and athletic performance [14] [16].
Comparative Analysis of Biological Matrices
The following table summarizes the core characteristics of blood and interstitial fluid as matrices for biosensing.
Table 1: Key Characteristics of Blood vs. Interstitial Fluid for Biosensing
| Characteristic | Blood | Interstitial Fluid (ISF) |
|---|---|---|
| Physiological Role | Systemic transport of gases, nutrients, hormones, and waste products [17]. | Bathes and nourishes cells; medium for exchange between blood and cells [14]. |
| Primary Sampling Method | Venipuncture or fingerprick (invasive) [15]. | Minimally invasive (e.g., subcutaneous sensors, microneedles) [14] [16]. |
| Metabolite Correlation | Gold standard reference [15]. | High correlation for many analytes, but with a physiological time lag [14] [16]. |
| Representativeness | Reflects systemic, whole-body concentration. | Reflects local, tissue-level concentration [17]. |
| Key Advantage | Direct measurement, established clinical reference. | Enables comfortable, continuous monitoring. |
| Key Challenge | Invasiveness limits frequency; unsuitable for real-time tracking. | Dynamic equilibrium with blood introduces calibration complexity [14] [3]. |
Experimental Evidence of Analyte Dynamics
The relationship between blood and ISF glucose has been extensively studied, particularly in the context of Continuous Glucose Monitoring (CGM). Research consistently shows that ISF glucose levels are correlated with blood glucose but exist in a kinetic equilibrium, resulting in a measurable time and magnitude gradient [14].
Table 2: Experimentally Measured Lag Times Between Blood and Interstitial Fluid Glucose
| Study (First Author, Year) | Estimated Lag Time (Minutes) | Study Population | IF Sampling Method |
|---|---|---|---|
| Shichiri M, 1986 [14] | 5 | People with diabetes (n=5) | Transcutaneous sensor |
| Sternberg F, 1996 [14] | 2–12 | People with diabetes (n=40) | Microdialysis |
| Rebrin K, 2000 [14] | 5–12 | Anaesthetised dogs | Transcutaneous sensor |
| Boyne MS, 2003 [14] | 4–10 | People with type 1 diabetes (n=14) | Transcutaneous sensor |
| Steil GM, 2005 [14] | 3–8 | Healthy subjects (n=10) | Transcutaneous sensor |
| Kulcu E, 2003 [14] | 5 | People with type 1 or 2 diabetes (n=51) | Reverse iontophoresis |
For other metabolites, the dynamics can differ. A study on lactate monitoring during aerobic exercise found a strong correlation (ρ = 0.93) between ISF lactate and blood lactate, positioning ISF as a reliable proxy for systemic lactate levels. In contrast, sweat lactate showed a much weaker correlation (ρ = 0.36), highlighting the importance of matrix selection for specific analytes [16].
Metabolomic studies further reveal that ISF can provide a unique signature that differs from blood. An NMR-based analysis of patients with arterial hypertension identified nine potential metabolomic biomarkers in ISF that were distinct from those found in plasma or urine. These ISF-specific biomarkers primarily reflected alterations in lipid and amino acid metabolism and indicated increased levels of local oxidative stress and inflammation [17].
Experimental Protocols for Matrix Comparison
To ensure the accuracy and reliability of comparative data, rigorous experimental protocols must be followed. The following workflow outlines a standardized approach for validating ISF sensor readings against blood references.
Detailed Methodology
Participant Selection and Sample Collection
Studies should recruit a well-defined population (e.g., healthy adults, diabetic patients, or athletes) with approved ethical oversight and informed consent [17] [16]. For dynamic monitoring, samples are collected at synchronized timepoints.
- Blood Collection: Venous or capillary blood is drawn using standard phlebotomy procedures. Plasma is isolated by centrifugation (e.g., 3000× g for 10 min at 4°C) for analysis [17] [3].
- ISF Collection: ISF can be accessed via:
- Continuous Subcutaneous Sensors: Commercial or research-grade CGM systems are implanted according to manufacturer protocols [14].
- Microdialysis: A probe is inserted into the subcutaneous tissue and perfused with a buffer to harvest analytes [14].
- Microneedle Arrays: Patches containing micron-scale needles penetrate the skin barrier to access ISF, often functionalized with biosensing elements [16].
Sample Processing and Metabolite Analysis
- Blood/Plasma: Processed plasma and ISF samples are often analyzed using high-resolution techniques like 1H NMR spectroscopy for broad metabolomic profiling [17]. For specific analytes, targeted biosensing is employed.
- Biosensor Calibration: Electrochemical biosensors, such as Electrochemical Aptamer-Based (EAB) sensors, require careful calibration. A common method involves generating a calibration curve by measuring the sensor response (e.g., Kinetic Differential Measurement values) across a range of target concentrations in a relevant medium (e.g., fresh whole blood). The data is fitted to a Hill-Langmuir isotherm to determine parameters like the binding curve midpoint (K~1/2~) and signal gain, which are used to convert sensor output into concentration estimates [3].
Critical Factors in Experimental Design
- Temperature Control: Sensor response and binding equilibria are temperature-sensitive. Calibration should be performed at the intended measurement temperature (e.g., 37°C for in-vivo studies) to avoid significant quantification errors [3].
- Media Freshness and Composition: The age and source of calibration media (e.g., blood) can impact sensor performance. Using freshly collected blood is superior to aged, commercially sourced blood, as it better replicates the in-vivo environment [3].
- Data Synchronization: Accurate timestamping of all samples is crucial for calculating physiological lag times between blood and ISF analyte changes [14].
The Scientist's Toolkit: Research Reagent Solutions
The following table lists essential materials and their functions for conducting research on blood and ISF metabolite dynamics.
Table 3: Essential Research Reagents and Materials for Matrix Comparison Studies
| Item | Function/Application | Representative Example |
|---|---|---|
| Potentiometric Sensor | Measures ion concentration (e.g., H+, Na+, K+) by detecting changes in electrical potential; commonly used for pH and electrolyte sensing in sweat and ISF [15] [16]. | Ionselective electrodes in wearable patches. |
| Amperometric Sensor | Measures current generated by the redox reaction of an analyte; used for continuous monitoring of metabolites like glucose and lactate [14] [16]. | Enzyme-based (e.g., glucose oxidase) subcutaneous sensors. |
| Single-Walled Carbon Nanotubes (SWCNT) | Nanomaterial scaffold for near-infrared (NIR) optical biosensors; offers high biocompatibility and stable fluorescence for long-term implantable sensing [18]. | NIR fluorescence-based nitric oxide sensors. |
| Electrochemical Aptamer-Based (EAB) Sensor | Combines a target-specific aptamer with an electrochemical reporter; enables real-time measurement of specific molecules (e.g., drugs, metabolites) in undiluted whole blood [3]. | Vancomycin-detecting sensors for therapeutic drug monitoring. |
| Microneedle Array | Minimally invasive platform to access ISF; can be fabricated from polymers (e.g., SU-8) and integrated with biosensing elements for continuous monitoring [16]. | Lactate-sensing microneedle patches for athletic monitoring. |
| High-Resolution NMR Spectroscopy | Non-destructive analytical technique for unambiguous identification and quantification of a wide range of metabolites in biofluids like plasma, ISF, and urine [17]. | 600 MHz NMR for metabolomic fingerprinting of hypertension. |
The choice between blood and interstitial fluid as a biological matrix is not a matter of identifying a superior option, but of selecting the most appropriate one for the specific research or clinical application. Blood remains the indispensable gold standard for definitive, point-in-time measurements. However, for the future of continuous, real-time health monitoring, ISF offers a minimally invasive and information-rich alternative. The key to its successful utilization lies in a deep understanding of the analyte-specific dynamics and time delays that exist between these compartments. Robust, temperature-matched calibration protocols are critical to translate ISF sensor signals into accurate physiological data. As biosensing technologies like microneedles and advanced electrochemical sensors continue to evolve, the simultaneous monitoring of multiple matrices will provide a more holistic and dynamic picture of human physiology, revolutionizing personalized healthcare and athletic performance optimization.
The Impact of Temperature, pH, and Ionic Strength on Sensor Response
For researchers and drug development professionals, the pursuit of accurate, continuous molecular monitoring in vivo represents a significant frontier in biomedical science. A critical, yet often underexplored, challenge in this domain is the susceptibility of biosensors to fluctuations in their immediate physiological environment. Parameters such as temperature, pH, and ionic strength—while tightly regulated in the mammalian body—can vary sufficiently across different tissue types and physiological states to compromise sensor accuracy. This guide provides a comparative analysis of how these environmental factors impact various biosensor platforms, evaluates the performance of different calibration strategies to mitigate these effects, and presents supporting experimental data to inform robust sensor selection and deployment in research.
Comparative Impact of Environmental Factors on Sensor Platforms
The stability and accuracy of biosensors are not uniform; their performance under stress is a function of their underlying design, materials, and transduction mechanisms. The following comparison outlines the tolerance of different sensor types to environmental variations.
Table 1: Comparative Stability of Capped Gold Nanoparticles (AuNPs) under Environmental Stress [19]
| Capping Agent | Temperature Tolerance | pH Tolerance | Ionic Strength Tolerance (Saline) |
|---|---|---|---|
| Glutathione (AuNPs-II) | Stable up to 70°C for 144 h | Wide range (pH 3–11) | High (up to 1600 mM) |
| Citrate (AuNPs-I) | Less stable than AuNPs-II | Less stable than AuNPs-II | Less stable than AuNPs-II |
| Ascorbic Acid (AuNPs-III) | Susceptible to slight variation | Narrow range | Low (only up to 80 mM) |
Table 2: Impact of Physiological-Scale Variations on Electrochemical Aptamer-Based (EAB) Sensors [20]
| Environmental Parameter | Physiological Range Tested | Impact on EAB Sensor Accuracy | Corrective Action |
|---|---|---|---|
| Ionic Strength & Cations | 152 mM to 167 mM (Na+, K+, Mg2+, Ca+) | Minimal; Mean Relative Error (MRE) clinically acceptable (<20%) | No correction typically needed |
| pH | 7.35 to 7.45 | Minimal; MRE clinically acceptable (<20%) | No correction typically needed |
| Temperature | 33°C to 41°C | Significant error induced | Requires measurement and correction |
Key Insights from Comparative Data
- Nanoparticle Stability: Glutathione-capped AuNPs demonstrate exceptional colloidal stability under extreme conditions, making them superior for applications requiring high ionic strength, variable pH, or elevated temperatures [19]. In contrast, Ascorbic Acid-capped AuNPs are highly susceptible to even mild environmental changes.
- In Vivo Sensor Robustness: EAB sensors, a leading platform for continuous in vivo monitoring, show remarkable resilience to physiologically relevant variations in ionic composition and pH. This is largely because these parameters are under tight homeostatic control in blood and interstitial fluid [20].
- The Primary Challenge - Temperature: Across platforms, temperature fluctuation is the most significant environmental confounder. For EAB sensors, physiologically plausible changes (e.g., from 33°C skin temperature to 41°C core fever) induce substantial measurement errors that must be corrected for accurate readings [20].
Experimental Protocols for Assessing Environmental Impact
To systematically evaluate sensor performance, standardized experimental protocols are essential. The methodologies below are derived from cited studies and can serve as templates for validation.
- Objective: To determine the tolerance levels of differentially capped AuNPs to temperature, pH, and ionic strength.
- Synthesis: AuNPs are synthesized via chemical reduction methods. Citrate-capped AuNPs (AuNPs-I) are prepared by the trisodium citrate reduction method. Glutathione-capped (AuNPs-II) and Ascorbic Acid-capped (AuNPs-III) are synthesized by ligand exchange and direct reduction, respectively.
- Characterization: Synthesized AuNPs are characterized using UV-Vis spectroscopy (to monitor the Localized Surface Plasmon Resonance (LSPR) peak), Dynamic Light Scattering (DLS) for size and zeta potential, and Transmission Electron Microscopy (TEM) for morphology.
- Stress Testing:
- Temperature: AuNP colloidal solutions are incubated at temperatures ranging from 4°C to 70°C for up to 144 hours. Aliquots are taken at intervals for LSPR measurement and visual inspection for aggregation.
- pH: The pH of AuNP solutions is adjusted from pH 2 to 12 using dilute HCl or NaOH. Changes in LSPR and solution color are monitored after a set equilibration time.
- Ionic Strength: Increasing concentrations of NaCl (from 0 mM to 1600 mM) are added to AuNP solutions. The stability is assessed by tracking the LSPR peak and observing color changes indicative of aggregation.
- Data Analysis: The specific conditions under which the LSPR peak broadens, shifts, or disappears—or the solution color changes—are identified as the tolerance limits.
- Objective: To quantify the accuracy of EAB sensors against target analytes under physiological variations in cation concentration, pH, and temperature.
- Sensor Calibration:
- Calibrate sensors in a standard buffer (e.g., 20 mM HEPES, pH 7.4) containing midpoint concentrations of physiological cations (Na+, K+, Mg2+, Ca2+) at 37°C.
- Perform titrations of the target analyte (e.g., vancomycin, phenylalanine) and fit the data to a Langmuir isotherm model to generate a standard calibration curve.
- Validation Testing:
- Challenge new sensors with a test set of analyte concentrations under "out-of-calibration" conditions.
- Cation/Ionic Strength: Use buffers where all four cations are simultaneously at the lower or upper end of their physiological range.
- pH: Use buffers at pH 7.35 and 7.45.
- Temperature: Perform measurements across a range from 33°C to 41°C.
- Use the standard-condition calibration curve to estimate the analyte concentration in these non-standard conditions.
- Challenge new sensors with a test set of analyte concentrations under "out-of-calibration" conditions.
- Data Analysis: Calculate the Mean Relative Error (MRE) for each condition. Compare the MRE under test conditions to the MRE achieved under standard calibration conditions to assess the degradation in accuracy.
Diagram 1: Environmental impact pathways and calibration corrections for biosensors.
Calibration Methods for Accuracy Optimization
When environmental factors degrade sensor performance, calibration strategies are essential to restore accuracy. The following methods are currently employed in research settings.
Table 3: Comparison of Calibration Methods for In-Vivo Biosensing
| Calibration Method | Principle | Experimental Workflow | Impact on Accuracy | Key Considerations |
|---|---|---|---|---|
| Point-of-Care (POC) Blood Glucose Calibration [21] | Uses intermittent fingerstick blood glucose measurements to recalibrate a continuous glucose monitor (CGM). | 1. POC BG measurement is taken.\n2. Value is entered into the CGM device if the sensor reading is outside a validation threshold (e.g., ±20%).\n3. Sensor recalibrates its output. | MARD reduced from 25% at calibration event to ~9.6% after 6 hours. | Most effective when calibration is timely (within 5-10 minutes of POC test). |
| Temperature-Aware Correction Algorithms [20] | Measures ambient temperature and applies a mathematical correction to the sensor signal based on pre-characterized temperature sensitivity. | 1. Characterize sensor's dose-response curve at multiple temperatures.\n2. Develop a model (e.g., using ANN) that maps signal and temperature to analyte concentration.\n3. In deployment, co-measure temperature and apply the model in real-time. | Corrects substantial errors induced by physiological temperature variations (33-41°C). | Requires integrated temperature sensor and robust model trained on high-quality data. |
| AI-Enhanced Signal Processing [22] [23] | Uses machine learning (e.g., Artificial Neural Networks) to process complex signal data (e.g., fluorescence lifetime) and decouple analyte concentration from environmental noise. | 1. Train a model (e.g., ANN, Spiking GNN) on a large dataset of sensor outputs under varied analyte and environmental conditions.\n2. Deploy the trained model to interpret raw sensor signals in real-time. | Improves precision, enables faster readouts, and enhances robustness against interference. | Dependent on the quality and breadth of the training dataset; can be computationally intensive. |
Diagram 2: Workflow for selecting calibration correction methods.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Materials and Reagents for Sensor Stability and Calibration Research
| Reagent/Material | Function in Research | Example Application |
|---|---|---|
| Glutathione (GSH) | Capping agent for gold nanoparticles to confer high colloidal stability against aggregation under extreme ionic, pH, and temperature stress [19]. | Creating stable nanoparticle platforms for sensing in complex biological environments like waste water or physiological fluids. |
| Electrochemical Aptamer-Based (EAB) Sensor | A biosensor platform where a target-binding, redox-tagged aptamer is immobilized on a gold electrode, enabling real-time, reversible molecular monitoring in vivo [20]. | Continuous measurement of drugs (e.g., vancomycin) or metabolites (e.g., phenylalanine) in live animal models. |
| Chromatic Nanoswitchers (CNSs) | Fluorescent nanothermometers comprising a dye in a thermoresponsive matrix, providing high-sensitivity lifetime-based temperature reading resistant to environmental interference [23]. | Accurate, remote thermal sensing at the nanoscale (e.g., for cellular thermodynamics or microelectronic devices). |
| Artificial Neural Networks (ANNs) | Machine learning models for advanced processing of complex sensor signals (e.g., from FET sensors or fluorescent nanoswitchers) to improve accuracy and speed of readouts [22] [23]. | Predicting sensor sensitivity categories from material properties; enabling fast, robust thermal readouts from fluorescence lifetime data. |
| Phase Change Material (PCM) Matrix | A material (e.g., eicosane/docosane mixture) that undergoes a solid-to-liquid phase transition at a specific temperature, used to modulate a fluorescent dye's emission properties [23]. | Serving as the core of CNSs to create a highly temperature-sensitive fluorescent reporter around physiological temperatures (~37°C). |
Distinguishing Between In-Vivo and Ex-Vivo Calibration Requirements
In the field of biosensing, the accuracy and reliability of measurements are paramount, particularly when these sensors are deployed in complex biological environments. The calibration requirements for biosensors diverge significantly depending on whether they are intended for use within a living organism (in vivo) or outside of it in controlled laboratory settings (ex vivo). This guide objectively compares the performance and calibration methodologies for these two distinct application domains, framing the discussion within a broader thesis on accuracy comparison for calibration methods in biosensing research. The calibration approaches are shaped by fundamentally different challenges: in vivo calibration must contend with a dynamic, closed-loop biological system, whereas ex vivo calibration operates in controlled, accessible environments. Understanding these distinctions is critical for researchers, scientists, and drug development professionals who rely on precise measurements for diagnostic, therapeutic, and research applications.
Comparative Analysis of Calibration Environments
The table below summarizes the core distinctions between in vivo and ex vivo biosensor calibration, highlighting how the deployment environment dictates calibration strategy, challenges, and technological solutions.
Table 1: Fundamental Requirements for In-Vivo vs. Ex-Vivo Biosensor Calibration
| Aspect | In-Vivo Calibration | Ex-Vivo Calibration |
|---|---|---|
| Primary Objective | Continuous, real-time monitoring in a dynamic, closed system [5] [18] | Precise, endpoint or intermittent measurement in a controlled, open system [9] [24] |
| System Accessibility | Limited or no physical access post-implantation; often a closed-loop system [18] | Full physical and operational access; an open system allowing for direct manipulation [9] |
| Key Challenges | Biofouling, signal drift, dynamic physiological changes, biocompatibility, and limited recalibration opportunities [18] [25] | Controlling experimental parameters (e.g., pH, temperature), correcting for instrumentation drift, and sample handling [9] [26] |
| Calibration Strategy | Emphasis on calibration-free operation, internal reference standards, and reversible sensing elements [5] [18] | Reliance on external calibration curves using standard solutions and control samples [9] [24] |
| Common Techniques | Self-referencing sensors, multi-parameter correction, in-situ background measurement [5] [27] | Pre- and post-measurement calibration with known analyte concentrations, signal normalization [9] |
| Data Reliability | Vulnerable to long-term signal drift and biofouling; requires robust sensor design [25] | Generally high and can be verified repeatedly; susceptible to acute instrumental error [9] |
Experimental Protocols and Performance Data
In-Vivo Calibration: Towards Calibration-Free Operation
The gold standard for in vivo sensing is a calibration-free or self-calibrating sensor that maintains accuracy over long durations within the body. A prominent example is the use of electrochemical DNA (eDNA) biosensors for continuous therapeutic drug monitoring (TDM).
Table 2: Performance of Selected In-Vivo Biosensing Platforms
| Biosensor Platform | Target Analyte | Key Calibration Feature | Reported Performance / Challenge |
|---|---|---|---|
| Electrochemical DNA (eDNA) Sensors [5] | Drugs, Neurochemicals | Calibration-free strategies; reversible binding for continuous equilibrium | Advances personalized drug therapy; challenges in long-term stability & selectivity [5] |
| Genetically Encoded FRET Biosensor (R-eLACCO2.1) [27] | Extracellular L-lactate | Use of internal FRET standards ("FRET-ON/OFF") for signal normalization | Enables multiplexed imaging with neural activity sensors (e.g., GCaMP) in awake mice [27] |
| Microneedle (MN) Biosensors [25] | Glucose, Lactate, Hormones | Pre-use calibration; challenge with signal drift due to biofouling & electrode degradation | Long-term stability (>24h) is challenging; strategies include antifouling coatings [25] |
Detailed Experimental Protocol: FRET Biosensor Calibration for In-Vivo Imaging [9] [27]
- Sensor Design and Expression: Utilize a genetically encoded biosensor (e.g., R-eLACCO2.1 for lactate) expressed in the target tissue of a live animal model (e.g., mouse somatosensory cortex).
- Introduction of Calibration Standards: Co-express or co-introduce engineered "FRET-ON" and "FRET-OFF" standard proteins in a subset of cells. These standards provide reference signals for high and low FRET efficiency, independent of the actual analyte concentration.
- In-Vivo Image Acquisition: Perform multiplexed fluorescence imaging (e.g., using two-photon microscopy) on awake, behaving subjects. Simultaneously capture signals from the biosensor and the calibration standards.
- Signal Normalization: Normalize the acquired acceptor-to-donor FRET ratio from the biosensor against the signals from the FRET-ON and FRET-OFF standards within the same imaging session. This corrects for fluctuations in laser intensity, optical path, and tissue scattering.
- Data Validation: The calibration process should restore the expected reciprocal changes in donor and acceptor signals, validating the observed biosensor responses against instrumentation artifacts.
In-Vivo FRET Biosensor Calibration Workflow
Ex-Vivo Calibration: Precision Through Controlled Referencing
Ex vivo calibration relies on constructing a reliable relationship between sensor signal and analyte concentration in a controlled medium, which is then applied to interpret measurements in biological samples like serum, urine, or tissue extracts.
