Evaluating Biosensor Sensitivity and Specificity: From Foundational Concepts to Clinical Validation
This article provides a comprehensive evaluation of biosensor sensitivity and specificity, tailored for researchers, scientists, and drug development professionals.
Evaluating Biosensor Sensitivity and Specificity: From Foundational Concepts to Clinical Validation
Abstract
This article provides a comprehensive evaluation of biosensor sensitivity and specificity, tailored for researchers, scientists, and drug development professionals. It explores the fundamental principles defining sensor performance, including key metrics like limit of detection (LOD), wavelength sensitivity, and figure of merit (FOM). The scope extends to advanced methodological applications across biomedical fields, such as cancer cell detection and therapeutic monitoring, alongside emerging optimization strategies leveraging machine learning and novel materials. The content further addresses critical troubleshooting for real-world performance and outlines rigorous clinical validation protocols and comparative analyses essential for regulatory approval and successful translation into clinical and research settings.
Defining Performance: Core Principles and Metrics for Biosensor Sensitivity and Specificity
In the development and evaluation of biosensors, specific analytical parameters are used to quantitatively assess performance, ensure reliability, and validate results for clinical or research use. For scientists and professionals in drug development, a precise understanding of these Figures of Merit (FOMs) is not merely academic; it is critical for selecting appropriate diagnostic tools, interpreting experimental data accurately, and ultimately making decisions that can accelerate drug discovery and ensure patient safety.
This guide provides a structured comparison of these fundamental concepts—Sensitivity, Specificity, Limit of Detection (LOD), and related metrics—framed within the context of biosensor research. We will define these terms, outline standard protocols for their determination, present comparative performance data from real-world studies, and provide a toolkit for their practical application in the laboratory.
Core Definitions and Mathematical Foundations
The performance of a biosensor or diagnostic test is fundamentally characterized by its ability to correctly identify the presence and quantity of an analyte. The following parameters form the cornerstone of this evaluation.
2.1 Sensitivity and Specificity: Diagnostic Accuracy
Sensitivity and Specificity are statistical measures used to evaluate the clinical or diagnostic accuracy of a binary classification test, such as distinguishing between diseased and healthy states [1].
- Sensitivity, or the true positive rate, measures the proportion of actual positives that are correctly identified. A test with high sensitivity effectively rules out the disease when the result is negative (often summarized as "SnOut").
- Specificity, or the true negative rate, measures the proportion of actual negatives that are correctly identified. A high specificity effectively rules in the disease when the result is positive ("SpIn") [1].
These concepts are intrinsically linked to the Confusion Matrix and the Receiver Operating Characteristic (ROC) curve. The ROC curve plots the true positive rate (Sensitivity) against the false positive rate (1-Specificity) at various threshold settings. The Area Under the Curve (AUC) of the ROC curve provides a single measure of overall accuracy, where an AUC of 1.0 represents a perfect test, and 0.5 represents a test no better than chance [1].
2.2 Limit of Detection (LOD) and Limit of Quantification (LOQ): Analytical Sensitivity
While diagnostic sensitivity refers to the rate of true positives, the term "sensitivity" in an analytical context often relates to the smallest detectable amount of an analyte. This is formally defined by the LOD and LOQ [1] [2].
- Limit of Detection (LOD): The lowest quantity of an analyte that can be reliably distinguished from its absence. According to the widely accepted IUPAC definition, for a signal to be deemed detectable, it must be greater than the signal from a blank sample by three times the standard deviation of the blank (S > 3σ) [1] [2]. This provides a 99% confidence level for a false positive.
- Limit of Quantification (LOQ): The lowest concentration of an analyte that can be quantitatively determined with stated acceptable precision and accuracy. It is typically defined as a signal ten times greater than the noise level (S > 10σ) [1].
It is crucial to distinguish between analytical sensitivity (LOD) and diagnostic sensitivity (true positive rate), as they address different aspects of a test's performance [1] [3].
2.3 Selectivity vs. Specificity
Although sometimes used interchangeably, selectivity and specificity have distinct meanings in biosensor science. Specificity refers to the ability of a bioreceptor (e.g., an antibody) to assess an exact analyte in a mixture. In contrast, selectivity is the broader ability of the biosensor to differentiate the target analyte from other interfering substances or contaminants in a sample matrix [1] [3].
Table 1: Summary of Key Figures of Merit in Biosensor Evaluation
| Figure of Merit | Definition | Typical Benchmark | Primary Significance |
|---|---|---|---|
| Sensitivity (Diagnostic) | Proportion of true positives correctly identified [1]. | Varies by application; e.g., ≥80% for SARS-CoV-2 LFDs per WHO [4]. | Ability to rule out a disease (SnOut). |
| Specificity | Proportion of true negatives correctly identified [1]. | Varies by application; e.g., ≥97% for SARS-CoV-2 LFDs per WHO [4]. | Ability to rule in a disease (SpIn). |
| Limit of Detection (LOD) | Lowest analyte concentration distinguishable from a blank [1] [2]. | Signal-to-Noise > 3 (S > 3σ) [1]. | Measure of analytical sensitivity. |
| Limit of Quantification (LOQ) | Lowest analyte concentration that can be accurately measured [1]. | Signal-to-Noise > 10 (S > 10σ) [1]. | Lower limit of the quantitative range. |
| Selectivity | Ability to differentiate target analyte from interferents in a mixture [1] [3]. | N/A | Resistance to false signals from sample matrix. |
Experimental Protocols for Determining FOMs
Standardized experimental protocols are essential for the consistent and accurate determination of these FOMs. Below are detailed methodologies for key assays.
3.1 Protocol for Determining Limit of Detection (LOD)
The following procedure outlines a general method for establishing the LOD for an amperometric biosensor, which can be adapted for other transducer types [1].