Detailed Experimental Protocol: Aptamer-Based Fluorescent Detection of ATP in Body Fluids [24]
- Probe Fabrication: Construct a fluorescent nanoprobe by adsorbing a ROX-tagged ATP-aptamer onto the surface of titanium carbide (TC) nanosheets. The TC acts as a quencher, initializing the probe in an "off" state.
- Construction of Calibration Curve:
- Prepare a series of standard ATP solutions in a buffer, spanning the expected physiological range (e.g., 0 μM to 1.5 mM).
- Incubate a fixed concentration of the TC/Apt probe with each standard solution.
- Measure the fluorescence recovery at 610 nm upon excitation at 545 nm. The fluorescence intensity increases as ATP binds the aptamer, releasing it from the quencher.
- Plot fluorescence intensity versus ATP concentration to generate a standard calibration curve.
- Sample Measurement and Quantification:
- Dilute the ex vivo sample (e.g., mouse serum, human serum, or urine) appropriately.
- Incubate the sample with the same concentration of TC/Apt probe under identical conditions.
- Measure the fluorescence signal and use the pre-established calibration curve to determine the ATP concentration in the unknown sample.
Table 3: Performance of an Ex-Vivo ATP Biosensor in Body Fluids [24]
| Body Fluid Sample | Linear Detection Range | Limit of Detection (LOD) | Key Application |
|---|---|---|---|
| Mouse Serum | 1 μM to 1.5 mM | 0.2 μM | Monitoring metabolic status and disease biomarkers [24] |
| Human Serum | 1 μM to 1.5 mM | 0.2 μM | Diagnostic detection of diseases linked to abnormal ATP [24] |
| Mouse Urine | 1 μM to 1.5 mM | 0.2 μM | Non-invasive metabolic monitoring [24] |
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents and materials critical for implementing the calibration methods discussed in this guide.
Table 4: Essential Research Reagents for Biosensor Calibration
| Reagent / Material | Function | Example Use Case |
|---|---|---|
| FRET Standard Plasmids (FRET-ON, FRET-OFF) [9] | Provide internal reference signals for normalizing imaging conditions and calculating FRET efficiency in vivo. | Calibrating genetically encoded biosensors (e.g., R-eLACCO2.1) in live cell or animal imaging [9]. |
| Titanium Carbide (TC) Nanosheets [24] | Act as a highly efficient fluorescence quencher in a FRET-based assay configuration. | Core component of the ex vivo ATP detection probe; quenches ROX-aptamer fluorescence [24]. |
| ROX-tagged ATP Aptamer [24] | The biological recognition element that binds ATP specifically, coupled to a fluorescent reporter. | Sensing element in the ex vivo ATP probe; fluorescence recovers upon target binding [24]. |
| Analyte Standard Solutions | Used to create the primary calibration curve, defining the relationship between signal and concentration. | Preparing known concentrations of ATP, glucose, or lactate for ex vivo sensor calibration [25] [24]. |
| Antifouling Coatings (e.g., Zwitterionic polymers) [25] | Coating material applied to sensor surfaces to minimize non-specific protein adsorption and biofouling. | Extending the functional lifetime and stability of implantable microneedle sensors in vivo [25]. |
The calibration requirements for in vivo and ex vivo biosensing are fundamentally distinct, each presenting a unique set of challenges and necessitating specialized technological solutions. Ex vivo calibration achieves high accuracy through controlled external referencing and calibration curves, offering precision for diagnostic and research applications. In contrast, in vivo calibration is evolving toward calibration-free and self-referencing paradigms to overcome the constraints of dynamic, inaccessible biological systems. The choice of calibration strategy directly impacts the validity and reliability of the resulting data. As the field advances, the integration of robust internal standards, antifouling materials, and artificial intelligence for data correction will be crucial to bridging the gap between the precision of ex vivo methods and the imperative for reliable, long-term in vivo monitoring.
Comparative Analysis of Calibration Techniques and Algorithms
Calibration is a fundamental process in scientific measurement, serving as the critical bridge between a sensor's raw signal and a meaningful, quantitative result. In the context of in-vivo biosensing research, where accurate measurement of biological analytes is essential for both research conclusions and drug development, the choice of calibration methodology directly impacts data reliability. The two primary approaches—one-point and two-point calibration—differ significantly in their underlying principles, implementation complexity, and ultimately, their measurement accuracy.
A one-point calibration assumes a proportional relationship between the sensor's signal and the analyte concentration, effectively presuming that the calibration line passes through the origin (zero signal corresponds to zero concentration). This method calculates the sensor's sensitivity (S) from a single reference measurement: S = I/G, where I is the sensor current and G is the reference glucose concentration. The concentration at any time is then estimated as G(t) = I(t)/S [28]. In contrast, a two-point calibration incorporates an additional parameter to account for the sensor's background current (Io), which represents a glucose-nonspecific signal caused by interfering substances in the interstitial fluid such as ascorbic acid, acetaminophen, and uric acid. This method determines both sensitivity and background current using two reference measurements: S = (I₂ - I₁)/(G₂ - G₁) and Io = I₁ - (S × G₁). The subsequent concentration estimation is given by G(t) = (I(t) - Io)/S [29] [30].
The ongoing debate surrounding these methods centers on a fundamental trade-off: whether the theoretical advantage of accounting for background current in the two-point approach outweighs the potential error amplification from measurement uncertainties in practical applications. This article objectively compares these calibration strategies specifically for in-vivo biosensing, examining their relative accuracy through published experimental data, detailing their implementation protocols, and providing practical guidance for researchers in the field.
Theoretical Foundations and Practical Trade-offs
Core Conceptual Differences
The mathematical distinction between these calibration methods has profound practical implications. The one-point calibration model operates on a single-parameter system (sensitivity only), while the two-point calibration establishes a two-parameter system (sensitivity and background current). This additional parameter in the two-point method aims to enhance accuracy by accounting for the sensor's baseline signal, but it also introduces a potential vector for error propagation [30]. Measurement uncertainties, inherent in both reference glucose measurements and sensor signal acquisition, can significantly impact the calculated values of both S and Io. These uncertainties often manifest as a negative correlation between the estimated sensitivity and background current, sometimes resulting in physiologically implausible negative values for Io [30].
A significant challenge in two-point calibration arises from the physiological time lag between blood glucose (BG) and interstitial glucose (IG) concentrations. Since continuous glucose monitoring (CGM) sensors measure glucose in the interstitial fluid, not directly in blood, a variable gradient exists between BG and IG, particularly during non-steady-state conditions like dropping hypoglycemia or post-meal spikes. This lag causes a fundamental mismatch when calibrating ISIG values (which reflect IG) against BG values, leading to substantial error in estimating the sensor background current, especially when calibration points are taken during these dynamic periods [29].
Table 1: Core Characteristics of One-Point and Two-Point Calibration
| Feature | One-Point Calibration | Two-Point Calibration |
|---|---|---|
| Underlying Principle | Assumes negligible background current (Io); linear relationship through origin [28]. | Accounts for non-zero background current (Io); defines both slope and intercept [29]. |
| Mathematical Complexity | Simple: G(t) = I(t)/S [28]. | More complex: G(t) = (I(t) - Io)/S [29]. |
| Key Assumption | Background current (Io) is negligible or constant [28]. | Background current can be accurately estimated from two points [29]. |
| Primary Advantage | Simplicity, reduced error propagation from fewer measurements, user-friendly [28]. | Theoretically more comprehensive by accounting for baseline signal [29]. |
| Primary Limitation | Inaccurate if background current is significant and unaccounted for [29]. | Highly sensitive to measurement errors in reference values and physiological time lag [29] [30]. |
| User Workload | Lower (requires one reference measurement per calibration) [28]. | Higher (requires two reference measurements per calibration) [29]. |
Experimental Data and Performance Comparison
Clinical Evidence from Glucose Monitoring Studies
Substantial clinical evidence, particularly from continuous glucose monitoring (CGM) research, demonstrates a counterintuitive finding: despite its simpler model, one-point calibration often delivers superior accuracy in practice. A comprehensive study involving 132 type 1 diabetes patients directly compared a real-time CGM algorithm using two-point calibration against its updated version using one-point calibration. The results were revealing: the one-point calibration approach improved overall CGM accuracy, with the most significant enhancement observed in the critical hypoglycemic range. The Median Absolute Relative Difference (MARD) in hypoglycemia was 12.1% for one-point calibration compared to 18.4% for the two-point method [29].
Furthermore, the one-point calibration increased the percentage of sensor readings in the clinically accurate Zones A+B of the Clarke Error Grid Analysis across the entire glycemic range and enhanced hypoglycemia sensitivity, a crucial safety parameter for diabetic patients [29]. A separate, earlier study that implanted glucose sensors in nine diabetic patients for 3-7 days found congruent results. It reported that the percentages of points in zones A and B of the Clarke Error Grid were significantly higher when the system was calibrated using the one-point method compared to the two-point method [28].
Quantitative Performance Metrics
Table 2: Summary of Key Performance Metrics from Clinical Studies
| Performance Metric | One-Point Calibration Performance | Two-Point Calibration Performance | Study Context |
|---|---|---|---|
| MARD in Hypoglycemia | 12.1% [29] | 18.4% [29] | 132 type 1 diabetes patients [29]. |
| Points in Clarke Error Grid A+B | Significantly higher percentage [28] | Lower percentage [28] | 9 diabetic patients, 3-7 day implantation [28]. |
| Hypoglycemia Sensitivity | Enhanced [29] | Reduced [29] | 132 type 1 diabetes patients [29]. |
| Impact of Reference Measurement Error | Less sensitive [28] | Highly sensitive; causes miscalculation of S and Io [30] | Theoretical analysis and patient trials [30] [28]. |
The superior performance of the one-point method is largely attributed to its robustness against measurement uncertainties. Every reference blood glucose measurement carries a potential error (e.g., ±10% for commercial meters), and every sensor signal is subject to electronic noise. The two-point calibration process magnifies these errors. As noted in research, "a measurement error on the current, linked for instance to electric noise, and/or on capillary blood glucose measurement... contributed to the generation of a value of Io which could be either positive or negative" [30]. The one-point method, by avoiding the calculation of this additional parameter, sidesteps this source of error amplification.
Detailed Experimental Protocols
Protocol for a One-Point Calibration Study
The following protocol is adapted from methodologies used in clinical CGM research [29] [28]:
- Sensor Deployment: Implant the biosensor (e.g., a subcutaneous enzymatic glucose sensor) into the target tissue (e.g., abdominal subcutaneous tissue) of the study subject (e.g., human or animal model).
- Reference Measurement Collection: At predetermined time points (e.g., before meals), obtain a reference measurement of the analyte (e.g., capillary blood glucose) using a validated reference method (e.g., clinical glucose meter). Ensure the measurement is performed in duplicate for confirmation.
- Signal Recording: Simultaneously record the raw signal output (e.g., current in nA) from the biosensor.
- Calculation of Sensitivity (S): For each calibration instance, calculate the sensor's sensitivity as the ratio of the sensor signal (I) to the reference concentration (G): S = I / G.
- Conversion to Estimated Concentration: To convert subsequent sensor signals I(t) into estimated analyte concentrations G(t), apply the formula: G(t) = I(t) / S.
- Recalibration Schedule: Recalibrate the sensor periodically (e.g., once or twice daily) to account for potential changes in sensor sensitivity over time.
Protocol for a Two-Point Calibration Study
This protocol outlines the steps for a two-point calibration, incorporating elements from both biosensing and other scientific fields [29] [31]:
- Sensor Deployment: Implant the biosensor as described in Section 4.1.
- Two-Point Reference Collection: Obtain two separate reference measurements (G₁, G₂) and their concomitant sensor signals (I₁, I₂). These measurements should be taken at different concentration levels and distant by a sufficient time interval (e.g., at least 1 hour) to ensure a meaningful difference.
- Parameter Calculation:
- Calculate the sensor sensitivity: S = (I₂ - I₁) / (G₂ - G₁).
- Calculate the background current: Io = I₁ - (S × G₁).
- Conversion to Estimated Concentration: For all subsequent sensor signals I(t), calculate the analyte concentration using: G(t) = (I(t) - Io) / S.
- Error Handling: Implement procedures to handle potential calculation errors, such as negative Io values, which can arise from measurement uncertainties [30].
Protocol for a Comparative Accuracy Study
To objectively compare both methods, a within-subject design is optimal [29]:
- Study Population: Recruit a sufficient number of subjects (e.g., 100+ type 1 diabetic patients) to ensure statistical power.
- Data Collection: Collect a large dataset of paired sensor signals and high-quality reference measurements over several days.
- Post-Hoc Analysis: Apply both one-point and two-point calibration algorithms to the same sensor data stream offline.
- For one-point calibration, use reference points from, for instance, pre-meal times.
- For two-point calibration, use pairs of reference points, such as those before breakfast.
- Accuracy Assessment: Compare the output of both calibrated signals against the reference measurements using standardized metrics:
- Median Absolute Relative Difference (MARD): Calculated for the overall range and specific glycemic ranges (hypoglycemia, euglycemia, hyperglycemia).
- Clarke Error Grid Analysis (EGA): To assess clinical accuracy.
- Hypoglycemia Sensitivity and Specificity.
Diagram 1: Workflow for a Comparative Calibration Accuracy Study. This diagram illustrates the parallel application of one-point and two-point calibration algorithms on the same dataset for a direct performance comparison.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for In-Vivo Calibration Research
| Item Name | Function/Description | Relevance to Calibration Research |
|---|---|---|
| Subcutaneous Glucose Sensor (e.g., SCGM1, Roche) [29] | Microdialysis-based or enzymatic sensor for continuous glucose measurement in interstitial fluid. | The primary data source. Its raw signal (ISIG) is the input for all calibration procedures. |
| High-Accuracy Blood Glucose Meter (e.g., Glucotrend) [30] [28] | Provides reference capillary blood glucose measurements for calibration and validation. | Serves as the "ground truth." Its measurement error is a key source of uncertainty in calibration [30]. |
| MCT Inhibitors (e.g., AR-C155858, AZD3965) [31] | Pharmacological blockers of monocarboxylate transporters. | Used in advanced two-point calibration protocols (e.g., for FRET sensors) to manipulate intracellular metabolite levels and determine the sensor's dynamic range (RMAX). |
| MPC Inhibitor (e.g., UK-5099) [31] | Pharmacological blocker of the mitochondrial pyruvate carrier. | Used in conjunction with MCT inhibitors to induce intracellular pyruvate saturation for sensor calibration. |
| FRET-based Genetically Encoded Indicator (e.g., Pyronic) [31] | A fusion protein that changes fluorescence upon binding a specific metabolite (e.g., pyruvate). | A modern biosensing tool whose fluorescence signal requires calibration for quantitative assessment, often via a two-point method to determine its full dynamic range in each cell. |
The body of evidence from in-vivo biosensing research challenges the intuitive appeal of the more complex two-point calibration. For researchers and drug development professionals, the choice between one-point and two-point calibration is not merely theoretical but has direct consequences for data integrity.
The consensus from multiple studies indicates that one-point calibration often provides superior accuracy, particularly in dynamic physiological states like hypoglycemia. This is primarily because it is less vulnerable to the error amplification inherent in calculating a background current (Io) from noisy real-world measurements. The two-point method, while theoretically more comprehensive, is highly sensitive to physiological time lags and reference measurement errors, often leading to greater overall deviation [29] [30] [28].
Recommendations for Practice
Based on the analyzed evidence, the following recommendations are proposed:
- Prioritize One-Point Calibration for Routine CGM: For most in-vivo glucose monitoring applications, a one-point calibration protocol, performed once or twice daily before meals, is recommended as the starting point for its robustness and simplicity [28].
- Reserve Two-Point Calibration for Specific Cases: Two-point calibration remains valuable in scenarios where the background current is known to be significant and stable, or in specialized research requiring absolute quantification of novel biomarkers using advanced sensors like FRET-based indicators, where its protocol is well-established [31].
- Acknowledge and Minimize Reference Error: Regardless of the method chosen, researchers must recognize that the accuracy of the reference measurement is a fundamental limiter of calibration quality. Using highly precise reference methods and duplicate measurements is crucial [30].
- Contextualize the "Best" Method: The optimal calibration strategy is use-specific. Researchers should conduct pilot studies to compare both methods on their specific sensor platform and target analyte to make a data-driven decision.
In conclusion, within the critical field of in-vivo biosensing, the simpler one-point calibration method frequently offers a more favorable trade-off, yielding not just greater usability but also higher measurement accuracy than its two-point counterpart.
Dual-Frequency and Ratiometric Approaches for Calibration-Free Operation
The need for frequent calibration remains a significant hurdle limiting the widespread clinical adoption of continuous biosensors. Conventional biosensors require calibration against reference samples to correct for sensor-to-sensor fabrication variations and signal drift experienced in complex biological environments. This process is cumbersome, increases the risk of user error, and is particularly problematic for measuring endogenous biomarkers where "zero-concentration" reference points are unavailable [32] [33]. In response to these challenges, dual-frequency and ratiometric approaches have emerged as transformative strategies that enable calibration-free operation while maintaining high accuracy in vivo.
These innovative methods leverage inherent signal properties rather than external references to generate measurement outputs that are largely independent of the absolute number of sensing elements or the microscopic surface area of electrodes. By producing a unitless ratiometric signal, these approaches effectively cancel out common noise sources and fabrication variances that plague traditional single-output sensors [32] [33]. This capability is particularly valuable for applications such as therapeutic drug monitoring and tracking of disease biomarkers in live animals and humans, where conventional calibration is impractical or impossible after sensor deployment [5].
This guide provides a systematic comparison of these calibration-free methodologies, focusing on their operational principles, experimental implementation, and performance characteristics. By presenting quantitative data and detailed protocols, we aim to equip researchers and drug development professionals with the necessary information to select and implement appropriate calibration-free strategies for their specific in vivo biosensing applications.
Comparative Performance Analysis of Calibration-Free Methods
The table below summarizes the key performance characteristics of major calibration-free biosensing approaches, highlighting their relative advantages in real-world applications.
Table 1: Performance Comparison of Calibration-Free Biosensing Methods
| Method | Target Analytes | Dynamic Range | Reported Accuracy | Key Advantages | Implementation Complexity |
|---|---|---|---|---|---|
| Dual-Frequency EAB | Vancomycin, Phenylalanine, Cocaine | Up to 100-fold | Within ±20% across dynamic range | Drift correction in vivo, eliminates single-point calibration | Medium (requires frequency optimization) |
| Ratiometric EAB | Vancomycin, Phenylalanine | Not specified | Effectively indistinguishable from KDM | Simple signal calculation, robust performance | Low (simple current ratio calculation) |
| Dual-Comb Biosensing | SARS-CoV-2 nucleocapsid protein | Detection to sub-fM level | High precision via RF conversion | Exceptional sensitivity, active temperature compensation | High (specialized optical setup required) |
| Ratiometric Fluorescence | Various small molecules, ions | Varies by probe design | Improved reliability via self-calibration | Built-in reference signal, visual detection capability | Medium (requires dual-emission probes) |
Table 2: In Vivo Performance of Electrochemical Aptamer-Based Sensors
| Sensor Type | Analysis Method | Test Environment | Baseline Recovery | Drift Correction | Calibration Requirement |
|---|---|---|---|---|---|
| Traditional EAB | Single-frequency SWV | Live rats | Poor without calibration | Limited | Single-point calibration essential |
| Dual-Frequency EAB | rKDM (Equation 2) | Live rats | Accurate | Excellent | None |
| Dual-Frequency EAB | Ratiometric (Equation 3) | Live rats | Accurate | Excellent | None |
Experimental Protocols for Key Calibration-Free Methods
Dual-Frequency Electrochemical Aptamer-Based (EAB) Sensing
Principle of Operation: This method exploits the square-wave frequency dependence of electron transfer kinetics in electrochemical aptamer-based sensors. When target molecules bind to electrode-bound aptamers, they alter electron transfer rates, producing measurable current changes. The approach uses two specific square-wave frequencies: one that is highly responsive to target binding and another that is minimally responsive [32] [33].
Protocol Details:
- Sensor Fabrication: Thiol-modified redox reporter-labeled aptamers are co-immobilized onto gold electrodes through self-assembled monolayer formation, typically using a 1:1000 ratio of aptamer to 6-mercapto-1-hexanol to achieve optimal packing density and sensor response [32].
- Frequency Selection: Prior to testing, identify optimal frequency pairs through preliminary experiments. For cocaine detection, 500 Hz (responsive) and 40 Hz (non-responsive) have been used effectively [33].
- Measurement: Interrogate sensors simultaneously or sequentially at both selected frequencies using square wave voltammetry.
- Data Analysis: Calculate the ratiometric output using either the rKDM or simple ratio method:
Validation: Researchers should conduct in vivo testing using known drug administration protocols (e.g., 30 mg/kg vancomycin bolus infusion in rat models) to compare sensor outputs with expected pharmacokinetic profiles [32].
Dual-Comb Biosensing Protocol
Principle of Operation: This optical method transforms antigen-concentration-dependent optical spectrum shifts into photonic radio-frequency shifts using optical frequency combs, enabling highly precise electrical frequency measurements. A dual-comb configuration with active and dummy sensing elements provides built-in temperature drift compensation [34].
Protocol Details:
- Setup Configuration: Establish two synchronized optical frequency combs with matched multimode-interference (MMI) fiber sensors in their cavities.
- Surface Modification: Functionalize the MMI fiber sensor in the active comb with specific antibodies (e.g., anti-SARS-CoV-2 nucleocapsid protein) while the dummy sensor remains unmodified or blocked with irrelevant antibodies.
- Measurement: Expose both sensors to the sample solution and monitor the repetition frequency (frep) shifts in both combs.
- Data Processing: Calculate the differential signal between active and dummy sensors to compensate for temperature-induced drift:
Δfrep = frep(active) - frep(dummy)[34].
Validation: Test with standard antigen solutions across expected concentration ranges (e.g., 0-1000 pg/mL for SARS-CoV-2 nucleocapsid protein) to establish calibration curves before analyzing unknown samples [34].
Signaling Pathways and Experimental Workflows
The following diagrams illustrate the core operational principles and experimental workflows for the primary calibration-free biosensing methods discussed in this guide.
Dual-Frequency EAB Sensing Workflow
Dual-Comb Biosensing Signal Pathway
Essential Research Reagent Solutions
The table below catalogues key reagents and materials required for implementing dual-frequency and ratiometric calibration-free biosensing approaches, based on the methodologies cited in this guide.
Table 3: Essential Research Reagents for Calibration-Free Biosensing
| Reagent/Material | Function | Example Application | Key Considerations |
|---|---|---|---|
| Thiol-modified Aptamers | Biorecognition element | EAB sensor fabrication | Target-specific selection; redox reporter incorporation required |
| 6-Mercapto-1-hexanol (C6-OH) | Self-assembled monolayer formation | EAB sensor surface passivation | Optimize aptamer:C6-OH ratio for binding efficiency |
| Methylene Blue | Redox reporter | Electron transfer modulation in EAB | Covalent attachment to aptamer essential |
| Anti-SARS-CoV-2 N protein Antibody | Biorecognition element | Dual-comb biosensing for COVID-19 | Surface immobilization required on MMI fiber |
| Gold Electrodes | Sensor substrate | EAB sensor platform | Microscopic surface area affects baseline current |
| MMI Fiber Sensors | Optical sensing element | Dual-comb biosensing | Requires surface functionalization |
| Polydopamine-based Coatings | Antifouling protection | In vivo sensor stability | Improves biocompatibility and reduces drift |
Dual-frequency and ratiometric approaches represent a paradigm shift in biosensor operation, effectively addressing the longstanding challenge of calibration in continuous molecular monitoring. The experimental data and performance comparisons presented in this guide demonstrate that these methods achieve accuracy within clinically acceptable margins (±20%) without requiring single-point calibration [32] [33].
For researchers and drug development professionals, the choice between these approaches depends on specific application requirements. Dual-frequency EAB sensors offer particular advantages for in vivo therapeutic drug monitoring due to their robust drift correction capabilities and relatively straightforward implementation [32]. Dual-comb biosensing provides exceptional sensitivity for detecting low-abundance biomarkers but requires more specialized optical instrumentation [34]. Ratiometric fluorescence methods present opportunities for visual detection and simplified readouts, especially in point-of-care settings [35].
As these calibration-free technologies continue to evolve, their integration with artificial intelligence for data processing and adaptive sensing promises to further enhance performance across healthcare, environmental monitoring, and personalized medicine applications [36]. The research reagents and experimental protocols outlined in this guide provide a foundation for implementing these cutting-edge approaches in various biosensing contexts.
In the pursuit of reliable quantitative measurements for in-vivo biosensing research, the choice of calibration model is paramount. These models are crucial for translating a raw sensor signal, such as a change in optical intensity or electrical current, into an accurate concentration reading of a target analyte within a living system. Kinetic calibration models primarily address the challenges of dynamic biological environments, where factors like sample matrix effects and sensor fouling can degrade performance over time. This guide objectively compares two dominant methodological approaches: Diffusion-Based Calibration and On-Fibre Standardization.
Diffusion-based models rely on mathematical frameworks to account for the mass transport and biochemical reaction kinetics of an analyte at the sensor interface. In contrast, on-fibre standardization incorporates a reference material or process directly onto the sensor probe, enabling self-calibration and correction of signal drift. This guide will compare the theoretical foundations, experimental performance, and practical applicability of these two strategies, providing researchers with the data necessary to select the optimal method for their specific in-vivo biosensing challenges.
Theoretical Foundations and Key Principles
Diffusion-Based Calibration Models
Diffusion-based models are grounded in the principles of reaction-diffusion kinetics, which describe how the rate of signal generation is governed by the diffusion of an analyte to the sensor's bioactive surface and the subsequent biochemical reaction.
- Fundamental Mechanism: These models mathematically describe the sequence of an analyte diffusing from the bulk solution to the sensor surface, followed by its specific binding or reaction with an immobilized bioreceptor (e.g., an enzyme, antibody, or aptamer). The resulting signal is a function of both the analyte's concentration gradient and the kinetics of the biorecognition event [37] [38].
- Michaelis-Menten Kinetics: For enzymatic biosensors, the reaction at the surface is often described by Michaelis-Menten kinetics. The simplified model connects the bulk substrate concentration to the local reaction rate and the resulting change in a measurable parameter (e.g., local pH) [39] [38]. The steady-state response can be modeled to extract key kinetic parameters like the apparent Michaelis-Menten constant ((KM)) and the maximum reaction rate ((V{max})), which are vital for calibrating the sensor's response to analyte concentration [39].
- Governing Equations: The physical process is typically modeled using a reaction-diffusion equation. For a spherical sensor geometry, this can be expressed in a non-dimensional form, accounting for factors like enzyme loading and substrate diffusion [38]:
\[ \frac{1}{x^n}\frac{d}{dx}\left(x^n\frac{dM(x)}{dx}\right) - 2h^2 \frac{M(x)}{\alpha + M(x)} = 0 \]Where (M(x)) is the dimensionless substrate concentration, (n) defines the geometry (e.g., (n=2) for spherical), (h) is a Thiele modulus representing the reaction-to-diffusion ratio, and (\alpha) is the dimensionless Michaelis constant [38].
On-Fibre Standardization Methods
On-fibre standardization focuses on integrating a reference mechanism directly onto the optical fibre sensor itself to correct for instrumental drift and environmental variability, rather than relying solely on a priori kinetic models.
- Fundamental Mechanism: This approach uses the intrinsic properties of the optical fibre or an added reference layer to provide a stable signal benchmark. The core idea is to measure the analyte-sensitive signal relative to a reference signal that is insensitive to the analyte but affected by the same environmental and instrumental noise [40] [41].
- Evanescent Field and Internal Referencing: Many optical fibre biosensors operate by measuring intensity changes in the light guided through the fibre, which can be caused by luminescence or absorption from an analyte interacting with the evanescent field at the fibre's surface [40]. On-fibre standardization can be achieved by using a specific coating that provides a stable reference luminescence, or by leveraging different optical phenomena (e.g., referencing the amplitude of a specific cladding mode in a tilted fibre Bragg grating) to distinguish the analyte response from false signals [41].
- Advantages for In-Vivo Sensing: The primary strength of this method is its ability to perform real-time correction for signal drift caused by factors such as light source instability, variable coupling efficiency, and changes in the biological environment (e.g., biofouling that nonspecifically attenuates light) [40] [42]. This makes it exceptionally suited for long-term, continuous monitoring in dynamic in-vivo settings.
Performance Comparison and Experimental Data
The following tables summarize the key performance characteristics and experimental findings for biosensors employing these two calibration strategies, based on recent research.
Table 1: Comparative Performance of Diffusion-Based Calibrated Biosensors
| Target Analyte | Sensor Platform | Calibration Model Core | Reported LoD | Dynamic Range | Key Advantage |
|---|---|---|---|---|---|
| Urea [39] | Potentiometric EISCAP | Michaelis-Menten Steady-State | N/A | 0.1 - 50 mM | Quantifies enzyme kinetics ((KM), (V{max})) in different matrices (PBS vs. Artificial Urine). |
| Oxygen/Substrate [38] | Spherical Enzyme Catalyst | Reaction-Diffusion (Michaelis-Menten) | N/A | N/A | Predicts substrate concentration profile within a spherical cell or biocatalyst. |
| Therapeutic Drugs [5] | Electrochemical DNA (eDNA) | Binding Kinetics & Diffusion | Sub-femtomolar | > 6 orders of magnitude | Enables real-time, continuous monitoring of molecules in vivo. |
Table 2: Comparative Performance of On-Fibre Standardized Biosensors
| Sensor Technology | Standardization Method | Primary Application | Key Performance Outcome | Benefit of Standardization |
|---|---|---|---|---|
| Tilted Fibre Bragg Grating (TFBG) [41] | Multiresonant spectral referencing | Biochemical sensing | Excellent Limit of Detection (LoD); Elimination of temperature cross-sensitivities. | Enables simultaneous multiparameter sensing and accurate measurement in complex environments. |
| Intensity-Based Optical Fibre Biosensors [40] | Signal normalization & reference coatings | Detection of biomolecules | High sensitivity; Resistance to EM interference. | Corrects for light source instabilities and coupling variations, simplifying instrumentation. |
| Plasmonic Optical Fibre Sensors [42] | Advanced fibre structures (D-shaped, tapered) | Biomonitoring, disease diagnostics | High sensitivity and miniaturization. | Facilitates remote sensing and real-time monitoring capabilities in compact designs. |
Experimental Protocols
Protocol for Characterizing a Diffusion-Based Urea Biosensor
This protocol is adapted from the development of a potentiometric urea biosensor using an Electrolyte–Insulator–Semiconductor Capacitor (EISCAP) [39].
- Sensor Fabrication and Functionalization: Fabricate an EISCAP structure (e.g., Al/p–Si/SiO₂/Ta₂O₅). The pH-sensitive Ta₂O₅ gate is functionalized by depositing a bilayer of polyallylamine hydrochloride (PAH) and the enzyme urease.
- Experimental Setup and Data Acquisition: Place the sensor in a measurement cell connected to a precision impedance analyzer. Sequentially expose the sensor to standard solutions of urea prepared in phosphate buffer (PBS) and a complex matrix like artificial urine (AU), covering a concentration range of 0.1 to 50 mM. For each concentration, record the capacitance-voltage (C-V) curve after the signal stabilizes. Measure the shift in the characteristic capacitance value, which correlates to the local pH change induced by the enzymatic hydrolysis of urea.
- Data Fitting and Parameter Extraction: Use a simplified kinetic model under the steady-state approximation. The model provides an implicit algebraic relation linking the bulk urea concentration to the local pH at the sensor surface. Employ a numerical solver and fitting routine (e.g., in MATLAB) to fit the experimental pH-versus-urea data. This fitting yields the apparent kinetic parameters: the Michaelis constant ((KM)) and the normalized maximum reaction rate ((k̄V)).
- Validation: Compare the fitted parameters between PBS and AU. A significant change in (k̄_V), as reported in the literature (a three-order reduction in AU), highlights the inhibitory effects of the complex matrix and validates the necessity of matrix-specific calibration [39].
Protocol for Implementing On-Fibre Standardization with TFBGs
This protocol outlines the use of Tilted Fibre Bragg Gratings (TFBGs) for biosensing with intrinsic referencing, leveraging their multimode resonance spectrum [41].
- Sensor Fabrication: Inscribe a TFBG in the core of a single-mode optical fibre using femtosecond laser irradiation or phase mask technology. The tilt angle (typically 4-15 degrees) is a key parameter determining the spectral properties.
- Biofunctionalization: Immobilize bioreceptors (e.g., antibodies, aptamers) specific to the target analyte onto the fibre's cladding surface. This often involves prior surface activation (e.g., silanization) to create a reactive layer for covalent bonding of the receptors.
- Interrogation and Data Acquisition: Connect the TFBG to an interrogator or optical vector analyzer. Acquire the transmission spectrum of the TFBG, which shows numerous narrow-band cladding mode resonances and a core mode resonance (Bragg wavelength). Expose the sensor to solutions with varying concentrations of the target analyte.
- Signal Processing and Standardization: As the analyte binds to the surface, it changes the local refractive index, causing amplitude changes in the cladding mode resonances. The core mode resonance (Bragg wavelength) is strongly sensitive to temperature and strain but insensitive to the surrounding refractive index. Therefore, the Bragg resonance can be used as an internal reference to subtract the effects of temperature fluctuations from the cladding mode signals. The calibrated signal is the normalized amplitude change of the selected cladding mode(s).
- Quantification: Build a calibration curve by plotting the normalized, referenced signal against the logarithm of the analyte concentration to determine the limit of detection and sensitivity.
Conceptual Workflow and Signaling Pathways
The following diagram illustrates the core signaling pathway and logical sequence of events in a kinetic calibration model based on an enzymatic reaction, leading to a measurable signal.
Diagram 1: Signal pathway for diffusion-kinetic calibration.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Biosensor Development and Calibration
| Item | Function / Application | Specific Examples / Notes |
|---|---|---|
| Urease Enzyme | Bioreceptor for urea biosensing; catalyzes hydrolysis of urea, producing a local pH change. | Used in diffusion-based potentiometric sensors (EISCAP) for kinetic parameter extraction [39]. |
| DNA/Aptamer Probes | Bioreceptors for electrochemical DNA (eDNA) sensors; provide high specificity for targets like drugs, neurotransmitters, and biomarkers. | Enable sub-femtomolar detection in vivo; known for reversibility and continuous monitoring capabilities [5]. |
| Functionalized Gold Nanoparticles (AuNPs) | Enhance signal transduction in electrochemical and optical biosensors; increase surface area for bioreceptor immobilization. | Used in composites with MoS₂ for ultrasensitive electrochemical immunosensors (e.g., for BRCA-1) [12]. |
| Tilted Fibre Bragg Grating (TFBG) | Optical fibre sensing platform; its spectral comb of resonances enables intrinsic referencing and multiplexing. | Ideal for eliminating cross-sensitivities (e.g., temperature) in biochemical sensing [41]. |
| Polymer Coatings (e.g., PAH) | Used for enzyme immobilization on sensor surfaces; forms a stable matrix that retains bioactivity. | Polyallylamine hydrochloride (PAH) is used in bilayer structures with urease on EISCAP sensors [39]. |
| Graphene & Derivatives | Sensor transducer material; offers high conductivity, large surface area, and biocompatibility for electrical and optical biosensors. | Used in field-effect transistors (FETs) and electrochemical sensors for sensitive label-free detection [43]. |
The choice between diffusion-based kinetic models and on-fibre standardization is not a matter of which is universally superior, but which is most appropriate for the specific research application. The experimental data and protocols presented herein provide a clear framework for this decision.
- Diffusion-Based Calibration is a powerful tool for fundamental studies of sensor behavior and for applications where understanding the underlying reaction kinetics and mass transport is critical. Its strength lies in its ability to provide a deep, mechanistic understanding of the sensor's function and to extract quantitative kinetic parameters, even in complex matrices. This makes it invaluable for ex-vivo characterization and for in-vivo applications where the biochemical environment is reasonably well-understood and stable.
- On-Fibre Standardization excels in practical, real-world in-vivo sensing scenarios where operational stability and reliability over time are the primary concerns. Its ability to internally correct for signal drift caused by environmental instabilities and biofouling in real-time is a decisive advantage for long-term, continuous monitoring, as required in therapeutic drug monitoring or intensive physiological studies.
In summary, diffusion-based models provide the theoretical foundation for understanding sensor response, while on-fibre standardization offers a robust engineering solution to maintain accuracy in dynamic environments. The future of in-vivo biosensing likely lies in the synergistic combination of both approaches: using sophisticated kinetic models to design better sensors and intelligent on-probe standardization to ensure they perform reliably in the complex theater of a living system.
Advanced Algorithms for Continuous Glucose Monitoring Systems
Continuous Glucose Monitoring (CGM) systems have revolutionized diabetes management by providing real-time, dynamic insights into glucose levels, thereby enabling more precise therapeutic decisions [44] [45]. The core intelligence of these systems resides in their advanced algorithms, which transform raw sensor signals into accurate and clinically actionable glucose readings. The performance of these algorithms, particularly their calibration methods—whether factory-based or user-dependent—directly impacts measurement accuracy and reliability [46] [47]. This guide objectively compares the performance of current CGM systems, focusing on the critical role of their algorithms within the broader context of accuracy comparison for in-vivo biosensing research. We present supporting experimental data, detailed methodologies, and key reagents to serve researchers, scientists, and drug development professionals.
Performance Comparison of Leading CGM Systems
A recent 2025 prospective study provides a robust head-to-head comparison of three major factory-calibrated CGM systems: FreeStyle Libre 3 (FL3), Dexcom G7 (DG7), and Medtronic Simplera (MSP) [48]. The study involved 24 adults with type 1 diabetes who wore all three sensors in parallel, with comparator measurements obtained using venous laboratory analyzers (YSI 2300, Cobas Integra) and a capillary blood glucose meter (Contour Next) [48].
The results demonstrate that the accuracy of all CGM systems varies depending on the comparator method used for evaluation, highlighting a fundamental challenge in standardizing performance assessment for in-vivo biosensors [48] [45].
Table 1: Overall System Accuracy (MARD) Against Different Comparator Methods [48]
| CGM System | MARD vs. YSI (Venous) | MARD vs. INT (Venous) | MARD vs. CNX (Capillary) |
|---|---|---|---|
| FreeStyle Libre 3 (FL3) | 11.6% | 9.5% | 9.7% |
| Dexcom G7 (DG7) | 12.0% | 9.9% | 10.1% |
| Medtronic Simplera (MSP) | 11.6% | 13.9% | 16.6% |
Table 2: Performance Across Glycemic Ranges (Based on YSI Comparator) [48]
| CGM System | Hypoglycemic Range | Normoglycemic Range | Hyperglycemic Range |
|---|---|---|---|
| FreeStyle Libre 3 (FL3) | Less Accurate | More Accurate | More Accurate |
| Dexcom G7 (DG7) | Less Accurate | More Accurate | More Accurate |
| Medtronic Simplera (MSP) | More Accurate | Less Accurate | Less Accurate |
Beyond factory-calibrated systems, research explores the impact of algorithm design and optional calibration. A study on the CE-marked CareSens Air (CSAir) CGM system compared its original manual calibration algorithm to an updated algorithm with optional calibrations [47]. The updated algorithm demonstrated superior performance, improving the overall MARD from 9.9% to 8.7% and the 20/20 agreement rate from 90.1% to 93.9% [47]. This underscores that algorithm refinements can significantly enhance accuracy even for the same hardware.
Furthermore, an investigation into a novel, calibratable real-time CGM device (QT AIR) based on FreeStyle Libre technology demonstrated that calibration could drastically improve its performance [46]. The MARD was reduced from 20.63% (uncalibrated) to 12.39% in an outpatient setting, and to 7.24% in a controlled in-hospital setting [46].
Experimental Protocols for CGM Algorithm Validation
The performance data cited above were generated using rigorous clinical protocols designed to comprehensively evaluate CGM accuracy under static and dynamic glycemic conditions.
Parallel Sensor Wear and Comparator Measurements
The 2025 comparative study of FL3, DG7, and MSP followed a design where each participant wore sensors from all three systems simultaneously on the upper arms for up to 15 days [48]. This approach minimizes inter-subject variability for a more direct comparison. Key aspects included:
- Reference Methods: Three different comparator methods were used in parallel during frequent sampling periods: the YSI 2300 STAT PLUS laboratory analyzer (glucose oxidase-based), the COBAS INTEGRA 400 plus Analyzer (hexokinase-based), and the Contour Next capillary blood glucose meter [48].
- Measurement Frequency: During the in-clinic sessions, venous (YSI, INT) and capillary (CNX) comparator measurements were taken every 15 minutes over seven hours [48].
Dynamic Glucose Excursion Testing
A critical component of modern CGM validation is testing during controlled glycemic excursions. The study by [48] employed a standardized glucose manipulation procedure to induce clinically relevant scenarios [48]:
- Controlled Hyperglycemia: Participants consumed a carbohydrate-rich breakfast followed by a delayed insulin bolus.
- Induced Hypoglycemia: Insulin was used to guide glucose levels downward.
- Rapid Glucose Fluctuations: Mild exercise and fast-absorbed carbohydrates were used to create rising and falling glucose trends.
- Stable Normoglycemia: The procedure concluded with a period of stable glucose levels.
This protocol ensures a sufficient distribution of data across all glycemic ranges and dynamic conditions, which is essential for thoroughly testing the predictive and smoothing capabilities of CGM algorithms [48] [46].
The following diagram illustrates this standardized testing workflow.
Data and Accuracy Analysis
Post-data collection, the analysis involves several standardized steps:
- Data Pairing: CGM readings (stored automatically every 5 minutes) are paired with the temporally closest comparator measurement, typically within a ±5-minute window [48] [47].
- Accuracy Metrics: Key metrics are calculated from the paired data, including:
- Mean Absolute Relative Difference (MARD): The primary metric for analytical point accuracy [48] [47] [45].
- 20/20 Agreement Rate (AR): The percentage of CGM values within ±20 mg/dL (±20%) of the reference value for glucose concentrations below (above) 100 mg/dL [47].
- Error Grid Analysis (EGA): Used to assess clinical accuracy, such as the Clarke Error Grid or the newer Diabetes Technology Society Error Grid (DTSEG), which categorizes point pairs into zones of clinical risk [48] [47] [49].
Conceptual Framework of CGM Algorithm Operation
CGM systems function by measuring glucose in the interstitial fluid, not blood. Advanced algorithms are crucial to account for the physiological time lag (5-10 minutes) between blood and interstitial glucose concentrations, especially during rapid glucose changes [45]. Furthermore, they must process the raw sensor signal, which is subject to noise and sensitivity drift due to factors like biofouling [45].
The following diagram outlines the core operational workflow of a CGM algorithm, from signal acquisition to final display.
The Scientist's Toolkit: Research Reagent Solutions
The validation of CGM algorithms and systems relies on a suite of essential reagents and instruments. The following table details key items used in the featured studies.
Table 3: Essential Research Reagents and Instruments for CGM Validation
| Item Name | Function/Application | Relevance to CGM Research |
|---|---|---|
| YSI 2300 STAT PLUS Analyzer | Laboratory-grade glucose analyzer using a glucose oxidase method. | Considered a gold-standard reference method for venous blood glucose measurement in clinical trials [48] [49]. |
| Cobas Integra 400 Plus Analyzer | Laboratory analyzer using a hexokinase-based method for glucose measurement. | Used as an alternative venous plasma reference method to compare and contrast CGM performance [48]. |
| Contour Next Meter | Handheld self-monitoring blood glucose (SMBG) system. | Serves as a capillary whole blood reference and is commonly used for mandatory or optional user calibration of CGM systems [48] [47]. |
| Glucose Oxidase (GOx) | Enzyme used as the biorecognition element in most electrochemical CGM sensors. | Catalyzes the oxidation of glucose, producing an electrical current signal proportional to glucose concentration; the foundation of the biosensor [44] [50] [51]. |
| Prussian Blue | Electrochemical mediator. | Deposited on sensor electrodes to facilitate electron transfer, lowering the operating potential and reducing the effect of interfering substances, thereby enhancing accuracy [51]. |
| 3D-Printed Microneedle Array | Minimally invasive platform for biosensing. | Used in research to develop novel, painless sensor designs that access interstitial fluid in the dermis, representing a future direction for CGM technology [51]. |
The accuracy of in-vivo biosensing for research and clinical diagnostics is fundamentally governed by the biological medium in which measurements occur. The selection between whole blood, interstitial fluid (ISF), and various proxy media involves critical trade-offs between physiological relevance, technical feasibility, and analytical performance. This guide provides an objective comparison of these media, with a specific focus on how calibration methods must be adapted to account for inherent physiological and technological differences. Continuous Glucose Monitors (CGMs), which primarily sample from ISF, serve as a pivotal case study in managing the complex relationship between a proxy medium (ISF) and the reference standard (whole blood) [52]. The calibration practices employed directly impact the key metric of accuracy—the Mean Absolute Relative Difference (MARD)—across different sensing platforms and media [21].