- Signal Measurement: Perform repeated measurements (n ≥ 10) of a blank sample (a sample without the analyte) to establish the baseline signal and its standard deviation (σ).
- Calibration Curve: Prepare and analyze a series of standard solutions with known analyte concentrations across the expected range. Plot the signal response against concentration to generate a calibration curve.
- LOD Calculation: Apply the formula derived from the calibration curve. The LOD is calculated as the concentration corresponding to the mean blank signal plus three times the standard deviation of the blank. Mathematically, if the calibration curve is
y = ax + b, whereyis the signal andxis the concentration, then:
3.2 Protocol for Evaluating Diagnostic Sensitivity/Specificity
Evaluating diagnostic sensitivity and specificity requires a clinical study comparing the test device against a reference standard [4].
- Sample Collection: Obtain well-characterized clinical samples (e.g., surplus patient samples from a healthcare setting) that include both positive and negative cases for the condition of interest.
- Blinded Testing: Analyze all samples using the biosensor or test device under evaluation. The operators should be blinded to the reference results to prevent bias.
- Reference Method Comparison: Compare the results from the test device with those from a validated reference method (e.g., RT-PCR for viral detection, or culture for bacterial detection).
- Statistical Analysis: Construct a 2x2 confusion matrix to classify results into True Positives (TP), False Positives (FP), True Negatives (TN), and False Negatives (FN).
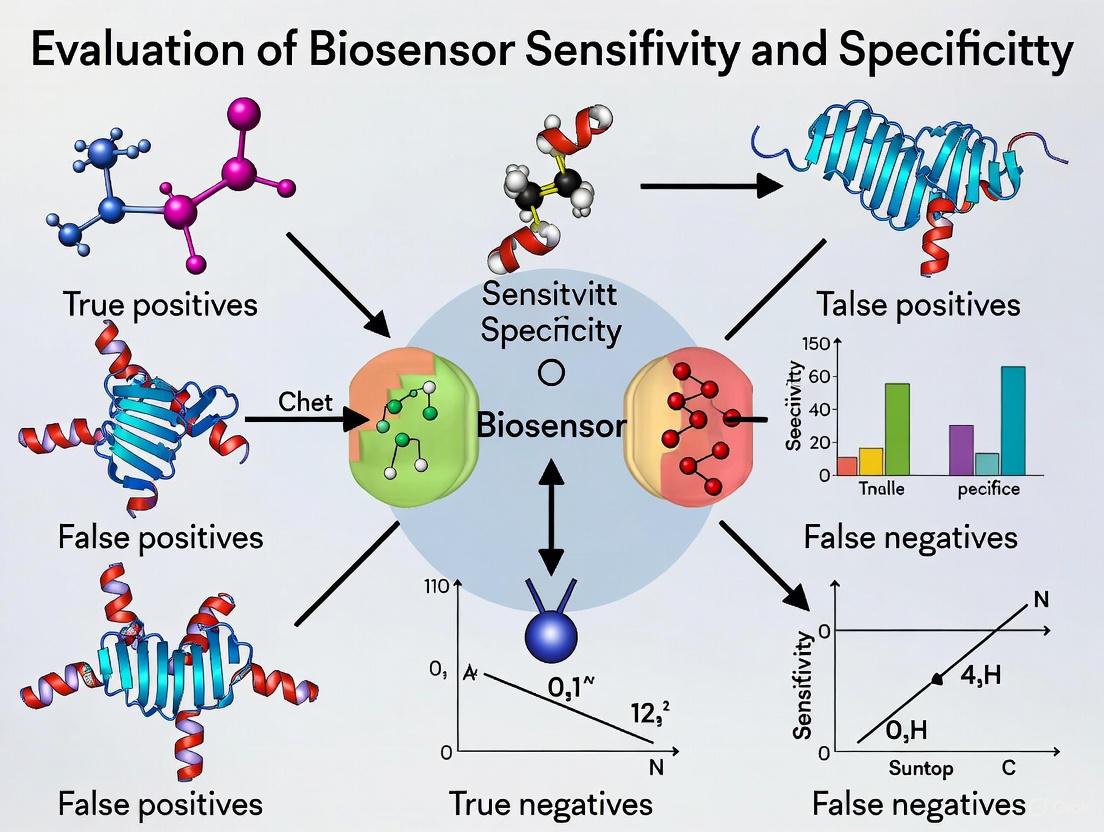
The following diagram illustrates the logical workflow and calculations involved in this validation process.
Comparative Performance Data in Practice
Independent, real-world evaluations often reveal performance variations that may differ from manufacturer claims. This is critical for professionals making procurement or deployment decisions.
4.1 Independent Evaluation of SARS-CoV-2 Lateral Flow Devices (LFDs)
A large-scale independent evaluation by the UK Health Security Agency (UKHSA) of 86 SARS-CoV-2 LFDs highlights this discrepancy.
- Claimed vs. Actual Performance: The study found that while 73 of the 86 LFDs claimed clinical sensitivity ≥85% in their instructions for use, the UKHSA-determined sensitivity ranged from 32% to 83% [4].
- Lack of Correlation: The analysis found "no evidence of correlation between manufacturer-reported test sensitivity and UKHSA determined test sensitivity," underscoring the necessity of independent verification for critical performance metrics [4].
4.2 Comparison of Molecular vs. Antigen Tests for Strep A
A 2025 comparative study of Group A Streptococcus (GAS) tests provides a clear example of how different technologies yield different LODs, directly impacting analytical sensitivity.
- Study Design: The study compared the LoD of one molecular point-of-care test (ID NOW Strep A 2) and three lateral flow immunoassays (BD Veritor, Sofia, OSOM) using serial dilutions of bacterial isolates [5].
- Results: The molecular test demonstrated a significantly lower LoD (3.125 × 10³ to 2.5 × 10⁴ CFU/mL) compared to the lateral flow assays (1 × 10⁶ to 1.5 × 10⁷ CFU/mL), confirming its higher analytical sensitivity [5].