Physiological and Technical Profiles of Biosensing Media
The core challenge in media selection stems from the distinct compositions and dynamics of each fluid. Whole blood represents the definitive clinical standard for analytes like glucose, offering a direct reflection of systemic concentrations. Its use is ubiquitous in central laboratory testing and point-of-care (POC) fingerstick devices. However, its invasive sampling profile limits continuous monitoring applications [53].
In contrast, Interstitial Fluid (ISF) is a filtrate of blood plasma that bathes the cells in tissues. It serves as the primary measurement medium for most subcutaneous CGMs. The key technical challenge is the physiological lag that can exist between blood and ISF glucose concentrations, particularly during periods of rapid glycemic change. The primary advantage of ISF is its accessibility for minimally invasive, long-term sensor implantation [52].
Proxy Media, such as cell culture supernatants or engineered synthetic fluids, are used in laboratory and early-stage biosensor development. They provide a controlled environment for validating biosensor function and calibration algorithms before progression to complex in-vivo settings. For instance, FRET-based biosensors are often first characterized in calibrated standard solutions to establish a robust performance baseline before live-cell imaging [9].
Table 1: Characteristics of Key Biosensing Media
| Media Type | Physiological Relevance | Primary Use Case | Key Limitation |
|---|---|---|---|
| Whole Blood | High (clinical gold standard) | Point-of-care testing, lab analysis | Invasive sampling; not suitable for continuous monitoring |
| Interstitial Fluid (ISF) | Moderate (correlated with blood) | Subcutaneous continuous monitors (e.g., CGMs) | Physiological time lag vs. blood |
| Proxy Media (in-vitro) | Low (controlled composition) | Biosensor R&D; method calibration | Does not replicate full in-vivo complexity |
Quantitative Comparison of CGM Performance Across Media
The performance of commercially available CGMs, which predominantly sense in ISF, provides the most direct real-world data for comparing media accuracy. The table below summarizes key performance metrics for leading systems, using MARD as the primary indicator of accuracy against blood glucose references. A lower MARD indicates closer agreement between the ISF reading and the blood standard [52].
Table 2: Performance Metrics of Continuous Glucose Monitors (ISF vs. Blood)
| CGM Device | Reported MARD (%) | Wear Time (Days) | Warm-up Time | Key Feature |
|---|---|---|---|---|
| Dexcom G7 | 8.2% (Adults) [52] | 10 [54] | 30 minutes [52] | Real-time data to smart devices [53] |
| Abbott FreeStyle Libre 3 | ~8.9% [52] | 14 [52] | 1 minute (no scan) [52] | No fingerstick calibration required [52] |
| Medtronic Guardian 4 | 9-10% [52] | 7 [52] | Not specified | Seamless integration with Medtronic pumps [52] |
| Eversense E3 | 8.5% [54] | 180 [54] | 24 hours [54] | Long-term implantable; removable transmitter [52] |
Experimental Data on Calibration Impact
A 2025 feasibility study in an ICU setting directly investigated how POC blood glucose calibration impacts the accuracy of a factory-calibrated CGM (Dexcom G6). The study defined validation as a CGM reading being within ±20% of the POC BG for values ≥100 mg/dL or ±20 mg/dL for values <100 mg/dL. The results demonstrated that calibration significantly improved device performance in a challenging clinical environment [21].
Table 3: Impact of POC Blood Glucose Calibration on CGM Accuracy (ICU Study)
| Time Point | Validation Rate (%) | MARD (%) |
|---|---|---|
| At Calibration | Not Applicable | 25.0% |
| 6 Hours Post-Calibration | 72.6% | 9.6% |
| 12 Hours Post-Calibration | 66.7% | 12.7% |
| 24 Hours Post-Calibration | 77.8% | 13.2% |
Experimental Protocols for Calibration and Validation
Protocol 1: FRET Biosensor Calibration Using Engineered Standards
This protocol, adapted from a 2025 methodology paper, is designed for calibrating FRET-based biosensors in live-cell imaging, providing a framework for managing signal variability in proxy media and cellular environments [9].
Objective: To generate normalized FRET ratios that are independent of imaging parameters (e.g., laser intensity, detector sensitivity) by using internal calibration standards.
Materials:
- FRET Biosensors: Genetically encoded unimolecular biosensors (e.g., CFP-YFP FRET pair).
- Calibration Standards: Engineered "FRET-ON" and "FRET-OFF" cell lines, where the FRET efficiency is constitutively high or low.
- Control Cell Lines: Donor-only and acceptor-only expressing cells.
- Imaging Setup: Confocal or widefield microscope capable of spectral imaging or sensitized emission FRET.
Methodology:
- Cell Preparation: Plate cells expressing the biosensor of interest and the calibration standards (FRET-ON, FRET-OFF, donor-only, acceptor-only) in a barcoded fashion or on separate dishes.
- Image Acquisition: Acquire images of all cell types under identical, steady-state illumination conditions. Collect donor and acceptor channel emissions upon donor excitation.
- Signal Correction (Using Controls):
- Use donor-only cells to calculate spectral bleed-through (SBT) of donor emission into the acceptor channel.
- Use acceptor-only cells to calculate the degree of direct acceptor excitation.
- Calibration Curve Generation:
- Calculate the apparent FRET ratio (acceptor emission / donor emission) for the FRET-ON and FRET-OFF standards.
- These two points establish a calibration curve that relates the apparent FRET ratio to the actual FRET efficiency.
- Normalization: For each experimental condition, normalize the raw FRET ratio from the biosensor-expressing cells against the calibration curve derived from the standards imaged in the same session.
Data Analysis: The calibrated FRET ratio corrects for fluctuations in imaging parameters and enables a more reliable determination of actual FRET efficiency and its dynamics over time [9].
Protocol 2: Point-of-Care Blood Glucose Calibration for CGM in Critical Care
This protocol is based on a 2025 clinical feasibility study investigating hybrid CGM/POC BG protocols in ICU patients, representing a critical practice for aligning ISF readings with blood standards [21].
Objective: To improve and validate the accuracy of a subcutaneous CGM in critically ill patients by performing timed calibrations against POC blood glucose measurements.
Materials:
- Continuous Glucose Monitor: A factory-calibrated CGM system (e.g., Dexcom G6).
- Point-of-Care Blood Glucose Meter: An FDA-cleared blood glucose monitor with test strips and lancets.
- Calibration Timer.
Methodology:
- Initial Validation: Upon CGM placement, compare the CGM reading to a POC BG measurement. Validation is achieved if the CGM value is within ±20% of the POC BG for values ≥100 mg/dL or ±20 mg/dL for values <100 mg/dL.
- Calibration Trigger: A calibration is performed if the CGM consistently fails validation checks or as per a predefined clinical protocol (e.g., every 12 hours).
- Calibration Procedure:
- Perform a POC BG test using a fingerstick capillary blood sample.
- Within 5-10 minutes of the POC test, enter the BG value into the CGM device or its associated display app to initiate the calibration.
- Ensure the sensor is in a stable state (not during a period of rapid glucose change) at the time of calibration.
- Post-Calibration Validation: Continue to perform validation checks against POC BG at 6, 12, and 24 hours after calibration to monitor the decay of calibration accuracy.
Data Analysis: Calculate the MARD for the CGM before and after calibration against the POC BG values. Track the validation rates over time to determine the optimal calibration frequency for the patient population [21].
Visualization of Core Concepts
CGM Calibration Workflow
The following diagram illustrates the hybrid protocol for calibrating an ISF-based CGM against a blood glucose standard, a key strategy for managing inter-media discrepancies.
FRET Biosensor Calibration Logic
This diagram outlines the logical workflow for calibrating FRET biosensor signals using engineered standards to achieve quantitative measurements independent of imaging conditions.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for conducting rigorous experiments in biosensor calibration and media comparison studies.
Table 4: Essential Research Reagents and Materials
| Item | Function/Application | Example Use Case |
|---|---|---|
| FRET Calibration Standards | Genetically engineered cells with fixed high/low FRET efficiency. | Normalizing FRET biosensor signals in live-cell imaging against a known reference [9]. |
| Point-of-Care (POC) Glucose Meter | Provides reference whole blood glucose values for calibration. | Validating and calibrating ISF-based CGM readings in clinical or research settings [21]. |
| Spectral Control Cell Lines | Cells expressing only the donor or acceptor fluorophore. | Quantifying and correcting for spectral crosstalk (bleed-through) in FRET experiments [9]. |
| Continuous Glucose Monitor (CGM) | Measures glucose concentration in the interstitial fluid (ISF). | Studying the dynamics and correlation between ISF and blood glucose in vivo [52] [54]. |
| Potentiostat | Instrument for controlling and measuring electrochemical signals. | Characterizing the performance of electrochemical biosensors in various media [55]. |
Optimizing Calibration Protocols and Overcoming Practical Limitations
Mitigating Early Sensitivity Attenuation and Signal Dropouts
In the pursuit of reliable in-vivo biosensing, researchers and drug development professionals face significant challenges in maintaining sensor accuracy. Early Sensitivity Attenuation (ESA) and signal dropouts consistently bias sensor output downward, compromising data integrity for long-term monitoring and clinical decision-making. ESA typically occurs within the first few hours of sensor initiation, while dropouts are shorter, unpredictable signal losses that can occur independently of sensor age [56]. This guide objectively compares current methodological approaches for mitigating these issues, providing experimental data and protocols to inform selection of optimal calibration strategies for specific research applications.
Comparative Analysis of Mitigation Strategies
The table below summarizes the core operational principles, advantages, and limitations of current primary strategies for addressing ESA and signal dropouts.
Table 1: Comparison of Mitigation Strategies for ESA and Signal Dropouts
| Strategy | Core Mechanism | Key Advantages | Documented Limitations |
|---|---|---|---|
| Dynamic Calibration Algorithms [56] | Uses adjustment maps balancing over/under-calibration risk based on a priori information; defers calibration if system checks fail | Reduces unnecessary recalibration; improves user experience; mitigates effects of signal attenuation | Requires robust reference measurement pairing; performance depends on calibration timing and signal stability checks |
| Chemical Signal Amplification [57] | Amplifies signal transduction per biorecognition event using polymerization or nanocatalysts | Dramatically enhances detection signal; improves limit of detection; enables minute analyte quantification | Complex reaction optimization; potential for nonspecific amplification in complex matrices |
| Feedback Amplifier Circuits [58] | Incorporates positive/negative feedback cascade amplifiers in whole-cell biosensor design | Increases output signal intensity (1.11-2.64x); reduces response time (6h to 4h); expands linear range | Primarily demonstrated for cadmium detection; requires genetic engineering of cellular components |
| AI/ML-Enhanced Signal Processing [59] [60] | Applies machine learning models for signal denoising, drift correction, and anomaly detection | Adapts to complex patterns; handles multivariate nonlinear relationships; enables predictive diagnostics | Requires extensive training datasets; model interpretability challenges; computational resource demands |
| Transfer Learning Calibration [61] | Transfers models from pre-calibrated sensors to new sensors with minimal additional calibration | Reduces calibration samples by up to 99.3% (from 10 days to ~2 hours); addresses manufacturing tolerances | Initial multi-sensor dataset requirement; potential domain adaptation challenges |
Quantitative Performance Assessment
The following experimental data, compiled from published studies, enables direct comparison of method efficacy across key performance metrics.
Table 2: Quantitative Performance Metrics of Mitigation Strategies
| Method Category | Reported Sensitivity Improvement | Limit of Detection Enhancement | Signal-to-Noise Gain | Response Time Impact |
|---|---|---|---|---|
| Polymerization Amplification [57] | Not quantified | 1 fM (DNA hybridization); 2.19 fmol/spot (SPR) | Not quantified | Not quantified |
| Nanocatalyst Amplification [57] | Not quantified | 0.8-3.1 pg/mL (lateral flow immunoassay) | Not quantified | Not quantified |
| Feedback Amplifier [58] | Specificity increased from 17.55 to 23.29 | 0.1 nM Cd²⁺ (maintained) | Fluorescence output increased 1.11-2.64x | Reduced from 6h to 4h |
| ML-Based Calibration [59] | RMSE = 0.143 (stacked ensemble) | Not specified | Key parameters identified: enzyme amount, pH, analyte concentration | Not quantified |
| Transfer Learning [61] | Not quantified | ~18 ppb acetone (with 99.3% calibration reduction) | Not quantified | Not quantified |
Experimental Protocols
Dynamic Calibration with Adjustment Maps
Protocol Objective: Implement sensitivity calibration that balances over-calibration and under-calibration risks using a priori information [56].
Workflow:
- Define System Checks: Establish criteria for validating sensor signal stability and physiological feasibility before calibration attempts
- Receive Calibration Request: Initiate process upon user command or system trigger
- Acquire Reference Measurement: Pair reference observation (e.g., blood glucose measurement) with corresponding sensor data
- Conduct Initial Calibration: Use first predetermined duration of reference observation paired with sensor data up to calibration time
- Update Calibration: Apply same reference measurement at second predetermined duration spanning first duration plus additional period
- Apply Adjustment Map: Utilize predefined maps balancing calibration risks based on historical performance data
- Defer if Unstable: Postpone calibration if system checks indicate signal instability or dropout conditions
Key Parameters:
- Reference observation duration windows (e.g., 5-second sampling periods)
- Signal stability thresholds for calibration deferral
- Adjustment map weighting factors for risk balance
Polymerization-Based Signal Amplification
Protocol Objective: Enhance detection sensitivity through radical polymerization-triggered signal amplification [57].
Workflow:
- Surface Functionalization: Immobilize capture molecules (DNA, antibodies) on substrate surface
- Target Binding: Incubate with sample for specific target recognition and binding
- Initiator Conjugation: Attach polymerization initiators (e.g., bromoisobutyrroyl bromide) to probe molecules
- Polymerization Reaction: Apply monomer solution (HEMA) with catalyst mixture (CuCl, CuBr₂, 2,2'-bipyridyl)
- Signal Development: Grow polyHEMA film with opaqueness indicating target presence
- Quantitative Measurement: Correlate film opacity or thickness to target concentration
Key Parameters:
- Monomer concentration: 2-hydroxyethyl methacrylate (HEMA)
- Catalyst ratio: CuCl/CuBr₂/bipyridyl optimized for controlled polymerization
- Reaction time and temperature controlled for quantitative correlation
AI-Enhanced Signal Processing Framework
Protocol Objective: Implement machine learning for biosensor signal prediction and noise reduction [59].
Workflow:
- Dataset Preparation: Systematically generate data encompassing variations in:
- Enzyme amount
- Glutaraldehyde concentration
- pH
- Conducting polymer scan number
- Analyte concentration
- Model Training: Train and evaluate 26 regression models across six families:
- Linear models
- Tree-based methods (Random Forest, XGBoost)
- Kernel-based models (SVR)
- Gaussian Process Regression
- Artificial Neural Networks
- Stacked ensembles
- Model Validation: Employ 10-fold cross-validation with four performance metrics (RMSE, MAE, MSE, R²)
- Feature Interpretation: Apply SHAP and permutation analysis to identify influential parameters
- Implementation: Deploy best-performing model for real-time signal correction
Key Parameters:
- Cross-validation: 10-fold stratified
- Performance thresholds: RMSE < 0.15, R² ≈ 1.00
- Key identified features: Enzyme amount, pH, analyte concentration
Signaling Pathways and Workflows
Diagram 1: Dynamic calibration workflow implementing system checks and adjustment maps to mitigate ESA [56].
Diagram 2: Chemical signal amplification pathway using polymerization for enhanced sensitivity [57].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for ESA and Dropout Mitigation Studies
| Reagent/Material | Function | Example Application |
|---|---|---|
| Atom Transfer Radical Polymerization Components [57] | Signal amplification through controlled polymer growth | DNA hybridization detection; protein sensing |
| Enzyme-Linked Biosensor Systems [59] | Biorecognition element for specific analyte detection | Glucose monitoring; pathogen detection |
| Fluorescent Protein FRET Pairs [9] | Genetically encoded biosensors for live-cell monitoring | Kinase activity tracking; molecular interaction studies |
| Carbon Nanomaterials [62] | Electrode material with high conductivity and antifouling properties | Electrochemical sensing in complex biological matrices |
| Metal Oxide Semiconductors [61] | Gas sensing material for volatile compound detection | Indoor air quality monitoring; breath analysis |
| Whole-Cell Biosensor Components [58] | Cellular systems with genetic circuits for detection | Heavy metal detection; environmental monitoring |
The comparative analysis presented demonstrates that effective mitigation of Early Sensitivity Attenuation and signal dropouts requires strategic selection of complementary approaches. Dynamic calibration algorithms provide immediate operational benefits for in-vivo monitoring systems, while chemical signal amplification offers substantial sensitivity enhancement for in-vitro applications. Emerging approaches utilizing machine learning and transfer learning show exceptional promise for reducing calibration burden and adapting to complex signal patterns, particularly valuable for long-term studies and commercial sensor deployment. Researchers should prioritize methods aligned with their specific biosensing platform, matrix complexity, and operational duration requirements, considering that hybrid approaches often yield optimal results for challenging applications in drug development and clinical research.
In the field of in-vivo biosensing, the accuracy of molecular measurements is not solely determined by the sensor's design but is profoundly influenced by the calibration strategy employed. A critical principle underpinning reliable data is the meticulous matching of calibration conditions to the actual measurement environment. This guide objectively compares the performance of different calibration methodologies, demonstrating that aligning media, temperature, and biological context during calibration with those encountered during in-vivo measurement is paramount for achieving clinically relevant accuracy. Data from recent studies on electrochemical, optical, and magnetic resonance-based sensors provide experimental proof that neglecting this alignment introduces significant error, compromising the value of research and its translation to clinical applications.
Comparative Analysis of Calibration Method Performance
The table below summarizes experimental data from key studies, comparing the accuracy and precision achieved under different calibration approaches.
Table 1: Performance Comparison of Calibration Methods for In-Vivo Biosensing
| Sensor Technology | Target Analytic | Optimal Calibration Condition | Suboptimal Calibration Condition | Accuracy & Precision (Optimal) | Accuracy & Precision (Suboptimal) | Key Experimental Finding |
|---|---|---|---|---|---|---|
| Electrochemical Aptamer-Based (EAB) Sensor [3] | Vancomycin (in blood) | Fresh whole blood at 37°C | Room temperature calibration; Aged commercial blood | Better than ±10% accuracy in clinical range | Overestimation of concentration; >10% error | Calibration temperature and blood age significantly impact signal gain and binding curve midpoint. |
| FRET Biosensor [9] | Kinase Activity (live cells) | In-cell calibration with FRET-ON/OFF standards | Uncalibrated FRET ratio imaging | Enables determination of actual FRET efficiency | FRET ratio is highly sensitive to imaging parameters and photobleaching | Calibration using engineered standards corrects for imaging fluctuations, restoring reciprocal donor/acceptor trends. |
| Hybrid PRF/T1 MR Thermometry [63] | Temperature in fat tissue | Ex vivo T1-temperature coefficient for fat (1.9%/°C) | PRF shift method alone in fat | Precision of 1.93°C ± 0.60°C in fat | Largely insensitive to temperature changes in fat | The PRF method is ineffective for fat; accurate thermometry requires a tissue-specific T1-temperature coefficient. |
| Metal Oxide Semiconductor (MOS) Gas Sensor [61] | Acetone (in air) | Transfer Learning Calibration Transfer | Factory calibration without transfer | RMSE of ~18 ppb (with 99.3% less calibration data) | High error due to manufacturing tolerances and drift | Advanced calibration transfer methods drastically reduce the calibration burden for new sensor units. |
Detailed Experimental Protocols & Methodologies
Protocol: EAB Sensor Calibration in Whole Blood
This protocol, derived from the work on vancomycin-detecting EAB sensors, details the steps for achieving high-fidelity calibration [3].
- Sensor Interrogation: Interrogate the EAB sensor using Square Wave Voltammetry (SWV) at two carefully selected frequencies—one "signal-on" and one "signal-off" frequency. The choice of frequencies must be optimized for the measurement temperature.
- Data Conversion: Convert the acquired voltammograms into Kinetic Differential Measurement (KDM) values. This is calculated by subtracting the normalized peak currents at the signal-on and signal-off frequencies and then dividing by their average. This step corrects for signal drift and enhances measurement gain.
- Calibration Curve Generation: In freshly collected, undiluted whole blood maintained at 37°C, collect KDM values over a range of target concentrations. For vancomycin, the clinically relevant range (e.g., 6 to 42 µM) should be densely sampled.
- Curve Fitting: Fit the averaged KDM values to a Hill-Langmuir isotherm to generate a calibration curve. The model is defined as:
KDM = KDM_min + ( (KDM_max - KDM_min) * [Target]^nH ) / ( [Target]^nH + K_1/2^nH )whereKDM_minandKDM_maxare the minimum and maximum KDM values,nHis the Hill coefficient, andK_1/2is the binding curve midpoint. - Measurement and Quantification: For unknown samples measured under the same conditions (fresh whole blood, 37°C), apply the fitted parameters to convert the observed KDM value into a target concentration using the derived equation.
Protocol: FRET Biosensor Calibration Using Engineered Standards
This protocol outlines the use of calibration standards to normalize FRET biosensor signals in live cells, mitigating the effects of variable imaging conditions [9].
- Standard Preparation: Generate barcoded cell lines expressing engineered "FRET-ON" and "FRET-OFF" standards. These are constructs where the donor and acceptor fluorescent proteins are locked in high-efficiency and low-efficiency FRET conformations, respectively.
- Sample Preparation: Mix the calibration standard cells with cells expressing the biosensor of interest. This can be done in separate wells or, ideally, within the same population using a barcoding system to identify different cell types.
- Image Acquisition: Image the mixed cell population under the experimental conditions. Acquire signals from both the donor and acceptor channels.
- Signal Normalization: Use the signals from the FRET-ON and FRET-OFF standards to create a normalization curve. This calibration adjusts the raw FRET ratio (acceptor/donor signal) from the biosensor cells, correcting for fluctuations in laser intensity, detector sensitivity, and path length.
- Efficiency Calculation: The calibrated FRET ratio becomes independent of imaging settings, allowing for a more accurate determination of the actual FRET efficiency and enabling reliable comparison across different experiments and long-term imaging sessions.
Protocol: T1-Based MR Thermometry for Fatty Tissues
This protocol describes the calibration and application of T1-based thermometry for monitoring temperature in fat tissue during MR-guided focused ultrasound surgery, where the standard PRF method fails [63].
- Ex Vivo Calibration:
- Sample Collection: Harvest adipose tissue (e.g., from a rabbit model).
- T1 Mapping: Using an inversion recovery sequence, acquire T1 maps of the fat sample while it is submerged in a water bath at multiple known temperatures across the range of interest (e.g., from body temperature to ablative temperatures).
- Coefficient Determination: For each pixel, plot T1 values against temperature. Perform a linear least-squares fit to determine the mean T1-temperature coefficient (
dT1/dT), expressed in %/°C. The study found a coefficient of 1.9%/°C ± 0.2%/°C for fat.
- In Vivo Application:
- Baseline Acquisition: Acquire a baseline T1 map of the target tissue (e.g., using a variable flip angle method) before heating.
- Dynamic Imaging: During the thermal procedure (e.g., sonication), run a sequence capable of simultaneous PRF (for aqueous tissues) and T1 mapping (e.g., SR-VFA-SoS) with appropriate spatial and temporal resolution.
- Temperature Calculation: Convert the measured changes in T1 (
ΔT1) to temperature change (ΔT) in fat tissue using the pre-determined coefficient:ΔT = (ΔT1 / T1_ref) / (dT1/dT), whereT1_refis the baseline T1 value.
Signaling Pathways, Workflows, and Logical Relationships
EAB Sensor Calibration and Measurement Workflow
The following diagram illustrates the multi-step process of calibrating an EAB sensor and using that calibration to determine unknown concentrations in a sample.
Logical Relationship: Calibration Condition vs. Measurement Accuracy
This diagram conceptualizes the core thesis that matching the calibration environment to the measurement environment is critical for minimizing systematic error in biosensing.
The Scientist's Toolkit: Essential Research Reagents & Materials
This table details key materials and their functions for implementing the rigorous calibration methodologies discussed in this guide.
Table 2: Essential Research Reagents and Solutions for In-Vivo Calibration
| Item Name | Function & Application | Critical Specification |
|---|---|---|
| Fresh Whole Blood | The optimal calibration matrix for EAB sensors and other blood-borne analyte sensors. Provides the correct chemical and cellular environment [3]. | Undiluted, freshly collected (<1 day old), from the relevant species (e.g., rat, human). |
| Genetically Encoded FRET Standards | Cells expressing FRET-ON and FRET-FF constructs. Used as internal calibration standards for live-cell FRET imaging to normalize against instrumental noise [9]. | Stable cell lines with locked high/low FRET efficiency. |
| Reference Thermometer (RTD PT100) | A highly accurate temperature sensor for calibrating thermal monitoring systems (e.g., in phantom studies or bath calibration) [64]. | Traceable calibration, high accuracy (e.g., ±0.1°C). |
| Dry-Well Calibrator with Reference Thermometer | A stable heat source for calibrating temperature sensors and probes as a complete system, ensuring traceability [65]. | High accuracy, multiple insert sizes for different probes. |
| Tissue-Mimicking Phantoms | Stable, reproducible materials (e.g., water-saturated foams, gels) for initial method validation and calibration of physical sensors without biological variability [64]. | Known, stable mechanical/thermal properties over the experimental range. |
| Variable Flip Angle (VFA) MRI Sequence | An MR sequence (e.g., SR-VFA-SoS) capable of simultaneous T1 mapping for fat thermometry and PRF shift for aqueous tissue thermometry [63]. | Capable of 3D acquisition with sufficient spatial (~1.5mm) and temporal (~2s) resolution. |
Accounting for Blood Age and Sample Processing Artifacts
In the field of in-vivo biosensing research, the accuracy of molecular measurements is fundamentally dependent on robust calibration methods that account for biological variables. Blood age—the time elapsed since blood sample collection—and sample processing artifacts introduced during handling and storage are two critical, yet often overlooked, factors that can significantly compromise data integrity [3] [66]. These variables introduce matrix effects and signal drift that, if unaddressed, lead to inaccurate concentration readings and flawed biological interpretations.
The pursuit of measurement accuracy has driven innovation in calibration strategies across different biosensing platforms. This guide provides an objective comparison of current calibration methodologies, evaluating their performance in controlling for pre-analytical variables. We focus specifically on approaches for in-vivo biosensing and blood-based biomarker analysis, presenting experimental data to help researchers select optimal calibration frameworks for their specific applications.
Comparative Analysis of Calibration Methods
The following analysis compares three distinct calibration approaches, highlighting their respective capabilities in managing blood age and processing artifacts.
Table 1: Performance Comparison of Biosensor Calibration Methods
| Calibration Method | Key Principles | Accuracy in Fresh Blood | Robustness to Blood Age | Implementation Complexity | Best Use Cases |
|---|---|---|---|---|---|
| Triple-Mode Biosensing | Cross-validation via three independent detection mechanisms (e.g., colorimetric, fluorescence, photothermal) [67]. | High (self-validating) | High (multiple signals reduce noise) | High (requires nanomaterial synthesis and multi-signal integration) | Complex biological matrices; ultrasensitive detection requiring high reliability |
| Media-Matched Calibration (EAB Sensors) | Calibration in freshly-collected, body-temperature blood that matches measurement conditions [3]. | ±10% accuracy for vancomycin in clinical range | Low (significant signal degradation in aged blood) | Moderate (requires fresh blood collection) | In-vivo therapeutic drug monitoring; real-time metabolite sensing |
| Multiplexed FRET Standardization | Uses engineered "FRET-ON" and "FRET-OFF" cells as internal standards to normalize signals across imaging sessions [9] [68]. | High (calibrated ratios independent of imaging settings) | Not applicable (cellular imaging) | Moderate (requires cell line development and barcoding) | Live-cell imaging of molecular activities; long-term tracking of biochemical processes |
Key Experimental Findings on Blood Age Effects
Direct investigation into blood age effects reveals significant calibration implications:
Signal Degradation Over Time: Electrochemical aptamer-based (EAB) sensors challenged in commercially sourced bovine blood (approximately 1 day old) showed lower signal gain compared to fresh blood, which would lead to overestimated vancomycin concentrations [3]. This difference persisted when comparing 1-day-old versus 14-day-old blood from the same draw, confirming that blood age itself impacts sensor response independently of processing method.
Temperature Interaction: The effect of blood age compounds with temperature mismatch. EAB sensor calibration curves differ significantly between room temperature (≈25°C) and body temperature (37°C), with some interrogation frequencies showing up to 10% higher signal at room temperature across the clinical concentration range [3]. Applying room-temperature calibrations to body-temperature measurements causes substantial concentration underestimates.
Experimental Protocols for Assessing Blood Age Effects
Protocol: Evaluating Blood Age Impact on EAB Sensor Calibration
This methodology details the procedure for quantifying how blood age affects biosensor accuracy, based on experimental approaches used in recent biosensing research [3].
Materials and Reagents:
- Freshly collected whole blood (rat or human, anticoagulated)
- Commercial sourced whole blood (for comparison)
- Target analyte (e.g., vancomycin hydrochloride)
- Phosphate-buffered saline (PBS)
- Electrochemical aptamer-based sensors specific to target
Procedure:
- Blood Collection and Aging: Collect fresh whole blood using standard venipuncture techniques with EDTA or heparin anticoagulant. Divide into aliquots for immediate use and aged samples (store at 4°C for specified durations: 1, 3, 7, and 14 days).
- Sensor Preparation: Fabricate EAB sensors according to established protocols, with aptamers modified with redox reporters and immobilized on gold electrodes.
- Calibration Curve Generation: For each blood age condition (fresh, 1-day, 3-day, 7-day, 14-day):
- Spike blood samples with target analyte across clinically relevant concentration range (e.g., for vancomycin: 0, 6, 12, 24, 42 µM)
- Measure sensor response using square wave voltammetry at both signal-on and signal-off frequencies
- Calculate Kinetic Differential Measurement (KDM) values: KDM = (Normalized signal-off current - Normalized signal-on current) / Average of both
- Fit KDM values to Hill-Langmuir isotherm to generate calibration curves for each condition
- Parameter Comparison: Quantify differences in key calibration parameters (KDMmax, K1/2, nH) across blood age conditions
- Accuracy Assessment: Apply different calibration curves to known concentration samples; calculate accuracy as: % Accuracy = 100 × (Expected Concentration - Observed Concentration) / Expected Concentration
Protocol: Triple-Mode Biosensor Validation in Complex Matrices
This procedure outlines validation of multi-mode biosensors against artifacts, based on approaches described in Mansouri et al. [67].
Materials and Reagents:
- Triple-mode biosensor platform (colorimetric/fluorescence/photothermal)
- Target analytes and potential interfering substances
- Nanomaterial-enhanced detection substrates
- Smartphone-based readout device or spectrophotometer
Procedure:
- Sensor Calibration in Pristine Media:
- Prepare standard solutions of target analyte in simple buffer
- Measure response across all three detection modes
- Establish baseline calibration curves for each mode independently
- Matrix Effect Assessment:
- Spike complex matrices (fresh blood, aged blood, processed samples) with known analyte concentrations
- Measure responses across all three detection modes
- Calculate recovery rates: % Recovery = 100 × (Measured Concentration in Matrix / Known Concentration)
- Cross-Validation Analysis:
- Compare results from all three detection modes
- Flag discrepancies where modes disagree beyond predetermined thresholds (e.g., >15%)
- Establish consensus value through weighted averaging of modal outputs
- Artifact Identification:
- Identify sample processing artifacts through inconsistent modal responses (e.g., colorimetric signal affected by hemolysis while fluorescence remains stable)
- Develop correction algorithms based on modal discrepancy patterns
Biological Pathways and Experimental Workflows
The following diagram illustrates the conceptual relationship between blood aging factors, their effects on biosensor signals, and calibration strategies to mitigate these effects.
This workflow illustrates how blood aging factors introduce specific artifacts that calibration strategies must address. Cellular changes like increased red cell distribution width (RDW) and biochemical alterations such as reduced antioxidant activity collectively impact sensor performance by modifying the molecular environment in which measurements occur [66]. Effective calibration approaches must therefore either match the measurement matrix precisely (media-matched calibration) or incorporate self-validation mechanisms (multi-mode biosensing) to compensate for these variables.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Biosensor Calibration Studies
| Reagent/Material | Function in Calibration Studies | Specification Notes |
|---|---|---|
| Fresh Whole Blood | Gold-standard matrix for in-vivo sensor calibration; provides native biochemical environment [3]. | Collect <2 hours before use; heparin or EDTA anticoagulant; maintain at 37°C for body-temperature simulations. |
| Electrochemical Aptamer-Based Sensors | Platform for real-time, in-vivo molecular monitoring; enables frequency-based signal manipulation (KDM) [3]. | Select aptamers with appropriate KD for target concentration range; optimize redox reporter placement. |
| Triple-Mode Biosensing Platforms | Cross-validating detection systems combining colorimetric, fluorescent, and photothermal readouts [67]. | Ensure spectral separation between modes; use nanomaterials to enhance signal amplification. |
| FRET Standard Cells | Genetically engineered "FRET-ON" and "FRET-OFF" cells for internal calibration of imaging systems [9] [68]. | Use same fluorescent protein pairs as biosensors; validate under actual experimental conditions. |
| Protein-Specific Antibodies | Tools for quantifying organ-specific proteins in blood for biological age estimation [69] [70]. | Verify specificity using knockout controls; check cross-reactivity with related proteins. |
The comparative analysis presented in this guide demonstrates that accounting for blood age and sample processing artifacts remains a significant challenge in biosensing research, with direct implications for measurement accuracy. Media-matched calibration using fresh, body-temperature blood currently provides the most straightforward path to accurate in-vivo measurements for therapeutic monitoring applications, achieving ±10% accuracy when properly implemented [3]. For more complex matrices or where fresh blood is unavailable, triple-mode biosensing approaches offer robust self-validation capabilities through multi-signal cross-correlation, though with increased implementation complexity [67].
Emerging approaches that combine elements of both strategies—such as incorporating internal standards into matrix-matched calibrations—represent promising directions for next-generation biosensing platforms. As the field advances toward increasingly multiplexed biomarker panels for biological age estimation [69] [70] and organ-specific aging tracking [70], developing calibration frameworks that simultaneously address multiple pre-analytical variables will become increasingly critical for generating reliable, reproducible data in both research and clinical applications.
Compensating for Time Lag Between Different Biological Compartments
In vivo biosensing provides unparalleled insight into dynamic biological processes, yet a significant challenge is accurately compensating for the time lag that occurs between molecular events in different cellular compartments. These temporal discrepancies can arise from delays in transcription, translation, protein modification, and transport between organelles, ultimately obscuring the true sequence of causal events in signaling pathways. For researchers and drug development professionals, this limitation complicates the interpretation of live-cell imaging data and can lead to flawed conclusions about mechanism of action. Calibration methods serve as critical tools to correct for these inherent biological delays and technical variabilities, enabling more accurate, quantitative, and temporally precise measurements.
This guide objectively compares the performance of three advanced calibration approaches: FRET-based standards, DNA strand displacement circuits, and nanomaterial-enabled self-calibrating platforms. By presenting experimental data and detailed protocols, we aim to equip researchers with the information needed to select optimal calibration strategies for their specific in vivo biosensing applications, particularly those requiring high temporal resolution across multiple cellular compartments.
Comparative Analysis of Calibration Method Performance
Table 1: Quantitative Performance Comparison of Biosensor Calibration Methods
| Method | Temporal Resolution | Spatial Compensation Capability | Key Advantages | Reported Limitations | Best-Suited Applications |
|---|---|---|---|---|---|
| FRET-Based Standards [9] | Minutes to hours | Single compartment to whole cell | • Internal control for imaging variations• Enables multiplexing with barcoding• Direct measurement of FRET efficiency | • Requires genetic engineering• Sensitive to photobleaching over long durations• Limited to FRET-capable biosensors | • Kinase activity profiling• Second messenger dynamics (e.g., Ca²⁺, cAMP)• Multiplexed signaling studies |
| DNA Strand Displacement Circuits [71] | Seconds to minutes | Not demonstrated for subcellular compartments | • Programmable logic functions (AND, OR, NOT)• Analog-to-digital conversion capability• Modular design with predictable thermodynamics | • Currently restricted to cell-free systems• Potential interference from cellular nucleases• Limited interface with protein-based biosensors | • Cell-free diagnostic applications• Processing of multiple nucleic acid inputs• Environmental monitoring |
| Nanomaterial Self-Calibrating Sensors [72] | Minutes | Not compartment-specific | • Ratiometric output minimizes matrix effects• Multimodal signals (colorimetric + fluorescence)• Enhanced stability in complex biological fluids | • Potential cytotoxicity concerns for in vivo use• Complex synthesis and functionalization• Limited biodegradability | • Detection of food contaminants and toxins• Point-of-care biomarker detection• Extracellular environmental monitoring |
Detailed Experimental Protocols for Key Calibration Methods
FRET Standard Calibration for Intracellular Biosensing
The FRET standard calibration method employs genetically encoded "FRET-ON" and "FRET-OFF" constructs to normalize signals against imaging condition variability, enabling more accurate temporal measurements across cellular compartments [9].
Experimental Protocol:
Construct Design: Engineer two calibration standards using CFP (donor) and YFP (acceptor) fluorescent proteins. For the "FRET-ON" standard, directly fuse CFP and YFP with a short, flexible linker (e.g., 5-10 amino acids) to ensure consistent high FRET. For the "FRET-OFF" standard, use a longer, rigid linker or point mutations that disrupt energy transfer while maintaining fluorescence.
Cell Preparation and Transfection:
- Culture mammalian cells (HEK293 or HeLa) in appropriate media with 10% FBS at 37°C with 5% CO₂.
- Transfect cells with FRET standard plasmids using lipid-based transfection reagents optimized for minimal cytotoxicity.
- Include untransfected controls to assess autofluorescence.
- For compartment-specific calibration, fuse localization signals (nuclear, mitochondrial, etc.) to the standards.
Image Acquisition:
- Use a confocal microscope with environmental control (37°C, 5% CO₂) maintained throughout imaging.
- Set donor excitation (typically 405-440 nm for CFP) and collect emission from both donor (460-500 nm) and acceptor (520-560 nm) channels.
- Acquire images at multiple locations with identical settings for all samples.
- Include donor-only and acceptor-only controls for spectral bleed-through correction.
Data Processing and Calibration:
- Calculate apparent FRET efficiency using the acceptor-to-donor signal ratio for each standard.
- Generate a calibration curve by plotting known FRET efficiencies of standards against measured ratios.
- Apply this calibration to correct FRET ratios from experimental biosensors in the same imaging session.
- For temporal alignment, compare calibration signals between compartments to establish lag times.
Table 2: Key Research Reagent Solutions for FRET Standard Experiments
| Reagent/Material | Function/Application | Example Specifications |
|---|---|---|
| CFP-YFP FRET Standards | Internal calibration controls | "FRET-ON" (high efficiency), "FRET-OFF" (low efficiency) constructs |
| Lipid-Based Transfection Reagent | Nucleic acid delivery | Low cytotoxicity, high efficiency for adherent cells |
| Live-Cell Imaging Medium | Maintenance of cell viability during imaging | Phenol red-free, with HEPES buffer |
| Confocal Microscope with Environmental Chamber | Image acquisition with cell viability maintenance | Temperature control (37°C), CO₂ regulation (5%), humidity control |
Figure 1: FRET Standard Calibration Workflow for Compensating Time Lags
DNA Strand Displacement Circuit Calibration
This method utilizes programmable nucleic acid circuits to process biosensor outputs, enabling logical operations and signal normalization that can account for temporal discrepancies [71].
Experimental Protocol:
Circuit Design and Preparation:
- Design toehold-mediated strand displacement gates using nucleic acid modeling software (NUPACK).
- Synthesize DNA strands commercially with HPLC purification.
- Anneal gate complexes by mixing stoichiometric ratios of strands in TM buffer (20 mM Tris, 10 mM MgCl₂, pH 8.0).
- Heat to 95°C for 5 minutes and cool slowly to room temperature over 4-6 hours.
Interfacing with Cell-Free Biosensing Systems:
- Utilize the ROSALIND (RNA Output Sensors Activated by Ligand Induction) platform or similar cell-free systems.
- Combine allosteric transcription factors (aTFs) with T7 RNA polymerase for target detection.
- Configure DNA templates with T7 promoter, aTF operator sequence, and InvadeR RNA sequence.
Signal Processing and Output:
- Combine DNA strand displacement gates with cell-free expression system.
- Add target analyte to initiate the sensing and computation cascade.
- Monitor fluorescence output in real-time using a plate reader.
- Implement logic functions (NOT, OR, AND, IMPLY) to process multiple temporal inputs.
Nanomaterial-Mediated Self-Calibrating Biosensors
This approach uses nanomaterials to generate ratiometric or multimodal signals that internally correct for environmental variabilities and temporal artifacts [72].
Experimental Protocol:
Nanomaterial Synthesis and Functionalization:
- Synthesize signal-labeled nanomaterials (quantum dots, gold nanoparticles, graphene oxide).
- Functionalize with recognition elements (antibodies, aptamers, enzymes).
- Conjugate with dual-signal reporters (fluorophore-quencher pairs, SERS tags).
Sensor Assembly and Testing:
- Immobilize functionalized nanomaterials on substrates (paper, electrodes, wells).
- Add sample containing target analyte and incubate to allow binding.
- Measure multiple signal outputs simultaneously (fluorescence, colorimetric, electrochemical).
Data Processing and Calibration:
- Calculate ratio between response signal and reference signal.
- Generate calibration curve using standard concentrations.
- Apply internal calibration to correct for matrix effects and temporal drift.
Pathway and Mechanism Diagrams for Temporal Calibration
Figure 2: Time Lag Compensation Across Cellular Compartments
The accurate compensation of time lags between biological compartments remains a significant challenge in biosensing research, with important implications for drug development and systems biology. Each calibration method offers distinct advantages: FRET standards provide the most direct approach for subcellular compartment alignment in live cells, DNA strand displacement circuits offer unparalleled programmability for signal processing, and nanomaterial-based systems deliver robust self-calibration in complex environments.
For research requiring precise temporal alignment across organelles in living cells, FRET-based calibration currently provides the most mature methodology, though it requires genetic modification of the biological system. As DNA circuit technology advances toward cellular implementation, it may offer more sophisticated temporal processing capabilities. Nanomaterial approaches show exceptional promise for extracellular and diagnostic applications where genetic manipulation is impractical.
Future methodological development should focus on combining the strengths of these approaches—perhaps through nucleic acid circuits that interface with protein-based biosensors or nanomaterials that enable both rationetric sensing and temporal processing. Such integrated systems would provide researchers with more powerful tools to deconvolve the complex temporal relationships that underlie cellular signaling and drug responses.
Adaptive Calibration Strategies for Long-Term Sensor Deployment
For researchers and drug development professionals, the long-term deployment of sensors in live systems (in-vivo) presents a significant challenge: maintaining measurement accuracy over time. Sensor drift, environmental interference, and biofouling can compromise data reliability, potentially invalidating critical research on drug pharmacokinetics or real-time biomarker tracking. Adaptive calibration strategies have emerged as a vital solution, moving beyond static, one-time calibration to dynamic methods that ensure sustained data fidelity. This guide objectively compares the performance of emerging adaptive calibration methods, providing a framework for selecting the optimal approach based on specific in-vivo biosensing research requirements.
Performance Comparison of Calibration Methods
The following table summarizes the core performance characteristics of different adaptive calibration strategies, based on recent experimental deployments.