Table 2: Comparative Analytical Sensitivity of Diagnostic Tests for Group A Streptococcus
| Test Name | Technology | Limit of Detection (LoD) Range (CFU/mL) | Relative Sensitivity |
|---|---|---|---|
| ID NOW Strep A 2 | Molecular (POC) | 3.125 × 10³ to 2.5 × 10⁴ [5] | Highest |
| Sofia Strep A+ | Lateral Flow (FIA) | 1 × 10⁶ to 1 × 10⁷ [5] | Medium |
| BD Veritor Plus | Lateral Flow | 1 × 10⁷ to 1.5 × 10⁷ [5] | Low |
| OSOM Strep A | Lateral Flow | 1 × 10⁷ [5] | Low |
The LOD Paradox: Contextualizing the Need for Sensitivity
A critical consideration in biosensor research is that a lower LOD is not always synonymous with a better biosensor. This is known as the "LOD paradox" [6].
- Clinical Relevance over Pure Sensitivity: The primary goal should be to detect analytes within their clinically significant range. A biosensor capable of detecting a biomarker at picomolar levels is technologically impressive, but if the biomarker's pathological concentration is in the nanomolar range, that ultra-sensitivity may be redundant. It can even be detrimental, adding unnecessary complexity, cost, and potential for interference without improving clinical outcomes [6].
- Balancing Performance Characteristics: The pursuit of an ultra-low LOD can sometimes compromise other vital features, such as the dynamic range, robustness, ease of use, and cost-effectiveness. A holistic approach that balances sensitivity with real-world applicability, regulatory compliance, and user needs is essential for developing impactful biosensors [6].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key materials and reagents commonly used in the development and validation of biosensors, particularly those based on electrochemical or immunoassay principles.
Table 3: Essential Research Reagent Solutions for Biosensor Development
| Material/Reagent | Function in Biosensor Development | Example Use Case |
|---|---|---|
| Bioreceptors (Antibodies, Aptamers, Enzymes) | The biological recognition element that binds specifically to the target analyte [3]. | Immobilized on a transducer surface to capture glucose (enzyme) or a viral antigen (antibody). |
| Silicon Nanowire Chips | A transducer platform that converts a bio-recognition event into an electrical signal [7] [8]. | Used in platforms like ASG's sensors for highly sensitive, multiplexed detection of host cell proteins [7] [8]. |
| Electrochemical Cell/Buffer | Provides the controlled chemical environment necessary for electrochemical measurements [1]. | Used in amperometric biosensors to maintain stable pH and ionic strength during signal measurement. |
| Reference Material (ATCC isolates) | Well-characterized samples used as a gold standard for determining LoD and validating assay accuracy [5]. | Serial dilution of S. pyogenes ATCC isolates to establish the LoD of a Strep A test [5]. |
| Lateral Flow Test Strips | A porous substrate that enables capillary flow for the separation and detection of analytes in rapid tests [4]. | The core component of SARS-CoV-2 antigen tests and home pregnancy tests. |
The evaluation of biosensor performance hinges on a set of core, quantifiable metrics that allow researchers to objectively compare technologies and predict their behavior in real-world applications. Wavelength sensitivity (WS), amplitude sensitivity (AS), and resolution are three such parameters, forming a critical triad for assessing a sensor's ability to detect minute biological events. Within the broader thesis of biosensor evaluation, understanding the practical interplay and trade-offs between these metrics is paramount for selecting the appropriate technology for specific applications, from early disease diagnostics to drug discovery. This guide provides a comparative analysis of contemporary biosensor technologies by synthesizing experimental data and detailed methodologies from recent, high-impact research.
Core Quantitative Metrics and Performance Comparison
Defining the Metrics
- Wavelength Sensitivity (WS) is a measure of the shift in the resonance wavelength (typically in nanometers, nm) per unit change in the refractive index (RI) of the surrounding medium. It is expressed in nm/RIU (Refractive Index Unit). A higher WS indicates that the sensor can produce a larger, more easily measurable signal for a small molecular binding event.
- Amplitude Sensitivity (AS) quantifies the change in the intensity or amplitude of the reflected or transmitted light at a fixed wavelength for a unit change in RI. It is expressed in RIU⁻¹. A sensor with high AS is adept at detecting intensity variations, which can be advantageous for certain detection schemes.
- Resolution defines the smallest detectable change in refractive index. It is inversely related to sensitivity and is expressed in RIU. A lower resolution value signifies a finer ability to distinguish between minute changes in analyte concentration.
Comparative Performance of Advanced Biosensors
The table below synthesizes experimental and simulation data from recent studies, providing a direct comparison of these metrics across different biosensor architectures.
Table 1: Comparative Performance Metrics of Contemporary Biosensors
| Biosensor Technology | Target Application | Wavelength Sensitivity (nm/RIU) | Amplitude Sensitivity (RIU⁻¹) | Resolution (RIU) | Figure of Merit (RIU⁻¹) |
|---|---|---|---|---|---|
| D-shaped PCF-SPR (Gold-TiO₂) [9] | Multi-cancer detection | 42,000 | -1,862.72 | Not Specified | 1,393.13 |
| ML-optimized PCF-SPR [10] | Chemical & cancer sensing | 125,000 | -1,422.34 | 8.00 × 10⁻⁷ | 2,112.15 |
| PCF-SPR (Dual-core) [11] | Basal cancer cell detection | 10,000 | Not Specified | Not Specified | Not Specified |
| Reflection-type GMR Metasurface [12] | Gastric cancer biomarker (CK8/18) | 420.33 | Not Specified | Not Specified | Not Specified |
| Graphene-Silver Metasurface [13] | COVID-19 detection | 400 (GHz/RIU)* | Not Specified | Not Specified | 5.000 |
Note: *This value is in GHz/RIU; conversion to nm/RIU is wavelength-dependent and not directly comparable.
The data reveals that photonic crystal fiber surface plasmon resonance (PCF-SPR) sensors currently push the boundaries of raw wavelength sensitivity, with machine learning (ML)-optimized designs achieving exceptional performance [10]. The incorporation of oxide layers like TiO₂ alongside gold has also proven highly effective for sensitivity enhancement [9]. In contrast, metasurface-based sensors, while demonstrating high figures of merit and excellent integration potential, often report more modest sensitivity values [13] [12].
Experimental Protocols and Methodologies
The high performance of modern biosensors is underpinned by rigorous design and validation protocols. The following workflows are foundational to the field.
Machine Learning-Enhanced Sensor Design and Optimization
The integration of machine learning represents a paradigm shift from traditional, computationally expensive iterative simulation methods.
Diagram 1: ML-driven biosensor optimization workflow.
Detailed Workflow:
- Parametric Design Definition: The process begins with defining the initial biosensor geometry and material properties. Key parameters include air hole diameter in PCFs, pitch distance, thickness of plasmonic layers (e.g., gold), and analyte layer thickness [10].
- Computational Modeling: The designed sensor is modeled using finite-element method (FEM) software, primarily COMSOL Multiphysics. This step simulates the sensor's optical behavior, such as mode propagation and the excitation of surface plasmons, across a range of refractive indices (e.g., 1.33 to 1.40) to generate data on effective index and confinement loss [11] [10].
- Dataset Generation: Data from thousands of simulations are compiled into a structured dataset, where the input features are the design parameters and the output targets are the performance metrics (effective index, confinement loss).
- Machine Learning Model Training: Regression models like Gradient Boosting (GBR), Extreme Gradient Boosting (XGBR), and Random Forest (RF) are trained on this dataset. These models learn the complex relationships between design parameters and sensor performance, achieving high predictive accuracy (R² > 0.99) [11] [10].
- Explainable AI Analysis: Techniques like SHapley Additive exPlanations (SHAP) are applied to interpret the ML models. This identifies the most influential design parameters (e.g., gold thickness, pitch, wavelength) on sensitivity and loss, providing actionable insights for optimization [10].
- Performance Validation: The optimized design parameters identified by the ML and XAI pipeline are validated through final simulations, confirming the predicted enhancements in sensitivity, resolution, and figure of merit [10].
Fabrication and Experimental Validation of Metasurface Biosensors
For metasurface sensors, sophisticated nanofabrication techniques are required to translate the design into a functional device.
Diagram 2: Metasurface biosensor fabrication and testing.
Detailed Workflow:
- Substrate Preparation: A silicon dioxide (SiO₂) substrate is rigorously cleaned using standard semiconductor cleaning protocols (e.g., RCA cleaning) to remove organic and metallic contaminants [13].
- Graphene Transfer: A high-quality monolayer of graphene is synthesized via chemical vapor deposition (CVD) on a copper foil and then transferred onto the SiO₂ substrate using a polymer support layer (e.g., PMMA), followed by etching and annealing [13].
- Metasurface Patterning: The intricate metasurface pattern (e.g., circular rings, rectangular resonators) is defined using high-resolution electron beam lithography (EBL). A layer of electron-sensitive resist is spin-coated, exposed to the electron beam according to the design, and developed [13].
- Metal Deposition and Lift-off: A thin film of plasmonic metal (silver or gold) is deposited onto the patterned substrate using electron beam evaporation. A subsequent lift-off process in acetone removes excess metal, leaving behind the precise metasurface structures [13].
- Surface Functionalization: The sensor surface is bio-functionalized by immobilizing specific biorecognition elements, such as monoclonal antibodies. This often involves chemical linkers like EDC/NHS to covalently bind antibodies to the sensor surface [14] [15].
- Optical Characterization and Sensing: The fabricated sensor is integrated into an optical setup. A tunable laser source emits light, which is polarized and coupled into the sensor. The output spectrum is recorded by an optical spectrum analyzer as analytes are introduced, allowing for the measurement of wavelength or amplitude shifts corresponding to binding events [9].
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and operation of high-performance biosensors rely on a suite of specialized materials and reagents.
Table 2: Key Research Reagent Solutions in Biosensor Development
| Item | Function in Biosensor Development | Specific Examples |
|---|---|---|
| Plasmonic Materials | Generate surface plasmon waves for highly sensitive detection. | Gold (Au), Silver (Ag) [13] [9] |
| 2D Materials & Coatings | Enhance field confinement, improve sensitivity, and provide functionalization sites. | Graphene, TiO₂, MoS₂, MXene [13] [11] [9] |
| Biorecognition Elements | Provide specificity by binding to the target analyte. | Monoclonal Antibodies, Aptamers [14] [15] |
| Coupling Reagents | Facilitate covalent immobilization of biorecognition elements onto the sensor surface. | EDC, NHS [14] |
| Optical Substrates | Serve as the mechanical support and optical platform for the sensor. | Silicon Dioxide (SiO₂), Photonic Crystal Fiber (PCF) [13] [9] |
The quantitative comparison of wavelength sensitivity, amplitude sensitivity, and resolution reveals a clear trajectory in biosensor development: complex architectures like PCF-SPR, particularly when enhanced with machine learning and novel materials, are achieving unprecedented sensitivity. However, the choice of biosensor must align with the specific application requirements, considering not only raw sensitivity but also factors like portability, cost, and ease of fabrication. Metasurface and other miniaturized platforms offer a compelling balance for point-of-care applications. As the field progresses, the standardized reporting of this core set of metrics, derived from rigorous and openly shared experimental protocols, will be crucial for advancing the broader thesis of robust biosensor evaluation and accelerating their translation from the research lab to the clinic.