Table 1: Performance Comparison of Adaptive Calibration Methods
| Calibration Method | Core Principle | Key Experimental Findings | Best-Suited Sensor Types |
|---|---|---|---|
| In-situ Baseline (b-SBS) [73] | Remote calibration by fixing sensitivity and adjusting baseline using statistical coefficients from sensor networks. | - Median R² increase of 45.8% (0.48 to 0.70) for NO₂ sensors [73]. - RMSE decrease of 52.6% (16.02 ppb to 7.59 ppb) [73]. - Baseline drift stable within ±5 ppb over 6 months [73]. | Electrochemical gas sensors (NO₂, NO, CO, O₃) [73]. |
| Trust-Based Dynamic Framework [74] | Dynamic model adjustment based on a trust score (accuracy, stability, responsiveness, consensus). | - MAE reduced by up to 68% for low-trust sensors [74]. - MAE reduced by 35-38% for reliable sensors [74]. - Outperformed Linear Regression and Random Forest in simulations [74]. | Low-cost particulate matter (PM) sensor networks [74]. |
| FRET Standardization [9] | Uses "FRET-ON" and "FRET-OFF" calibration standards in barcoded cells for signal normalization. | - Calibrated FRET ratio becomes independent of laser intensity and detector settings [9]. - Enables simultaneous determination of actual FRET efficiency [9]. - Facilitates highly multiplexed biosensor imaging [9]. | FRET-based biosensors (e.g., for kinase activity, G-protein activation) [9]. |
| Nonlinear Machine Learning [75] | Employing nonlinear models (e.g., ANN) to map sensor raw data to reference values. | - Achieved R² of 0.93 at 20-min resolution for PM₂.₅, outperforming linear models [75]. - Identified temperature, wind speed, and heavy vehicle density as key calibration factors [75]. | Low-cost PM₂.₅ sensors in urban environments [75]. |
| Self-Calibrating Ratiometric Sensors [72] | Built-in correction using a reference signal and a response signal for internal calibration. | - Corrects for signal fluctuations and matrix effects in complex samples [72]. - Provides a wider dynamic range and improved tolerance in food matrices [72]. - Enables ultra-precise trace detection [72]. | Fluorescence- and colorimetric-based biosensors for food hazards [72]. |
Detailed Experimental Protocols and Methodologies
In-situ Baseline Calibration (b-SBS) for Sensor Networks
The b-SBS method was designed for large-scale electrochemical sensor networks monitoring air quality [73]. The protocol involves a shift from traditional, labor-intensive side-by-side (SBS) calibration with reference monitors.
- Pre-deployment Phase: A batch of sensors undergoes multiple short-term (5-10 day) co-location trials with a reference-grade monitor (RGM). Hundreds of these "calibration samples" are used to analyze the distribution of sensitivity coefficients (the sensor's responsiveness to gas concentration) [73].
- Sensitivity Universalization: Analysis of over 100 sensors for each gas (NO₂, NO, CO, O₃) revealed sensitivity coefficients were clustered with a variation of less than 20%. This allows for the use of a single, universal median sensitivity value for all sensors of the same type in the network [73].
- Field Deployment and Baseline Calibration: Post-deployment, only the baseline (zero output) requires calibration. This is performed remotely using the 1st percentile method, which identifies the lowest sensor readings over a period to represent the baseline in clean air, without needing physical co-location with an RGM [73].
- Validation: Performance is validated by comparing the b-SBS calibrated data from field-deployed sensors against data from nearby RGMs, demonstrating significant improvements in R² and RMSE [73].
Trust-Based Dynamic Calibration Framework
This framework treats sensors as a democratic network, weighting their "votes" based on performance-based trust scores [74].
- Trust Score Calculation: Each sensor is assigned a dynamic trust score integrating four indicators:
- Accuracy: Proximity to a reference signal or trusted consensus.
- Stability: Minimal short-term variance in readings.
- Responsiveness: Ability to track concentration changes.
- Consensus Alignment: Agreement with neighboring sensors [74].
- Two-Stage Calibration:
- Offset-Scale Correction: Corrects large-scale systematic errors (offsets and scaling mismatches) common in all low-cost sensors.
- Adaptive Modeling: Sensors with high trust scores undergo minimal correction to preserve their inherent accuracy. Sensors with low trust scores trigger more complex calibration, leveraging expanded feature sets (e.g., wavelet-based features) and deeper machine learning models [74].
- Validation: The framework was validated through extensive simulations and real-world deployment in Zurich. It consistently reduced MAE, particularly for poorly performing sensors, and outperformed standard calibration models like Linear Regression and Random Forest [74].
FRET Biosensor Calibration via Engineered Standards
This optical method corrects for instrumentation variability in live-cell FRET imaging [9].
- Standard Preparation: Engineered calibration standards are created by locking the CFP-YFP FRET pair in constitutively "FRET-ON" (high efficiency) and "FRET-OFF" (low efficiency) conformations. These standards are expressed in subsets of cells that are barcoded for identification [9].
- Multiplexed Imaging: Barcoded cells expressing the calibration standards are mixed with cells expressing the biosensors of interest. All cells are imaged simultaneously under the same conditions [9].
- Signal Normalization: The known FRET ratios of the "FRET-ON" and "FRET-OFF" standards, measured during the session, create a calibration curve. This curve is used to normalize the FRET ratios of the experimental biosensors, compensating for variations in laser intensity and detector sensitivity [9].
- Efficiency Calculation: Including donor-only and acceptor-only cells in the experiment allows for the calculation of actual FRET efficiency, moving beyond the simpler but less accurate FRET ratio [9].
The following diagram illustrates the logical workflow of a trust-based dynamic calibration framework, integrating the key steps from data acquisition to consensus output.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Research Reagents and Materials for Adaptive Calibration
| Item | Function in Adaptive Calibration | Example Application |
|---|---|---|
| Electrochemical Sensor Node [73] | The core sensing unit for detecting gaseous analytes; requires characterization of sensitivity and baseline coefficients. | In-situ baseline calibration for environmental gas monitoring networks (NO₂, CO) [73]. |
| Reference-Grade Monitor (RGM) [73] [75] | Provides ground-truth data for initial model training and validation of sensor performance. | Co-location experiments to generate training data for linear and nonlinear calibration models [73] [75]. |
| "FRET-ON"/"FRET-OFF" Standards [9] | Genetically encoded calibration standards with known, fixed FRET efficiencies for signal normalization. | Correcting for instrumental drift and enabling cross-experiment comparison in live-cell imaging [9]. |
| Barcoding Proteins (Blue/Red FPs) [9] | Fluorescent proteins targeted to distinct subcellular locations to uniquely label cell populations. | Multiplexed imaging, allowing identification and tracking of different biosensors or standards in mixed cell cultures [9]. |
| Ratiometric Fluorescent Probe [72] | A sensing molecule that emits two distinct signals, one of which serves as an internal reference. | Self-calibrating sensors for detecting hazards in complex matrices (e.g., food, biological fluids), correcting for probe concentration and environmental effects [72]. |
The following diagram illustrates the experimental workflow for calibrating FRET biosensors using engineered standards in a barcoded, multiplexed setup.
The choice of an adaptive calibration strategy is paramount for the success of long-term in-vivo biosensing research. As the comparative data shows, the optimal method is highly dependent on the sensor technology and research context. For large-scale environmental sensor networks, in-situ baseline and trust-based methods offer scalable, data-driven solutions. In contrast, for precise molecular monitoring in live cells, FRET standardization provides the necessary rigor to overcome instrumental variance. Self-calibrating ratiometric sensors represent a powerful approach at the reagent level. By integrating these adaptive strategies, researchers can significantly enhance the reliability and longevity of their sensor deployments, ensuring the generation of high-quality, reproducible data for critical drug development and biomedical research.
Validation Frameworks and Accuracy Metrics Across Platforms
Dynamic Validation Methods for Calibration Accuracy and Structural Robustness
In the field of in-vivo biosensing research, the ability to trust sensor output is foundational to scientific discovery and clinical application. For biosensors deployed within living organisms, calibration accuracy ensures that measurements reflect true biochemical concentrations, while structural robustness guarantees that the sensor's performance withstands the complex biological environment. These two factors directly determine the reliability of data used in pharmacokinetic studies, therapeutic drug monitoring, and feedback-controlled drug delivery systems [5] [76].
Traditional single-point calibration methods often prove inadequate for in-vivo applications, where dynamic physiological conditions can alter sensor behavior. This comparison guide examines advanced dynamic validation methodologies that enable researchers to verify calibration accuracy and structural robustness under conditions mimicking real-world operation. By objectively comparing these approaches across key performance metrics, we provide a framework for selecting appropriate validation strategies tailored to specific biosensing applications, from electrochemical DNA-based sensors to whole-cell biosensing platforms [5] [77].
Comparative Analysis of Dynamic Validation Approaches
The following table summarizes the core characteristics, advantages, and limitations of prominent dynamic validation methods relevant to in-vivo biosensing research.
Table 1: Comparison of Dynamic Validation Methods for Biosensor Calibration and Robustness
| Validation Method | Key Principles | Target Biosensors | Reported Accuracy | Strengths | Limitations |
|---|---|---|---|---|---|
| V3 Framework (In Vivo Adaptation) [76] | Verification, Analytical Validation, Clinical Validation | Preclinical digital measures (e.g., biosensor data) | Establishes reliability and relevance | Holistic scope, ensures data integrity from raw data to biological interpretation, supports translational relevance | Complex implementation, requires specialized expertise, time-consuming validation process |
| Ground–Object–Air Cooperation [78] | High-precision 3D reference field with real-time pose tracking | Multi-sensor mobile platforms (e.g., Navcam, Hazcam, LiDAR) | Sub-millimeter pose tracking accuracy | Dynamic validation capability, assesses both calibration accuracy and structural robustness | Primarily designed for ex-vivo mechanical systems, limited direct biological application |
| Calibration-Standard Normalization [9] | FRET signal normalization using high and low FRET standards | Genetically encoded FRET biosensors | Enables cross-experimental and long-term studies | Compensates for imaging fluctuations and photobleaching, facilitates multiplexed imaging | Requires engineering of specific FRET standards, limited to optically interrogated biosensors |
| Kinetic Differential Measurement (KDM) [3] | Signal processing of square-wave voltammetry at multiple frequencies | Electrochemical aptamer-based (EAB) sensors | <10% error in clinical vancomycin range | Corrects for sensor drift, enhances gain for in-vivo measurements, validated in undiluted whole blood | Performance depends on careful media and temperature matching during calibration |
Detailed Experimental Protocols and Methodologies
V3 Framework for Preclinical Digital Measures
The V3 Framework, adapted from clinical digital medicine standards, provides a structured approach to validate digital measures derived from biosensors in preclinical research [76]. The methodology encompasses three distinct validation stages:
- Verification: Confirms that digital technologies accurately capture and store raw data from the biosensor without corruption or significant noise. This involves testing sensor hardware under controlled conditions to establish baseline performance metrics.
- Analytical Validation: Assesses the precision and accuracy of algorithms that transform raw sensor data into meaningful biological metrics. This stage involves comparing biosensor output against reference standards across the sensor's dynamic range.
- Clinical Validation: Confirms that the biosensor measurements accurately reflect the intended biological or functional states in animal models relevant to the specific context of use. This requires correlation with established physiological or behavioral endpoints.
Implementation of this framework requires collaboration between biosensor developers, biologists, and data scientists to establish appropriate validation protocols specific to each biosensor platform and research context.
Calibration-Standard Normalization for FRET Biosensors
This protocol enables robust calibration of FRET biosensor signals, addressing variability caused by imaging parameters, photobleaching, and environmental fluctuations [9]:
Table 2: Key Reagents for FRET Calibration Standard Experiments
| Research Reagent | Function/Description | Application in Validation |
|---|---|---|
| FRET-ON Standards | Engineered constructs with consistently high FRET efficiency | Serves as high-FRET reference for signal normalization |
| FRET-OFF Standards | Engineered constructs with consistently low FRET efficiency | Serves as low-FRET reference for signal normalization |
| Donor-Only Cells | Cells expressing only the donor fluorophore | Enables determination of crosstalk parameters |
| Acceptor-Only Cells | Cells expressing only the acceptor fluorophore | Facilitates correction for direct acceptor excitation |
| Barcoding Proteins | Blue or red FPs targeted to distinct subcellular locations | Enables multiplexed imaging of multiple biosensors |
Experimental Workflow:
- Prepare cell cultures expressing FRET-ON standards, FRET-OFF standards, and experimental biosensors in separate vessels.
- Use barcoding proteins with spectra separable from the biosensors to label cells expressing different standards and biosensors.
- Mix barcoded cells for simultaneous imaging in the experimental setup.
- Acquire fluorescence signals from donor and acceptor channels under standardized imaging conditions.
- Calculate normalized FRET ratios using the signals from FRET-ON and FRET-OFF standards to compensate for variability in imaging conditions.
- Apply calibrated FRET ratios to determine actual FRET efficiency for experimental biosensors.
This method has demonstrated effectiveness in restoring reciprocal donor and acceptor signal trends often obscured by imaging drifts, providing essential validation for observed biosensor responses in long-term studies [9].
Media-Matched Calibration for Electrochemical Aptamer-Based Sensors
For EAB sensors deployed in complex biological environments, calibration in media that closely matches the measurement environment is critical for accuracy [3]:
Protocol for Whole Blood Calibration:
- Collect fresh whole blood (rat or bovine) less than 24 hours before calibration.
- Maintain blood at body temperature (37°C) throughout calibration and measurement procedures.
- Divide blood samples and spike with known concentrations of target analyte (e.g., vancomycin) covering the expected dynamic range.
- Interrogate EAB sensors using square wave voltammetry at multiple frequencies (e.g., 25 Hz and 300 Hz) for each concentration.
- Convert voltammogram peak currents to Kinetic Differential Measurement (KDM) values using the formula: KDM = (Normalized signal at signal-off frequency - Normalized signal at signal-on frequency) / Average of both signals.
- Fit KDM values to a Hill-Langmuir isotherm to generate a calibration curve with parameters KDMmin, KDMmax, K1/2, and nH (Hill coefficient).
- Apply these parameters to convert subsequent in-vivo measurements to concentration estimates using the derived equation.
This methodology demonstrated accuracy better than ±10% for vancomycin measurement across the clinical range (6-42 µM) when calibration and measurement were performed under matched conditions (fresh whole blood at body temperature) [3].
Conceptual Framework for Dynamic Validation
The diagram below illustrates the logical relationships and workflow between different components of a comprehensive dynamic validation strategy for in-vivo biosensors.
Performance Metrics and Experimental Data
Impact of Calibration Conditions on Sensor Accuracy
Experimental data reveals how calibration conditions significantly impact measurement accuracy for in-vivo biosensors:
Table 3: Effect of Calibration Conditions on EAB Sensor Performance [3]
| Calibration Condition | Temperature | Blood Age | Measurement Error | Key Observations |
|---|---|---|---|---|
| Matched Conditions | 37°C | <24 hours | <10% across clinical range | Optimal accuracy achieved when calibration matches measurement environment |
| Temperature Mismatch | 25°C (cal) vs 37°C (measure) | <24 hours | Up to 40% underestimation | Signal gain and binding curve midpoint affected by temperature |
| Blood Age Discrepancy | 37°C | 1 day vs 14 days | Significant at extremes | Older blood shows reduced signal gain at high concentrations |
| Species Variation | 37°C | <24 hours | Moderate differences | Rat vs bovine blood shows variations in signal response |
Triple-Mode Biosensing for Enhanced Reliability
Emerging triple-mode biosensing platforms address validation challenges through self-correcting measurement architectures [67]:
Implementation Methodology:
- Design biosensing platforms that integrate three distinct detection mechanisms (e.g., colorimetric, fluorescent, and electrochemical).
- Engineer multifunctional nanomaterials that enable simultaneous signal generation across multiple modalities.
- Collect measurements from all three detection systems in parallel.
- Apply cross-validation algorithms to identify and correct anomalies in individual measurement channels.
- Generate consensus measurements incorporating data from all three modalities for improved accuracy and reliability.
These systems demonstrate particular utility in complex matrices where single-mode biosensors suffer from interference issues, with reported improvements in accuracy and reliability compared to single-mode approaches [67].
Dynamic validation of calibration accuracy and structural robustness represents a critical frontier in advancing in-vivo biosensing capabilities. The methodologies examined herein—from the comprehensive V3 Framework to application-specific approaches like calibration-standard normalization and media-matched calibration—provide researchers with powerful tools to verify biosensor performance under physiologically relevant conditions.
Experimental data consistently demonstrates that matching calibration conditions to measurement environments reduces errors by up to 30% in some systems, while structured validation frameworks significantly enhance the reliability of biosensor data in preclinical research [76] [3]. As biosensor technologies continue to evolve toward greater complexity and integration with artificial intelligence, robust dynamic validation methodologies will play an increasingly essential role in ensuring that these innovative tools deliver accurate, actionable data for biomedical research and clinical applications.
The choice of validation strategy should be guided by specific biosensor technology, intended application, and required precision, with multi-modal approaches generally offering superior reliability for critical applications where measurement accuracy directly impacts research conclusions or clinical decisions.
In the field of in-vivo biosensing research, establishing robust performance benchmarks is paramount for translating laboratory innovations into clinically reliable tools. Clinical accuracy, often defined as measurement deviation within ±20% of a reference standard, alongside precision, which quantifies measurement reproducibility, forms the critical foundation for evaluating biosensor efficacy. These benchmarks are not merely academic exercises; they are essential for ensuring that biosensors provide trustworthy data for therapeutic drug monitoring, disease diagnosis, and personalized medicine. The transition from a proof-of-concept biosensor to a clinically admissible device hinges on its ability to consistently meet these stringent performance criteria under real-world conditions, including complex matrices like serum, saliva, or interstitial fluid [2] [5].
The challenge lies in the multifaceted nature of performance validation. A biosensor must demonstrate not only high sensitivity and selectivity but also operational robustness against nonspecific binding, environmental fluctuations, and biofouling. Furthermore, the chosen calibration method profoundly influences the ultimate accuracy and precision of the device. This guide objectively compares the performance of various biosensor calibration and operational approaches, providing researchers with a framework for benchmarking their systems against emerging standards in the field [79] [80].
Quantitative Performance Data Comparison
The table below summarizes key performance metrics for different types of biosensors, as reported in recent literature. These metrics provide a benchmark for comparing the clinical accuracy and precision of various sensing strategies.
Table 1: Performance Benchmarks for Various Biosensor Types
| Biosensor Type / Target | Accuracy / Sensitivity | Precision / Dynamic Range | Key Performance Highlights | Reference & Context |
|---|---|---|---|---|
| SERS-based Immunosensor (α-Fetoprotein) [81] | Limit of Detection (LOD): 16.73 ng/mL | Detection range: 0 - 500 ng/mL | Liquid-phase SERS platform using Au-Ag nanostars; detects intrinsic vibrational modes of the biomarker. | Biosensors 2025 |
| Electrochemical DNA (eDNA) Sensor [5] | High versatility for real-time in vivo monitoring | Reversible and continuous operation | Enables therapeutic drug monitoring (TDM) and pharmacokinetic studies; focuses on calibration-free strategies. | Review Article 2025 |
| Photonic Microring Resonator (IL-17A) [79] | Accuracy validated via reference subtraction | Performance depends on optimal control probe (e.g., BSA scored 83%) | Label-free optical biosensor; systematic study on negative control probes to minimize nonspecific binding error. | Analytical Chemistry 2025 |
| Wearable Heart Rate Monitor [80] | Target Mean Absolute Error (MAE): ≤5 bpm | N/A | Investor-expected benchmark for clinical validation versus clinical-grade ECG. | Clinical Validation Guide |
| Whole-Cell Biosensor (Cobalt) [82] | Highly sensitive detection in complex food matrices | N/A | Engineered bacterial cells with fluorescence signal; detects low cobalt concentrations in bran and fine bran. | Biosensors 2025 |
| THz SPR Biosensor [81] | Phase Sensitivity: 3.1x10^5 deg/RIU (liquid) | N/A | Theoretical sensor with graphene-integrated Otto configuration; tunable via external magnetic field. | Biosensors 2025 |
Detailed Experimental Protocols for Benchmarking
To ensure that performance benchmarks are met, rigorous and standardized experimental protocols must be followed. These methodologies are critical for generating comparable and reliable data across different biosensor platforms.
Protocol for Label-Free Biosensor Validation with Reference Controls
This protocol, detailed in studies on photonic microring resonators, is essential for achieving high accuracy by accounting for nonspecific binding (NSB) [79].
- Step 1: Sensor Functionalization: Immobilize the specific capture probe (e.g., anti-IL-17A monoclonal antibody) on the active sensor surface. In parallel, functionalize a reference channel on the same chip with a carefully selected negative control protein.
- Step 2: Control Probe Selection: The choice of control is critical. Isotype-matched antibodies (e.g., mouse IgG1 for a mouse IgG1 capture antibody) are common, but systematic optimization is required. Alternatives include Bovine Serum Albumin (BSA), anti-FITC, or other non-interacting proteins to identify the probe that best corrects for NSB without over- or under-subtracting the signal.
- Step 3: Assay Execution and Data Acquisition: Introduce the sample (in buffer or a complex medium like serum) to both the active and reference sensors simultaneously under continuous flow. Record the binding response in real-time from both channels.
- Step 4: Reference Subtraction: The specific binding signal is obtained by subtracting the response of the reference channel from that of the active capture channel. This corrected signal is then used for all subsequent quantitative analysis and calibration curve generation.
Protocol for Staged Clinical Validation
For biosensors intended for clinical use, a multi-stage validation ladder is recommended by investors and regulatory bodies to de-risk the technology [80]. The workflow for this staged clinical validation is systematized as follows:
Figure 1: The clinical validation ladder for biosensors, outlining the staged process from initial lab tests to real-world deployment.
- Stage 1: Analytical Validation (Bench): This initial phase determines fundamental parameters including the Limit of Detection (LOD), linearity, signal drift, and repeatability under ideal, controlled laboratory conditions. This stage typically spans 2-8 weeks and uses spiked samples in buffer solutions [80].
- Stage 2: Technical/Engineering Verification: The biosensor hardware and software undergo stress tests, including electromagnetic interference (EMI/EMC) safety checks (per IEC 60601), battery life testing, and thermal stability assessment. This often requires third-party test houses [80].
- Stage 3: Controlled Clinical Accuracy: The biosensor is tested against the appropriate gold standard (e.g., 12-lead ECG for arrhythmia, clinical-grade pulse oximeter for SpO₂) using samples collected under ideal clinical conditions. This retrospective or case-control study provides initial estimates of sensitivity and specificity [80].
- Stage 4: Prospective Clinical Validation: This is a pivotal study where the biosensor is tested on a large, prospectively enrolled cohort from the intended use population. Pre-specified primary endpoints (e.g., sensitivity for atrial fibrillation, Mean Absolute Error for heart rate) are measured under real-world conditions, including motion, variable skin tones, and environmental factors [80].
- Stage 5: Real-World Performance & Utility: The final stage assesses the impact of the biosensor on clinical decision-making, health outcomes, and economics. Studies in this phase look at adoption rates, reduction in hospital readmissions, and patient adherence in community or home settings [80].
Protocol for In Vivo Sensor Calibration
For continuous in vivo monitors, such as continuous glucose monitors (CGMs), calibration is a dynamic process. Modern protocols move beyond simple one-point calibration to improve accuracy and user experience [56].
- Step 1: Reference Measurement and Pairing: Obtain a reference analyte value (e.g., from a fingerstick blood glucose meter) at a specific calibration time. This value is paired with the corresponding sensor signal from the in vivo biosensor.