In the pursuit of higher sensitivity and specificity for biosensors, the strategic selection of materials forms the very foundation of signal generation. Plasmonic metals and two-dimensional (2D) materials have emerged as particularly powerful components in the biosensor engineer's toolkit. These materials excel at transducing a biological binding event—such as an antibody attaching to a viral antigen—into a quantifiable, often optical, signal that can be detected with remarkable precision [16]. The operational principle of many advanced optical biosensors, including the widely used surface plasmon resonance (SPR), relies on exciting electron oscillations at a metal-dielectric interface. When the refractive index of the local environment changes due to a molecular binding event, it alters the resonance conditions, producing a detectable signal shift [16] [17]. The integration of 2D materials like graphene, transition metal dichalcogenides (TMDCs) such as MoS₂, and black phosphorus (BP) into these systems has further enhanced performance. Their exceptional surface-to-volume ratios and unique optical properties significantly improve the sensitivity and robustness of biosensing platforms [18] [19] [20]. This guide provides a comparative analysis of these critical materials, underpinned by experimental data, to inform their selection for applications ranging from viral detection to cancer diagnostics.
Comparative Analysis of Material Performance
The performance of a biosensor is quantified through key metrics such as sensitivity, figure of merit (FoM), and limit of detection (LOD). The tables below consolidate recent experimental and simulation data to facilitate a direct comparison between different material configurations.
Table 1: Performance comparison of SPR biosensors using different plasmonic metals and 2D materials.
| Sensor Configuration | Sensitivity (deg/RIU) | Figure of Merit (FoM) (/RIU) | Key Applications Demonstrated | Source |
|---|---|---|---|---|
| BK7/SiO₂/Cu/BaTiO₃ | 568 | 134.75 | Detection of basal, Jurkat, and HeLa cancer cells | [17] |
| BK7/Ag/MoS₂/Graphene | 175% improvement over graphene-only sensor | Not Specified | DNA hybridization detection | [20] |
| CaF₂/TiO₂/Ag/WS₂ (bilayer) | 240.10 | 78.46 | General biochemical sensing | [20] |
| SF10/Cu/Graphene (multiple layers) | Increase with layer count | Not Specified | DNA detection | [20] |
| BK7/Au/WSe₂/PtSe₂/BP | ~200 | 17.70 | General biochemical sensing | [20] |
Table 2: Performance of advanced metasurface and field-effect transistor (FET) biosensors incorporating 2D materials.
| Sensor Type & Configuration | Sensitivity | Limit of Detection (LOD) | Key Advantages | Source |
|---|---|---|---|---|
| Graphene-Ag Metasurface | 400 GHz/RIU | Not Specified | Machine learning-enhanced predictive accuracy (R²=0.90) for COVID-19 detection | [13] |
| SERS Platform (Au-Ag Nanostars) | Not Applicable | 16.73 ng/mL (for α-Fetoprotein) | Label-free cancer biomarker detection using intrinsic vibrational modes | [14] |
| 2D Material-based Bio-FETs (e.g., Graphene, TMDCs, BP) | Very High (general claim) | Very Low (general claim) | Label-free diagnosis, real-time monitoring, portability for point-of-care | [19] |
| SERS Substrate (Ag NPs on Si nanowires) | Not Applicable | 10⁻¹¹ M | Signal amplification by orders of magnitude | [16] |
Fundamental Mechanisms of Signal Generation
The Plasmonic Effect and 2D Material Enhancement
The signal generation in plasmonic biosensors begins with the excitation of surface plasmons. In the most common Kretschmann configuration, a light source is directed through a prism onto a thin plasmonic metal film (e.g., Gold or Silver). At a specific angle of incidence, the energy of the photons is transferred to the electrons in the metal, creating coherent electron oscillations known as surface plasmon polaritons (SPPs). This results in a sharp dip in the reflected light intensity, measured as the resonance angle [16] [17]. When target analyte molecules bind to recognition elements on the sensor surface, they cause a local increase in the refractive index (RI). This RI change directly alters the propagation constant of the SPPs, leading to a measurable shift in the resonance angle or wavelength, which is the core signal of an SPR biosensor [17].
2D materials enhance this process through several mechanisms. Firstly, their large surface area provides abundant sites for biomolecule immobilization, increasing the number of binding events and thus the magnitude of the RI change [19]. Secondly, materials like graphene can act as field enhancers. Their unique electronic properties can intensify the electromagnetic field at the interface, making the sensor more responsive to minute RI variations [20]. Some 2D materials, like TMDCs, also have a high absorption coefficient, leading to more efficient interaction with incident light and a sharper resonance curve, which can improve the detection accuracy [20].
Experimental Workflow for Biosensing
The following diagram illustrates the standard workflow for conducting an experiment and generating a signal using a prism-coupled SPR biosensor, showcasing the integration of plasmonic metals and 2D materials.
Detailed Experimental Protocols
To achieve the reported data, rigorous experimental protocols for sensor fabrication and characterization must be followed. This section outlines the methodologies cited in the comparative tables.
Fabrication of a High-Sensitivity SPR Biosensor
The protocol for a multi-layered SPR sensor, as described in [17], involves precise thin-film deposition and optical characterization.
- Substrate Preparation: Begin with a BK7 prism as the coupling element. Clean the prism surface thoroughly using standard protocols (e.g., RCA cleaning) to remove organic and ionic contaminants [13].
- Layer-by-Layer Deposition:
- SiO₂ Layer: Deposit a 5 nm thick silicon dioxide (SiO₂) layer onto the prism. This layer can be deposited via techniques like sputtering or electron-beam evaporation and acts to enhance sensitivity and protect the metal layer [17].
- Plasmonic Metal Layer: Deposit a 50 nm thick copper (Cu) film onto the SiO₂ layer. The thickness is critical and must be optimized; the deposition is typically performed via thermal or electron-beam evaporation under high vacuum [17].
- Perovskite Layer: Deposit a 15 nm thick layer of barium titanate (BaTiO₃) over the copper. This high-refractive-index material significantly enhances the electromagnetic field, boosting sensitivity [17].
- Functionalization: For specific detection (e.g., of cancer cells), the sensor surface (BaTiO₃) must be functionalized with appropriate biorecognition elements, such as antibodies, using chemical linkers like EDC/NHS chemistry [14].
- Optical Characterization (Angular Interrogation):
- Setup: Use a monochromatic light source (e.g., a 650 nm laser diode). The light must be p-polarized. Mount the sensor on a goniometer to control the angle of incidence precisely [17] [20].
- Measurement: For a range of analyte refractive indices (e.g., 1.33 to 1.335), scan the incident angle and measure the intensity of the reflected light using a photodetector.
- Data Analysis: Plot reflectance versus angle for each analyte. The resonance angle is identified as the angle at which reflectance is minimum. Sensitivity is calculated as the shift in resonance angle per unit change in refractive index (deg/RIU) [17].
Fabrication of a SERS-Based Immunosensor
The protocol for a SERS-based platform for biomarker detection, as in [14], focuses on nanostar synthesis and functionalization.
- Substrate Synthesis: Synthesize Au-Ag nanostars using a wet-chemical method. Their sharp-tipped morphology is crucial for generating intense local electromagnetic "hot spots" [14].
- Nanostar Concentration: Concentrate the nanostars via centrifugation at different durations (e.g., 10, 30, and 60 minutes) to tune their density and SERS performance [14].
- Surface Functionalization:
- Activation: Incubate the nanostars with mercaptopropionic acid (MPA), which forms a self-assembled monolayer via Au-S bonds.
- Conjugation: Activate the carboxyl groups of MPA with a mixture of EDC and NHS. This creates an amine-reactive ester.
- Antibody Immobilization: Add monoclonal anti-α-fetoprotein antibodies (AFP-Ab) to the activated nanostars. The antibodies covalently attach to the MPA layer [14].
- SERS Measurement and Detection:
- Incubation: Incubate the functionalized nanostars with a sample containing the target antigen (AFP).
- Measurement: Use a Raman spectrometer to acquire spectra of the liquid-phase platform. Unlike conventional SERS, this platform detects the intrinsic Raman signal of the captured antigen itself, eliminating the need for a separate Raman reporter [14].
- Quantification: The intensity of the characteristic Raman peaks of the antigen is correlated with its concentration. The LOD is determined from the calibration curve, following statistical guidelines (e.g., EP17 protocol which involves measuring the limit of blank and low concentration samples) [16] [14].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key materials and their functions for developing and working with plasmonic biosensors.
Table 3: Essential materials and reagents for plasmonic biosensor research.
| Item Name | Function / Role in Experiment | Specific Examples |
|---|---|---|
| Plasmonic Metal Films | Serves as the active layer for generating surface plasmon polaritons (SPPs). | Gold (Au), Silver (Ag), Copper (Cu) [17] [20] |
| 2D Nanomaterials | Enhances sensitivity, provides high surface area for bioreceptor immobilization, and protects the metal layer. | Graphene, MoS₂, WS₂, Black Phosphorus (BP), WSe₂ [18] [19] [20] |
| Prism Couplers | Optical component to enable the phase-matching condition for SPR excitation via attenuated total reflection (ATR). | BK7 glass, SF10 glass [17] [20] |
| Biorecognition Elements | Provides specificity by binding to the target analyte, inducing the measurable refractive index change. | Antibodies, Aptamers, DNA strands [16] [14] [19] |
| Chemical Linkers | Facilitates the covalent immobilization of biorecognition elements onto the sensor surface. | EDC, NHS, MPA (Mercaptopropionic Acid) [14] |
| High-Refractive-Index Layers | Used in hybrid designs to further concentrate the electromagnetic field and boost sensitivity. | Barium Titanate (BaTiO₃), Silicon (Si) [17] [20] |
The drive for more sensitive and specific biosensors is fundamentally linked to the innovative use of materials. While traditional plasmonic metals like gold and silver remain the workhorses for signal generation, the data clearly demonstrates that hybrid configurations combining these metals with 2D materials (e.g., BK7/SiO₂/Cu/BaTiO₃) or perovskites yield superior performance [17]. The future of signal generation lies in this synergistic approach, where each material is selected to play a specific role—be it transduction, enhancement, or protection. Furthermore, the integration of these advanced material platforms with machine learning algorithms for data analysis is poised to push the boundaries of predictive accuracy and diagnostic reliability, paving the way for the next generation of point-of-care and clinical-grade biosensors [13].
Biosensor technology is undergoing a transformative evolution, driven by two parallel revolutions: the adoption of cell-free synthetic biology and the integration of artificial intelligence (AI) for data analysis and system optimization. Cell-free biosensors, which utilize biological machinery without maintaining living cells, offer advantages in stability, customization, and deployment in resource-limited settings [21]. Concurrently, AI and machine learning (ML) enhance biosensor capabilities by improving signal processing, pattern recognition, and predictive modeling, thereby boosting sensitivity, specificity, and reliability [22] [23]. This guide objectively compares the performance of these emerging systems, providing researchers and drug development professionals with a critical evaluation of their experimental performance, underlying mechanisms, and practical applications.
Performance Comparison of AI-Integrated and Cell-Free Biosensors
The convergence of cell-free biosensing and AI has led to significant advancements in detection capabilities. The table below provides a comparative overview of the performance of various biosensing systems as documented in recent experimental studies.