- Step 2: Sensitivity Adjustment and System Checks: The system's sensitivity is adjusted based on the difference between the reference value and the sensor signal. Advanced methods use an "adjustment map" that balances the risk of over- and under-calibration using a priori information. The system defers calibration if signal anomalies, such as early signal attenuation (ESA) or dropouts, are detected, as these can lead to inaccurate calibration [56].
- Step 3: Calibration Refinement: Some methods involve an update step, where the initial calibration is refined using the same reference measurement but paired with a longer duration of sensor data collected before and after the calibration time. This helps to stabilize the calibration factor [56].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table lists essential materials and reagents commonly used in the development and validation of high-performance biosensors, along with their critical functions.
Table 2: Essential Research Reagents for Biosensor Development and Validation
| Reagent / Material | Function in Biosensing | Application Context |
|---|---|---|
| Capture Antibodies (e.g., anti-IL-17A, anti-CRP) [79] | The primary biorecognition element that selectively binds the target analyte. | Immobilized on the sensor surface to provide specificity in immunosensors. |
| Isotype-Matched Control Antibodies [79] | Serves as a negative control on a reference channel to measure and subtract nonspecific binding (NSB) signals. | Critical for improving accuracy in label-free optical and electrochemical biosensors. |
| Bovine Serum Albumin (BSA) [79] | A common blocking agent and potential negative control protein to reduce NSB by occupying non-specific sites. | Used in surface passivation and as a benchmark for reference channel optimization. |
| Gold Nanoparticles & Nanostars [81] [83] | Plasmonic nanomaterials that enhance signal transduction, particularly in optical (SERS, SPR) and electrochemical biosensors. | Used to increase sensitivity and lower the limit of detection. |
| Functionalized Electrodes (Graphene, CNTs, Polyaniline) [83] | Nanomaterial-modified electrodes that provide a large surface area and excellent electron transfer capabilities. | Form the base of electrochemical biosensors for enhanced signal-to-noise ratio. |
| CRISPR-Based Platforms [84] [83] | Provides highly specific and programmable nucleic acid detection capabilities. | Used for detecting DNA/RNA targets, such as viral pathogens or specific genetic mutations. |
| DNA Aptamers [5] [83] | Synthetic, single-stranded DNA molecules that bind to specific targets (ions, molecules, proteins) with high affinity. | Serve as synthetic bioreceptors in place of antibodies for a wider range of targets. |
The establishment and adherence to rigorous performance benchmarks, specifically the ±20% clinical accuracy standard and high-precision metrics, are non-negotiable for the advancement of reliable in-vivo biosensing research. As demonstrated, achieving these benchmarks requires a multi-faceted approach: integrating advanced materials like nanomaterials and CRISPR systems, employing rigorous experimental protocols with appropriate controls, and following a staged clinical validation pathway. The choice of calibration method—from sophisticated in vivo reference subtraction to staged clinical trials—directly dictates the real-world accuracy and clinical utility of the biosensor. For researchers, the continuous refinement of these protocols and the diligent application of these benchmarks are the cornerstones of developing biosensors that not only generate compelling data in the lab but also earn the trust of clinicians and patients in the real world.
The ability to perform real-time, in-vivo molecular monitoring is revolutionizing our understanding of dynamic biological processes, from metabolite flux in single cells to drug pharmacokinetics in living animals. For researchers, scientists, and drug development professionals, selecting the appropriate biosensing technology is paramount for experimental success. This guide provides an objective, data-driven comparison between two leading platforms: electrochemical aptamer-based (EAB) biosensors and genetically encoded biosensors (GEBs). Framed within the critical context of calibration accuracy for in-vivo research, we dissect their operational principles, performance metrics, and the experimental protocols that underpin their application in complex biological environments.
The fundamental distinction between these platforms lies in their construction and the physical basis of their signal transduction.
- Electrochemical Aptamer-Based (EAB) Biosensors are engineered, surface-immobilized devices. They consist of an electrode-modified aptamer (a single-stranded DNA or RNA molecule) tagged with a redox reporter (e.g., methylene blue). Target binding induces a conformational change in the aptamer, which alters the electron transfer efficiency between the reporter and the electrode surface. This change is measured electrochemically as a current or impedance shift [85] [86].
- Genetically Encoded Biosensors (GEBs) are biomolecular tools constructed by fusing a sensing protein domain (e.g., a ligand-binding protein or transcription factor) to a fluorescent protein pair (e.g., cpYFP). Binding of the target metabolite causes a conformational shift in the sensor, modulating the Förster Resonance Energy Transfer (FRET) between the fluorescent proteins. The resulting change in fluorescence emission ratio is measured optically [87] [88].
The signaling pathways for these two technologies are illustrated below.
EAB Sensor Signaling Pathway
Genetically Encoded Biosensor Signaling Pathway
Performance Metrics and Quantitative Comparison
The choice between EAB sensors and GEBs is guided by their performance across key metrics, as summarized in the table below. The data is compiled from recent experimental studies (2020-2025).
Table 1: Comparative Performance Metrics for In-Vivo Biosensing
| Performance Metric | Electrochemical Aptamer-Based (EAB) Biosensors | Genetically Encoded Biosensors (GEBs) |
|---|---|---|
| Temporal Resolution | Seconds to sub-second [86] | Seconds to minutes [87] |
| Measurement Duration | Hours (typically 4-12 hours) [86] | Potentially days to weeks (limited by cell viability/expression) [88] |
| Spatial Resolution | Tissue or body fluid level (e.g., vein, interstitial fluid) [86] | Subcellular to cellular level [87] [88] |
| Limit of Detection (LoD) | Vancomycin: ~µM range in blood [3]HSA Aptamer Sensor: 124 fg/mL in PBS [89] | d-2-HG Sensor (DHOR): Demonstrated in vivo, specific values not quantified [87] |
| Key Strengths | • Real-time, in-vivo monitoring in bodily fluids• High specificity in complex media• Generalizable to many targets (drugs, metabolites, toxins) [85] [86] | • Subcellular resolution in living cells• Non-invasive, long-term monitoring within expressing cells• No need for external probe implantation [87] [88] |
| Major Limitations | • Limited operational duration in vivo due to biofouling/signal drift• Difficulty in obtaining high-performance aptamers for some targets [85] [86] | • Calibration is confounded by cellular metabolism and volume [90]• Requires genetic modification of the target system [88] |
Experimental Protocols for In-Vivo Calibration
Accurate calibration is the cornerstone of reliable quantitative biosensing. The protocols for EAB sensors and GEBs differ significantly, reflecting their distinct operational environments.
EAB Sensor Calibration Protocol
The following workflow, derived from established methodologies, ensures high accuracy for in-vivo EAB measurements [3].
Key Steps:
- Matrix Matching: Calibration curves are generated by titrating the target analyte into freshly collected, undiluted whole blood.
- Temperature Control: All titrations are performed at body temperature (37°C) to match in-vivo conditions, as temperature significantly impacts binding affinity and electron transfer kinetics [3].
- Signal Processing: Square wave voltammetry (SWV) is performed at two frequencies ("signal-on" and "signal-off"). The signals are converted into a Kinetic Differential Measurement (KDM) value, which corrects for signal drift and enhances gain [3].
- Curve Fitting: KDM values across target concentrations are fitted to a Hill-Langmuir isotherm to generate the calibration curve. The fitted parameters (KDMmax, KDMmin, K1/2, nH) are used to convert in-vivo sensor output into concentration values [3].
GEB Calibration Protocol
Calibrating GEBs inside living cells presents unique challenges, as infusion of metabolites can be confounded by endogenous cellular metabolism [90].
Key Steps and Pitfalls:
- Common Approach: A typical in-vivo calibration involves infusing a substrate (e.g., pyruvate) to deplete intracellular lactate, followed by infusion of a high dose of lactate to saturate the sensor (e.g., the Laconic sensor) [90].
- Critical Limitations: This method's validity is questioned because it fails to account for:
- Rapid metabolite interconversion (e.g., lactate-pyruvate) in blood and tissues.
- Preferential cellular oxidation of the infused metabolites.
- On-going glycolytic metabolism during the calibration procedure.
- Uncertainties in cellular volume [90].
- Recommendation: Thorough characterization of the sensor in the specific experimental system (e.g., plant, animal cell type) is required. Calibration data must be interpreted with caution, acknowledging potential inaccuracies from metabolic activity [90] [88].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of these biosensing technologies requires a specific set of reagents and materials.
Table 2: Key Research Reagent Solutions for Biosensor Development and Application
| Category | Item | Function in Experiment |
|---|---|---|
| EAB Sensors [3] [89] [86] | Gold Electrode / Screen-Printed Carbon Electrode | Solid support for aptamer immobilization via thiol-gold chemistry. |
| Methylene Blue | Redox reporter molecule; electron transfer efficiency is modulated by aptamer conformation. | |
| 6-Mercapto-1-hexanol (MCH) | Backfilling molecule to form a stable self-assembled monolayer, reducing non-specific adsorption. | |
| Prussian Blue (PB) | An alternative redox-active material used as an intrinsic signal generation layer, eliminating the need for terminal reporter tags [89]. | |
| GEBs [87] | Circularly Permuted Fluorescent Protein (cpYFP) | The sensing element whose fluorescence properties change upon metabolite binding. |
| Sensing Moieties (e.g., HgcR, Laconic) | The protein domain that specifically binds the target metabolite (e.g., d-2-HG, lactate). | |
| Viral Vectors / Transfection Reagents | For delivering the genetic code of the biosensor into the target cells or organisms. | |
| General [3] [90] | Fresh Whole Blood | Critical calibration matrix for EAB sensors to mimic in-vivo conditions accurately. |
| Pyruvate / Lactate Solutions | Metabolites used for in-vivo calibration attempts of metabolite GEBs (e.g., Laconic). |
This analysis reveals that EAB biosensors and GEBs are not competing technologies but are complementary tools designed for different experimental niches.
- Electrochemical Aptamer-Based (EAB) Biosensors excel at providing real-time, quantitative pharmacokinetic and metabolic data in the bloodstream and tissues of live animals. Their primary advantage is the ability to generate accurate concentration readings in complex, whole-body environments, provided calibration is performed with meticulous attention to media, temperature, and signal processing [3] [86]. The main challenge is extending their functional lifetime beyond several hours.
- Genetically Encoded Biosensors (GEBs) are unparalleled for mapping metabolic dynamics with high spatial resolution inside living cells. They are the tool of choice for studying subcellular compartmentalization, cell-type-specific metabolism, and long-term metabolic fluxes [87] [88]. However, their quantitative accuracy is currently limited by formidable calibration challenges, as cellular metabolism actively confounds the calibration process [90].
For researchers framing their work within a thesis on in-vivo biosensing accuracy, the calibration methodology is paramount. EAB sensors offer a more straightforward and validated path to absolute concentration measurements in bodily fluids. In contrast, while GEBs provide unparalleled insights into relative concentration changes in real-time within cells, translating their signals into precise absolute concentrations remains an active and critical area of methodological research. The choice ultimately depends on the biological question: for quantifying drug levels in plasma, EAB sensors are superior; for visualizing lactate gradients between astrocytes and neurons, GEBs are indispensable.
The evaluation of biosensor performance extends beyond simple statistical agreement to assess the clinical impact of measurement inaccuracies. Within the context of in-vivo biosensing research, calibration methods are not merely technical procedures but are critical determinants of whether a sensor can be safely used to guide therapeutic decisions. The Clarke Error Grid Analysis (EGA) has served as a foundational tool for this purpose since its development in 1987, providing a standardized methodology for quantifying the clinical accuracy of blood glucose meters by comparing their readings to a reference method [91]. This review objectively compares the Clarke EGA with subsequent validation techniques and frameworks, detailing their application in the evaluation of calibration methods for modern biosensors, including continuous glucose monitors (CGMs) and emerging electrochemical and non-invasive platforms.
The core principle of the Clarke Error Grid is to categorize the discrepancies between a test device and a reference method into zones that signify different levels of clinical risk. A Cartesian diagram is generated where the reference values are plotted on the x-axis and the test device values on the y-axis [92] [91]. The grid is then divided into five zones:
- Zone A: Represents values that deviate from the reference by no more than 20%, or are in the hypoglycemic range when the reference is also hypoglycemic. Points in Zone A are considered clinically accurate and would lead to correct treatment decisions [91].
- Zone B: Contains values that deviate by more than 20%, but where the treatment decisions would not be inappropriate or cause significant clinical risk [91].
- Zone C: Encompasses values that would lead to unnecessary corrective treatment (e.g., administering insulin for a normal glucose level) [91].
- Zone D: Represents dangerous failures to detect, where the test device fails to identify a clinically significant hypoglycemic or hyperglycemic event [91].
- Zone E: Contains the most critical errors, where the test device mistakes hypoglycemia for hyperglycemia or vice versa, potentially leading to catastrophic treatment errors [91].
The international standard ISO 15197:2013, which governs the performance of glucose monitoring systems, mandates that 99% of the measured values fall within the clinically acceptable Zones A and B of a Clarke Error Grid [93]. This benchmark has been widely adopted for validating the clinical utility of glucose sensors.
Evolution of Error Grid Analysis: From Clarke to DTS
While the Clarke Error Grid remains a gold standard, the field of diabetes technology has evolved, leading to the development of updated frameworks. The recent introduction of the Diabetes Technology Society (DTS) Error Grid aims to address the needs of modern devices, including both glucose meters and continuous glucose monitors (CGMs) [94]. A critical distinction of the DTS grid is that its zone boundaries were established based on a survey of 89 clinicians, incorporating contemporary treatment practices and knowledge [94].
A significant validation study using real-world adverse event data has raised important questions about established standards. This research analyzed the U.S. FDA's MAUDE database, which contains reports of device malfunctions, injuries, and deaths. By extracting instances where CGM users reported inaccuracies, the study found that Zone B of the error grid contained the highest percentage of adverse events, including complaints and injuries requiring medical intervention [94]. This finding challenges the ISO 15197:2013 requirement that 99% of results reside in Zones A and B, suggesting that a high concentration of results in Zone B may not be as clinically benign as previously assumed and that this may represent a "low bar" for regulatory requirements [94]. This evidence indicates that the clinical accuracy standards for glucose monitors are a subject of ongoing refinement and debate within the scientific community.
Table 1: Comparison of Error Grid Analysis Frameworks
| Feature | Clarke Error Grid (EGA) | Diabetes Technology Society (DTS) Error Grid |
|---|---|---|
| Year Introduced | 1987 [91] | 2024 [94] |
| Primary Application | Blood Glucose Meters | Glucose Meters and Continuous Glucose Monitors (CGMs) [94] |
| Basis of Zones | Clinical significance of errors for 1980s treatment practices | Survey of 89 clinicians on contemporary treatment practices [94] |
| Key Insight | Established the paradigm of clinical risk zoning; ISO 15197 requires 99% in Zones A+B [93] | Validation with real-world adverse event data shows complaints and injuries can occur in Zone B [94] |
Statistical Validation Techniques in Sensor Performance Evaluation
Beyond error grid analysis, a suite of statistical methods is essential for a comprehensive evaluation of biosensor performance and calibration efficacy. These techniques provide complementary insights into a sensor's accuracy, precision, and agreement with reference methods.
Bland-Altman Analysis, also known as the difference plot, is a robust method for assessing system accuracy with minimal statistical assumptions [93]. In this analysis, the difference between the test method and the reference method is plotted on the y-axis against the average of the two methods on the x-axis. This graph visually reveals the degree of agreement between the two methods, the presence of any systematic bias (e.g., consistent over- or under-estimation), and whether the bias changes across the measurement range [93].
The Mean Absolute Relative Difference (MARD) is another widely used metric, particularly for continuous glucose monitors. It calculates the average of the absolute values of the relative differences between the sensor readings and the reference values. For example, a non-invasive glucose monitoring device based on mid-infrared spectroscopy recently reported MARD values of 20.7% and 19.6% in a clinical test, which was noted as being equivalent to the performance of early CGM systems cleared by the FDA for adjunctive use [95]. However, experts caution that MARD alone is insufficient for a complete performance assessment and should be interpreted alongside clinical accuracy tools like error grids [94] [95].
The following diagram illustrates the logical relationship and application workflow of these primary statistical validation techniques in a typical biosensor evaluation pipeline.
Validation Techniques Workflow
Experimental Protocols for Calibration Assessment
Robust experimental design is paramount for generating reliable data on calibration method performance. The following protocols, drawn from recent literature, detail key methodologies for assessing both traditional and novel calibration approaches.
Protocol for Glucometer Quality Assurance per ISO 15197
A year-long study of 73 hospital glucometers provides a validated protocol for performance evaluation, aligning with ISO 15197:2013 guidelines [93].
- Internal Quality Control (IQC): Two levels of control solution (low and high) were run once per month on each glucometer. Devices producing values outside the manufacturer's specified range were flagged as outliers. The mean, standard deviation (SD), and coefficient of variation (CV%) of the IQC results were calculated over the study period to monitor precision [93].
- Proficiency Testing (PT): Every three months, a patient's venous blood sample was collected in a Sodium Fluoride-Potassium Oxalate vial. This sample was first analyzed using the laboratory reference method (a hexokinase-based assay on a Cobas C-6000 analyzer), with its accuracy verified by external quality assessment schemes. The same sample was then measured by every glucometer in the study, enabling a direct comparison of each glucometer to the reference method and an inter-instrument comparison [93].
- Statistical and Clinical Analysis: For PT, z-scores and percent variation from the reference value were calculated for each glucometer. The data were then plotted on both a Bland-Altman graph and a Clarke Error Grid to evaluate both statistical agreement and clinical significance [93].
Protocol for In-Vivo Calibration of Electrochemical Aptamer-Based Sensors
Research on Electrochemical Aptamer-Based (EAB) sensors for in-vivo drug monitoring (e.g., vancomycin) highlights the critical importance of calibration conditions [3].
- Calibration Media and Temperature: Sensors are calibrated by generating a dose-response curve (from zero to saturating target concentrations) in a specific media. Studies show that matching the temperature of the calibration media to the in-vivo measurement temperature (37°C) is crucial. Calibration curves collected at room temperature can differ significantly from those at body temperature, leading to substantial underestimation or overestimation of target concentrations in vivo [3].
- Media Freshness and Composition: For measurements in blood, calibrating in freshly collected, undiluted whole blood is superior to using aged, commercially sourced blood. Blood age can impact the sensor's signal gain, potentially leading to concentration overestimates [3]. The calibration curve is typically fitted to a Hill-Langmuir isotherm to derive parameters like KDM~max~, KDM~min~, K~1/2~, and the Hill coefficient (n~H~), which are then used to convert sensor signal into concentration estimates [3].
Protocol for Calibration-Free Sensor Operation
A "dual-frequency" method has been demonstrated for EAB sensors to achieve calibration-free operation while maintaining clinically relevant (±20%) accuracy [33]. This approach exploits the square-wave frequency dependence of EAB sensor signaling.
- Identification of Frequencies: A "responsive" square-wave frequency (e.g., 500 Hz) is identified where the sensor's peak current changes significantly upon target binding. A "non-responsive" frequency (e.g., 40 Hz) is also identified where the peak current remains constant regardless of target concentration [33].
- Ratiometric Signal Generation: The sensor is interrogated simultaneously at both the responsive (i) and non-responsive (i~NR~) frequencies. The current at the non-responsive frequency is proportional to the baseline current (i~min~). A ratiometric signal (i / i~NR~) is calculated, which is largely insensitive to sensor-to-sensor fabrication variations and drift [33].
- Concentration Estimation: Using pre-determined constants (α, γ, K~D~) obtained from a one-time characterization of the sensor design, the target concentration can be estimated directly from the ratiometric signal without the need for individual sensor calibration [33].
Table 2: Summary of Key Experimental Findings from Cited Studies
| Study Focus | Calibration Method | Key Performance Outcome | Reference Standard Used |
|---|---|---|---|
| Hospital Glucometers (73 devices) [93] | Monthly IQC; Quarterly PT vs. hexokinase lab method | 96.83% of values in Clarke Zone A; 3.17% in Zone B; 8 faulty devices identified and replaced | ISO 15197:2013; Clarke EGA |
| EAB Sensor for Vancomycin [3] | Calibration in fresh, 37°C whole blood | Accuracy better than ±10% over clinical range (6-42 µM) | Comparison to spiked known concentrations |
| Calibration-Free EAB Sensor [33] | Dual-frequency ratiometric method | Accuracy within ±20% over a 100-fold concentration range in serum | Comparison to spiked known concentrations |
| Non-Invasive Glucose Monitor [95] | Mid-infrared spectroscopy with algorithm calibration | MARD of 19.6-20.7% (comparable to early FDA-cleared CGM) | Comparison to reference blood glucose |
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and materials essential for conducting the experiments and validation procedures described in this guide.
Table 3: Research Reagent Solutions and Essential Materials
| Item Name | Function / Application | Specific Example / Note |
|---|---|---|
| Control Solutions (Low & High) | For Internal Quality Control (IQC) to verify glucometer precision and detect drift [93]. | e.g., Manufacturer-provided solutions with specified ranges (e.g., Low: 41-71 mg/dL, High: 208-282 mg/dL) [93]. |
| Sodium Fluoride/Potassium Oxalate Vials | Anticoagulant and glycolysis inhibitor for collecting venous blood samples for reference analysis [93]. | Preserves glucose concentration by inhibiting enolase, preventing glycolysis in drawn blood samples [93]. |
| Reference Method Enzymatic Assay | Gold-standard laboratory method for determining "true" glucose concentration for proficiency testing [93]. | Hexokinase method performed on a fully automated clinical chemistry analyzer (e.g., Cobas C-6000) [93]. |
| Fresh Whole Blood | Ideal calibration matrix for in-vivo biosensor calibration to mimic the actual measurement environment [3]. | Should be freshly collected and used at body temperature (37°C) for accurate calibration of sensors like EAB types [3]. |
| Electrochemical Aptamer-Based Sensor | Platform for continuous, real-time molecular monitoring in undiluted bodily fluids [5] [3]. | Comprises a redox-reporter-modified aptamer immobilized on a gold electrode; signal changes upon target binding [33]. |
| Non-Invasive Sensing Platform | Technology for painless glucose measurement without skin penetration [95]. | e.g., Quantum cascade laser exciting glucose molecules in the mid-infrared (8-12 µm) range, with photothermal detection [95]. |
The rigorous validation of calibration methods is a cornerstone of reliable in-vivo biosensing. The Clarke Error Grid remains an indispensable tool for assessing the clinical consequences of measurement inaccuracies, with its Zones A and B serving as a benchmark in international standards like ISO 15197:2013 [93]. However, evidence from real-world adverse events indicates that the clinical acceptance of these zones is still being refined [94]. A comprehensive evaluation requires a multi-faceted approach, integrating traditional statistical tools like Bland-Altman analysis and MARD with clinical error grids. As the field advances, the development of sophisticated calibration protocols that meticulously control for temperature and media composition [3], and the emergence of innovative calibration-free sensing strategies [33], are pushing the boundaries toward more accurate, reliable, and user-friendly biosensors for both research and clinical application.