Table 1: Performance Comparison of Advanced Biosensing Systems
| Biosensor Type / Platform | Target Analyte | Detection Limit | Specificity / Key Feature | Experimental Data Source |
|---|---|---|---|---|
| Cell-Free (CRISPR-based) | Pathogens/Viral RNA | Single-base specificity | Ultrasensitive, programmable | [24] |
| Cell-Free (Plasmonic Coffee-Ring) | PSA (for cancer) | 3 pg/mL | Asymmetric plasmonic pattern, smartphone readout | [25] |
| Cell-Free (Plasmonic Coffee-Ring) | Procalcitonin (for sepsis) | <10 pg/mL (in saliva) | Detects sepsis-relevant levels in human saliva | [25] |
| Cell-Free (aTF-based) | Lead (Pb²⁺) | 0.1 nM (≈20.7 ppt) | High selectivity in real water samples | [21] |
| Cell-Free (Riboswitch-based) | Tetracyclines | 0.079 - 0.47 µM | Broad-spectrum detection in milk | [21] |
| AI-Enhanced Optical | Disease biomarkers | Enhanced over non-AI counterparts | Improved multiplexing, noise reduction | [22] [23] |
| AND-Gate Peptide (Cell-Free) | Protease Activity (Cancer) | N/A (Boolean logic) | Distinguishes treated vs. untreated tumors in vivo | [26] |
| ML-Predicted Electrochemical | Glucose | RMSE = 0.143 (Model) | Stacked ensemble ML for signal prediction | [27] |
Analysis of Comparative Data
The data reveals distinct trends. Cell-free biosensors consistently achieve remarkably low detection limits across diverse targets, from metals to proteins, making them suitable for early disease diagnosis and environmental monitoring [21] [25]. A key differentiator is their functional specificity, achieved through various mechanisms: allosteric transcription factors (aTFs) for metals, riboswitches for antibiotics, and Boolean logic (AND-gates) for complex cellular events [21] [26]. AI's primary role is performance enhancement, using models like deep neural networks to extract quantitative data from complex outputs (e.g., smartphone images) or to predict and optimize sensor responses, thereby improving accuracy and reliability [27] [25].
Experimental Protocols for Key Biosensing Platforms
Reproducibility is fundamental to biosensor research. Below are detailed methodologies for two representative and high-performance platforms.
Protocol: Plasmonic Coffee-Ring Biosensor for Ultra-Sensitive Protein Detection
This protocol details the procedure for detecting low-abundance proteins like Procalcitonin (PCT) or Prostate-Specific Antigen (PSA) using a coffee-ring effect-based pre-concentration and plasmonic signal generation [25].
Primary Materials:
- Thermally treated nanofibrous membrane: Serves as the substrate for droplet evaporation.
- Protein sample: Prepared in a suitable buffer (e.g., 5 µL volume).
- Plasmonic droplet: Contains gold nanoshells (GNShs) functionalized with specific antibodies (e.g., 2 µL volume).
- Smartphone with camera: For image capture of the final pattern.
Step-by-Step Procedure:
- Sample Deposition and Pre-concentration: Pipette a 5 µL sample droplet onto the right side of the nanofibrous membrane. Allow it to dry completely at room temperature. During evaporation, the coffee-ring effect pre-concentrates the target proteins at the edge of the droplet.
- Plasmonic Signal Generation: Pipette a 2 µL droplet of functionalized GNShs onto the left side of the dried first droplet, ensuring a partial overlap. Allow this second droplet to dry completely.
- Pattern Formation: The evaporation-induced flow of the second droplet carries GNShs over the pre-concentrated protein coffee-ring. Specific antibody-protein interactions cause GNShs to form a dispersed 2D pattern in the overlap zone, while nonspecific aggregation occurs elsewhere, creating a visible asymmetric pattern.
- Data Acquisition and Analysis: Capture an image of the asymmetric plasmonic pattern using a smartphone. Analyze the image using a trained deep neural network (e.g., integrating generative and convolutional networks) to correlate the pattern with biomarker concentration quantitatively.
Protocol: AND-Gate Protease Biosensor for In Vivo Cancer Monitoring
This protocol outlines the application of a cell-free, nanoparticle-based biosensor that uses Boolean logic to detect specific protease activities associated with tumor cell death [26].
Primary Materials:
- Cyclic peptide-based nanosensors: Composed of iron oxide nanoparticles and engineered cyclic peptides that are substrates for both granzyme B (from immune cells) and matrix metalloproteinase (from cancer cells).
- Animal model: Mice with established tumors.
Step-by-Step Procedure:
- Sensor Administration: Intravenously inject the cyclic peptide-based nanosensors into the animal model.
- In Vivo Activation: The nanosensors circulate and accumulate in the tumor microenvironment. The sensor signal is activated only upon the simultaneous presence and cleavage by both granzyme B and matrix metalloproteinase (AND-gate logic). This dual-protease requirement ensures high specificity for immune activity against tumors.
- Signal Detection and Readout: Monitor the activated sensor signal using an appropriate in vivo imaging modality. The signal intensity correlates with the degree of immune-mediated tumor cell killing.
- Validation: Correlate the sensor signal with treatment efficacy, such as distinguishing between tumors that respond to immune checkpoint blockade therapy from those that are resistant.
Signaling Pathways and Experimental Workflows
The following diagrams illustrate the core operational logic of two advanced biosensor types, highlighting the integration of biological components and computational analysis.
AND-gate Biosensor Logic
Diagram 1: AND-gate Biosensor Logic. This diagram illustrates the Boolean logic required for signal activation in advanced biosensors like the protease-activated nanosensor. The biosensor (center) only produces a readable output when both required input proteases are present and active [26].
AI-integrated Biosensing Workflow
Diagram 2: AI-integrated Biosensing Workflow. This workflow shows how raw data from a biosensor is processed by AI/ML algorithms to generate an enhanced, more reliable output. Key applications of AI in this process include complex pattern recognition (e.g., from smartphone images), signal noise filtration, and quantitative analyte prediction [22] [23] [25].
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and deployment of advanced biosensors rely on a core set of biological and synthetic components.