Cross-Platform Accuracy Assessment in Complex Biological Matrices
Accurately quantifying analyte concentrations within complex biological matrices (e.g., blood, serum, tissue) represents a significant challenge in biosensing research and drug development. These matrices introduce substantial and variable background interference, often referred to as the "matrix effect," which can alter sensor responsiveness, cause signal suppression or enhancement, and lead to inaccurate readings. Matrix effects arise from numerous factors including proteins, lipids, salts, metabolic byproducts, and variable pH, all of which can interfere with the biorecognition event or the physicochemical transduction mechanism. For biosensors deployed in vivo or used with complex biological samples ex vivo, these effects are compounded by dynamic physiological changes and the presence of confounding non-target molecules. Consequently, a sensor calibrated in simple buffer solutions often demonstrates markedly different performance—including shifted sensitivity, altered linear dynamic range, and reduced selectivity—when applied to real-world biological samples. Robust calibration strategies are therefore not merely a procedural step but a critical determinant of analytical validity, especially for applications in therapeutic drug monitoring, personalized medicine, and pharmacokinetic studies where clinical decision-making depends on reliable data.
This guide provides a systematic comparison of established and emerging calibration methodologies designed to overcome matrix-induced inaccuracies. We objectively evaluate their performance based on experimental data, focusing on their operational principles, key performance metrics, and suitability for different research and clinical applications.
Comparative Analysis of Calibration Methodologies
The following table summarizes the core characteristics and performance data of the primary calibration approaches used to ensure accuracy in complex biological matrices.
Table 1: Comparison of Calibration Methods for Biosensing in Complex Matrices
| Calibration Method | Key Principle | Reported Performance Metrics | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Standard Addition | Analyte standard is added directly to the sample matrix; eliminates need for matched calibrators by accounting for signal modulation from the matrix [59] | Improved accuracy in complex samples; Reduces matrix-effect error [59] | Directly compensates for matrix effects in the specific sample; No need for an artificial matrix [59] | Sample-consuming; Increases preparation time and complexity; Not suitable for real-time, in vivo monitoring |
| Reference Standardization (FRET) | Uses internal calibration standards (e.g., "FRET-ON"/"FRET-OFF" cells) for signal normalization, making the output independent of imaging parameters [9] | Calibrated FRET ratio is independent of imaging settings; Enables determination of actual FRET efficiency [9] | Corrects for instrumental fluctuations and photobleaching; Facilitates multiplexed imaging and cross-experiment comparisons [9] | Requires genetic engineering of standards; Increases experimental setup complexity; Primarily for imaging applications |
| Machine Learning (ML) & Transfer Learning | Algorithms learn complex, non-linear relationships between sensor output and analyte concentration, compensating for drift, noise, and interference [96] [59] [61] | RMSE of 0.143-0.1465 for signal prediction [59]; 99.3% reduction in calibration samples needed for gas sensors [61] | Can handle large, noisy datasets; Capable of real-time signal correction; Reduces need for frequent recalibration [96] [61] | Requires large, high-quality training datasets; "Black box" nature can reduce interpretability; Computational resource demands |
| Direct Standardization (DS) / Piecewise Direct Standardization (PDS) | Mathematical transformation of signals from a new sensor to match those of a primary, fully calibrated sensor [61] | Enables calibration transfer between sensors; PDS showed lower RMSE than DS in some applications [61] | Mitigates manufacturing tolerances and unit-to-unit sensor variability; Reduces calibration burden for new sensors [61] | Requires a set of transfer samples measured on both sensors; Performance depends on the similarity between sensor responses |
Detailed Experimental Protocols and Data
Protocol 1: FRET Biosensor Calibration Using Reference Standards
This protocol, adapted from studies on robust calibration of FRET biosensors, is designed to produce quantitative measurements independent of microscope setup or laser intensity fluctuations [9].
Objective: To obtain accurate, calibrated FRET efficiency measurements in live cells, corrected for variations in imaging conditions.
Materials:
- Genetically encoded FRET biosensor of interest
- "FRET-ON" calibration standard (e.g., CFP-YFP pair with high, constitutive FRET)
- "FRET-OFF" calibration standard (e.g., CFP-YFP pair with minimal FRET)
- Donor-only and acceptor-only control cells
- Cell culture materials and appropriate growth media
- Confocal or fluorescence microscope capable of spectral imaging or sensitized emission FRET
Methodology:
- Cell Preparation and Plating: Culture and plate cells into appropriate imaging chambers. Prepare separate samples for:
- The experimental biosensor.
- FRET-ON standard cells.
- FRET-OFF standard cells.
- Donor-only control cells.
- Acceptor-only control cells.
Image Acquisition: For all samples, acquire fluorescence images under identical settings.
- Excite the donor and collect donor channel emission.
- Excite the donor and collect acceptor (FRET) channel emission.
- Excite the acceptor and collect acceptor channel emission.
- It is critical to keep all acquisition parameters (e.g., laser power, detector gain, exposure time) constant throughout the session.
Signal Correction and Calibration:
- Use the donor-only and acceptor-only cells to calculate spectral bleed-through (crosstalk) coefficients.
- Apply these coefficients to correct the raw FRET images of the biosensor and calibration standards.
- Calculate the apparent FRET ratio (R) for each pixel/cell: R = Corrected Acceptor Emission / Donor Emission.
- Normalize the experimental biosensor's FRET ratio using the calibration standards. The theoretical model indicates that using both high- and low-FRET standards is necessary for robust calibration under different excitation intensities [9]. The calibrated ratio becomes independent of the imaging conditions.
FRET Efficiency Calculation: With the calibrated ratios and the controls, the actual FRET efficiency (E) can be computed using the formula: E = 1 / (1 + β(R - Rmin)/(Rmax - R)), where β is a instrument-specific constant, and Rmin and Rmax are derived from the FRET-OFF and FRET-ON standards, respectively [9].
Key Experimental Data: This method has been validated to restore reciprocal changes in donor and acceptor signals that are often obscured by imaging fluctuations and photobleaching. The calibrated FRET ratio becomes independent of laser intensity and detector sensitivity, enabling reliable comparison across different experiments and long-term studies [9].
Protocol 2: Transfer Learning for Sensor Calibration Transfer
This protocol outlines the use of transfer learning, a machine learning technique, to adapt a pre-trained calibration model to a new sensor unit with minimal new data, effectively addressing manufacturing tolerances [61].
Objective: To drastically reduce the calibration time for a new metal oxide semiconductor (MOS) gas sensor intended for VOC detection in complex backgrounds.
Materials:
- A primary, fully calibrated "source" sensor (with a large, pre-existing calibration dataset)
- A new "target" sensor to be calibrated
- Gas mixing apparatus for generating standard gas mixtures
- Data acquisition system
Methodology:
- Initial Model Development (Source Domain):
- Expose the source sensor to a wide range of gas mixtures (e.g., 930 unique mixtures) spanning the expected operating conditions, including various interferents and humidity levels [61].
- Record the sensor's response (e.g., resistance or conductance over a temperature cycle) for each mixture.
- Train a robust initial machine learning model (e.g., a Convolutional Neural Network, TCOCNN) to predict analyte concentration from the raw sensor response data. This model serves as the pre-trained base.
Transfer Sampling (Target Domain):
- Expose the new target sensor to a very small subset of representative gas mixtures (as few as 0.7% of the samples used for the source sensor, equivalent to ~2 hours of data collection vs. 10 days) [61].
- Record the target sensor's responses to these transfer samples.
Model Transfer via Transfer Learning:
- Take the pre-trained model from the source sensor.
- "Freeze" the initial layers of the model, which are presumed to extract general features.
- Replace and "re-train" (fine-tune) only the final layers of the model using the small dataset collected from the target sensor. This allows the model to adapt to the specific response characteristics of the new sensor.
Validation:
- Validate the transferred model on a separate, independent dataset measured with the target sensor.
- Compare the prediction accuracy (e.g., Root Mean Squared Error - RMSE) against models built using other transfer methods like Direct Standardization (DS) or a model built from scratch on the target sensor's small dataset.
Key Experimental Data: In a comparative study, transfer learning outperformed DS and PDS. For acetone detection, an initial model built with data from six different sensors and then fine-tuned via transfer learning achieved an RMSE of around 18 ppb with only 2 hours of calibration data for the new sensor, a 99.3% reduction in calibration time [61].
Visualizing Calibration Assessment Workflows
The following diagram illustrates the logical workflow for selecting and applying a calibration method based on the specific research context and challenges.
Calibration Method Selection Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful execution of the described protocols requires specific reagents and materials. The following table details key solutions for setting up calibrated biosensing experiments, particularly those involving FRET and electrochemical systems.
Table 2: Essential Research Reagents and Materials for Biosensor Calibration
| Research Reagent / Material | Function and Application in Calibration |
|---|---|
| FRET-ON & FRET-OFF Standards | Genetically encoded constructs that provide stable high and low FRET signals, serving as internal references to normalize experimental biosensor data and correct for instrument-based variations [9]. |
| Covalent Organic Frameworks (COFs) | Crystalline porous materials used as electrode modifiers or probe carriers in electrochemical immunosensors. Their high surface area and stability enhance sensitivity and serve as a stable platform for bioreceptor immobilization, improving calibration stability [97]. |
| Graphene Foam Electrodes | A high-conductivity, three-dimensional electrode material. When functionalized (e.g., COOH-GF), it provides a large, stable surface for biomolecule immobilization, preserving electrical properties crucial for generating reproducible signals in electrochemical detection [97]. |
| Liquid Metal Composites | Materials like liquid metal particles (LMPs) in stretchable polymers. Used in wearable sensors, they provide stable conductivity under mechanical deformation, ensuring reliable signal acquisition during movement for in-situ monitoring [97]. |
| Bacteriophage-Graphene Hybrids (Graphages) | Bio-nanomaterials used for specific bacterial pathogen detection. Bacteriophages provide exquisite specificity, while graphene enables sensitive electrochemical transduction, creating a stable and selective sensing platform [97]. |
Conclusion
The accuracy of in-vivo biosensing is fundamentally tied to the selection and implementation of appropriate calibration methods. This analysis demonstrates that no single approach is universally superior; rather, method selection must balance clinical accuracy requirements (±20% for many applications), practical usability, and specific biological matrix constraints. Key findings indicate that matching calibration media and temperature to measurement conditions significantly enhances accuracy, while ratiometric and dual-frequency methods offer promising paths toward calibration-free operation. Future directions should focus on developing standardized validation protocols, creating more robust biosensor designs resistant to environmental interference, and advancing machine learning algorithms for adaptive calibration that minimizes user intervention while maintaining clinical-grade accuracy across diverse physiological conditions.
References
- 1. Biosensors, Artificial Intelligence Biosensors, False Results ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025796/]
- 2. Challenges in the application of biosensor technology ... [https://www.frontiersin.org/journals/sensors/articles/10.3389/fsens.2025.1641221/full]
- 3. Improved calibration of electrochemical aptamer-based ... [https://www.nature.com/articles/s41598-022-09070-7]
- 4. Accuracy of the one-point in vivo calibration of "wired" glucose ... [https://pubmed.ncbi.nlm.nih.gov/9608851/]
- 5. Continuous monitoring of biomolecular targets in vivo ... [https://www.sciencedirect.com/science/article/pii/S2451910325001243]
- 6. Smartphone-Based Biosensors: Current Trends ... [https://www.mdpi.com/2673-4591/106/1/10]
- 7. A photoelectrochemical biosensor based on self ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566324002793]
- 8. pH calibration allows accurate glucose detection in ... [https://www.nature.com/articles/s41467-025-65453-0]
- 9. Robust calibration and quantification of FRET signals using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595091/]
- 10. Addressing Signal Drift and Screening for Detection of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12327215/]
- 11. The measures of biosensor performance and how to ... [https://blog.igii.uk/the-measures-of-biosensor-performance-and-how-to-improve-accuracy]
- 12. Biosensors, Volume 15, Issue 5 (May 2025) – 69 articles [https://www.mdpi.com/2079-6374/15/5]
- 13. Bioinks and biofabrication techniques for biosensors ... [https://www.sciencedirect.com/science/article/pii/S2590006424002461]
- 14. Interstitium versus Blood Equilibrium in Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5983095/]
- 15. Multi-biosensing hairband for emergency health assessment [https://www.nature.com/articles/s41467-025-62556-6]
- 16. Monitoring blood lactate dynamics through sweat and ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914025014766]
- 17. Metabolomics of Interstitial Fluid, Plasma and Urine in ... [https://www.mdpi.com/2075-4418/10/11/936]
- 18. In vivo biosensing: progress and perspectives - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5520645/]
- 19. Effect of mild to extreme pH, temperature, and ionic ... [https://www.sciencedirect.com/science/article/abs/pii/S0022286024032599]
- 20. Effects of Physiological-Scale Variation in Cations, pH, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11855119/]
- 21. The Role of Calibration Practices in Optimizing CGM ... [https://www.sciencedirect.com/science/article/pii/S2949788425000668]
- 22. Expediting field-effect transistor chemical sensor design with ... [https://pubs.rsc.org/en/content/articlehtml/2025/me/d4me00203b]
- 23. Accurate and Fast Thermal Sensing via Phase-Responsive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12636073/]
- 24. Ex vivo and in vivo fluorescence detection and imaging of ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-021-00930-4]
- 25. Recent Developments in Microneedle Biosensors for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388307/]
- 26. A Quantitative Comparison of Calibration Methods for RGB ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5336030/]
- 27. A red fluorescent genetically encoded biosensor for in vivo ... [https://www.nature.com/articles/s41467-025-64484-x]
- 28. Part 2. Superiority of the one-point calibration method [https://www.sciencedirect.com/science/article/abs/pii/S0956566301003049]
- 29. Comparison Between One-Point Calibration and Two- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4764224/]
- 30. Calibration of a subcutaneous amperometric glucose sensor [https://www.sciencedirect.com/science/article/abs/pii/S0956566301003062]
- 31. Two-point calibration protocol for the Förster Resonance ... [https://www.spiedigitallibrary.org/journals/neurophotonics/volume-12/issue-S2/S22807/Two-point-calibration-protocol-for-the-F%C3%B6rster-Resonance-Energy-Transfer/10.1117/1.NPh.12.S2.S22807.full]
- 32. Dual-Frequency, Ratiometric Approaches to EAB Sensor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11821477/]
- 33. Calibration-Free Electrochemical Biosensors Supporting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6519131/]
- 34. Rapid, high-sensitivity detection of biomolecules using ... [https://www.nature.com/articles/s41598-023-41436-3]
- 35. Sensitivity, high throughput, and smart detection [https://www.sciencedirect.com/science/article/abs/pii/S0924424724001134]
- 36. The Role of Artificial Intelligence in Advancing Biosensor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12392873/]
- 37. A revisit on intraparticle diffusion models with analytical ... [https://www.sciencedirect.com/science/article/abs/pii/S2214714424004732]
- 38. The Reaction–Diffusion Models in Biomedicine [https://www.mdpi.com/2076-3417/13/21/11672]
- 39. Urea Detection in Phosphate Buffer and Artificial Urine [https://pmc.ncbi.nlm.nih.gov/articles/PMC12608829/]
- 40. Trends in the Design of Intensity-Based Optical Fiber ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8232210/]
- 41. Recent advances and current trends in optical fiber ... [https://www.sciencedirect.com/science/article/pii/S0165993624001456]
- 42. Optical Fibre-Based Sensors—An Assessment of Current ... [https://www.mdpi.com/2079-6374/13/9/835]
- 43. A comprehensive review of graphene-based biosensors [https://pmc.ncbi.nlm.nih.gov/articles/PMC12448920/]
- 44. Advances in Biosensors for Continuous Glucose ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8416677/]
- 45. Limits to the Evaluation of the Accuracy of Continuous ... [https://www.mdpi.com/2079-6374/8/2/50]
- 46. Accuracy of a novel calibratable real-time continuous ... [https://pubmed.ncbi.nlm.nih.gov/40331145/]
- 47. Comparative Performance Analysis of Manual and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12226519/]
- 48. Performance of Three Continuous Glucose Monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11795573/]
- 49. Clinical accuracy of a continuous glucose monitoring ... [https://pubmed.ncbi.nlm.nih.gov/25370149/]
- 50. Minimally and non-invasive glucose monitoring [https://pubs.rsc.org/en/content/articlehtml/2025/sd/d4sd00360h]
- 51. Continuous monitoring of diabetes with an integrated ... [https://www.nature.com/articles/s41378-021-00302-w]
- 52. 5 Best Continuous Glucose Monitors for 2025 [https://www.type1strong.org/blog-post/5-best-continuous-glucose-monitors-for-2025]
- 53. Best Glucose Monitors: 6 Pharmacist-Ranked Brands for 2025 [https://health.usnews.com/otc/rankings/blood-glucose-monitors]
- 54. 6 Best Glucose Monitors 2025: CGMs, apps, and more [https://www.healthline.com/health/diabetes/best-glucose-monitors]
- 55. Point-of-care biosensors for infectious disease diagnosis [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03897a?page=search]
- 56. Sensitivity calibration of in vivo sensors used to measure ... [https://patents.google.com/patent/US12279866B2/en]
- 57. Sensitivity-Enhancing Strategies in Optical Biosensing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7884068/]
- 58. Improvement of a highly sensitive and specific whole-cell ... [https://www.sciencedirect.com/science/article/pii/S2405805X2300025X]
- 59. Machine learning-based prediction and interpretation of ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25030048]
- 60. AI-Enhanced Electrochemical Sensing Systems: A Paradigm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467342/]
- 61. Comparison of Transfer Learning and Established ... [https://www.mdpi.com/2073-4433/14/7/1123]
- 62. A guide to reducing noise and increasing sensitivity in ... [https://blog.igii.uk/a-guide-to-reducing-noise-and-increasing-sensitivity-in-biosensors]
- 63. In vivo simultaneous proton resonance frequency shift ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11893039/]
- 64. Initial findings creating a temperature prediction model ... [https://www.nature.com/articles/s41598-025-92202-6]
- 65. 3 Methods of Temperature Sensor Calibration: Pros and ... [https://www.fluke.com/en-us/learn/blog/calibration/three-methods-calibrating-temperature-sensors?srsltid=AfmBOorT-GCA8a653oHUvdqs2oMvzpYNgJKTJ_7zFaLsu11ubnzYhf1z]
- 66. Red Blood Cells and Human Aging: Exploring Their ... [https://www.mdpi.com/2075-4418/15/16/1993]
- 67. Triple-mode biosensing strategies: A critical review of ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25023550]
- 68. Robust calibration and quantification of FRET signals using ... [https://www.sciencedirect.com/science/article/pii/S2589004225020048]
- 69. Biological age estimation using circulating blood biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC10603148/]
- 70. Stanford Medicine-led study finds way to predict which of our ... [https://med.stanford.edu/news/all-news/2023/12/aging-organs.html]
- 71. Programming cell-free biosensors with DNA strand ... [https://www.nature.com/articles/s41589-021-00962-9]
- 72. Nanomaterial-mediated self-calibrating biosensors for ultra ... [https://www.sciencedirect.com/science/article/abs/pii/S0010854524005502]
- 73. In-situ baseline calibration approach for enhanced data ... [https://www.nature.com/articles/s41612-025-01184-9]
- 74. Dynamic calibration of low-cost PM2.5 sensors using trust- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12228579/]
- 75. Field-based calibration and operation of low-cost sensors ... [https://www.sciencedirect.com/science/article/pii/S1309104225002788]
- 76. Validation framework for in vivo digital measures - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11751004/]
- 77. engineering encapsulation for whole-cell biosensors [https://www.sciencedirect.com/science/article/pii/S0167779925004470]
- 78. Dynamic Validation of Calibration Accuracy and Structural ... [https://www.mdpi.com/1424-8220/24/12/3896]
- 79. Everything's under Control: Maximizing Biosensor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11840803/]
- 80. Clinical Validation of Biosensors: Protocols That Investors ... [https://medstartups.org/clinical-validation-biosensors-protocols-investors-expect]
- 81. Biosensors, Volume 15, Issue 9 (September 2025) [https://www.mdpi.com/2079-6374/15/9]
- 82. Biosensors, Volume 15, Issue 11 (November 2025) [https://www.mdpi.com/2079-6374/15/11]
- 83. Advancing protein biosensors: redefining detection through ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d4ra06791f]
- 84. Biosensors and Bioelectronics | Vol 286, 15 October 2025 [https://www.sciencedirect.com/journal/biosensors-and-bioelectronics/vol/286/suppl/C]
- 85. -Based Biosensors for Sepsis Diagnosis... Electrochemical Aptamer [https://pubmed.ncbi.nlm.nih.gov/40710052/]
- 86. Real-time, In-vivo Molecular Monitoring Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9840907/]
- 87. A genetically encoded biosensor for point-of-care and live ... [https://www.nature.com/articles/s41467-025-62225-8]
- 88. Illuminating plant metabolism with genetically encoded ... [https://www.sciencedirect.com/science/article/pii/S017616172500080X]
- 89. A highly sensitive label-free aptamer sensor for timely detection of... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra05254h]
- 90. In vivo calibration of genetically encoded metabolite ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/36726217/]
- 91. Clarke Error Grid [https://en.wikipedia.org/wiki/Clarke_Error_Grid]
- 92. Clarke Error Grid Analysis - File Exchange - MATLAB Central [https://www.mathworks.com/matlabcentral/fileexchange/20545-clarke-error-grid-analysis]
- 93. Clarke Error Grid Analysis for Performance Evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8993970/]
- 94. Validation of the Diabetes Technology Society Error Grid [https://pmc.ncbi.nlm.nih.gov/articles/PMC11851577/]
- 95. Clinical validation of noninvasive blood glucose ... [https://www.nature.com/articles/s43856-025-01241-7]
- 96. Machine‐Learning‐Aided Advanced Electrochemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12369699/]
- 97. Biosensors, Volume 15, Issue 7 (July 2025) – 74 articles [https://www.mdpi.com/2079-6374/15/7]