Table 2: Key Research Reagent Solutions for Advanced Biosensing
| Reagent / Material | Function in Biosensing | Example Application |
|---|---|---|
| Allosteric Transcription Factors (aTFs) | Biological recognition element that changes structure upon binding a target analyte, triggering a signal. | Detection of heavy metals (e.g., Hg²⁺, Pb²⁺) in water [21]. |
| CRISPR-Cas Systems | Provides ultra-specific nucleic acid recognition and can be coupled to signal amplification. | Precision detection of pathogen DNA/RNA with single-base specificity [24]. |
| Riboswitches / RNA Aptamers | Synthetic RNA sequences that bind to a target molecule, regulating reporter gene expression. | Detection of small molecules like tetracycline antibiotics in food samples [21]. |
| Gold Nanoshells (GNShs) | Plasmonic nanoparticles that undergo visible aggregation or color change upon binding events. | Signal generation in ultra-sensitive protein detection platforms [25]. |
| Cyclic Peptides | Engineered synthetic molecules that can be designed as substrates for specific proteases. | Core sensing element in AND-gate logic biosensors for in vivo monitoring [26]. |
| Cell-Free Protein Synthesis (CFPS) Systems | Purified cellular machinery that enables protein expression without whole cells, allowing for tunable reactions. | The core reaction environment for many cell-free biosensors; enables production of reporter proteins [21]. |
| Nanofibrous Membranes | Porous substrate that facilitates controlled droplet evaporation and pre-concentration of analytes. | Used to create the coffee-ring effect for signal enhancement [25]. |
Advanced Sensing Modalities and Their Application in Biomedical Research
Optical biosensors have revolutionized the field of biomarker detection by enabling label-free, real-time analysis of molecular interactions. Among the most prominent technologies are Surface Plasmon Resonance (SPR), Photonic Crystal Fiber-SPR (PCF-SPR), and Surface-Enhanced Raman Spectroscopy (SERS), each offering distinct mechanisms and advantages for scientific research and drug development. SPR biosensors detect refractive index changes at a metal-dielectric interface, while PCF-SPR incorporates microstructured fibers to enhance light-matter interaction and sensitivity [28] [29]. SERS utilizes plasmonic nanostructures to amplify Raman scattering signals by several orders of magnitude, enabling single-molecule detection in some configurations. These platforms have become indispensable tools for researchers studying biomolecular interactions, disease mechanisms, and therapeutic candidate screening, particularly as the demand for high-sensitivity, point-of-care diagnostic technologies continues to grow [28] [30].
The evaluation of biosensor performance relies on several key parameters. Sensitivity quantifies the detectable change in signal per unit change in analyte concentration or refractive index, often reported as nm/RIU (refractive index unit) for wavelength-based detection or RIU⁻¹ for amplitude-based detection [29]. Specificity refers to the sensor's ability to distinguish target analytes from similar molecules in complex biological samples. Figure of Merit (FOM) combines sensitivity and resonance sharpness to provide a comprehensive performance metric, while resolution indicates the smallest detectable refractive index change [31] [29]. This guide provides an objective comparison of these three biosensing platforms, supported by experimental data and methodologies from recent research advances.
The following table summarizes the fundamental characteristics, operating principles, and typical applications of each biosensing platform:
Table 1: Fundamental Characteristics of Optical Biosensing Platforms
| Parameter | SPR | PCF-SPR | SERS |
|---|---|---|---|
| Detection Principle | Refractive index change at metal-dielectric interface [29] | Enhanced light-matter interaction in microstructured fibers [28] [29] | Raman signal amplification via plasmonic nanostructures |
| Key Materials | Gold, silver with dielectric layers (e.g., ZnO, Si₃N₄) [30] | Gold, silver, novel plasmonic materials (ZrN, TMDCs) [29] [32] | Gold, silver nanoparticles, nanostructured substrates |
| Typical Applications | Biomolecular interaction analysis, kinetic studies [28] | Cancer detection, environmental monitoring, chemical sensing [28] [29] | Pathogen detection, chemical imaging, single-molecule spectroscopy |
| Label-Free | Yes | Yes | Yes (indirect enhancement) |
| Throughput | Moderate | High (multi-analyte potential) | High (multiplexing capability) |
Recent advances in PCF-SPR sensors have demonstrated remarkable performance improvements through innovative design strategies. The bowtie-shaped PCF-SPR biosensor achieves a wavelength sensitivity of 143,000 nm/RIU and amplitude sensitivity of 6,242 RIU⁻¹ across a broad refractive index range (1.32-1.44) [31]. Machine learning-optimized PCF-SPR designs report similarly high performance with 125,000 nm/RIU wavelength sensitivity and 2,112.15 FOM [33] [10]. Comparative studies show that PCF-SPR sensors consistently outperform conventional SPR platforms in sensitivity metrics while offering greater design flexibility and miniaturization potential [28] [29].
Quantitative Performance Comparison
The table below summarizes experimental performance data for various biosensor configurations reported in recent literature:
Table 2: Experimental Performance Metrics of Recent Biosensor Designs
| Sensor Type | Configuration/Materials | Sensitivity | FOM | Resolution (RIU) | Detection Range (RIU) | Reference |
|---|---|---|---|---|---|---|
| PCF-SPR | Bowtie-shaped, Gold | 143,000 nm/RIU (WS), 6,242 RIU⁻¹ (AS) | 2,600 | 6.99×10⁻⁷ | 1.32-1.44 | [31] |
| PCF-SPR | ML-optimized, Gold | 125,000 nm/RIU (WS), -1,422.34 RIU⁻¹ (AS) | 2,112.15 | 8×10⁻⁷ | 1.31-1.42 | [33] [10] |
| SPR | BK7/ZnO/Ag/Si₃N₄/WS₂ | 342.14 deg/RIU | 124.86 | N/R | 1.33-1.40 | [30] |
| PCF-SPR | V-shaped, ZrN | 6,214.28 nm/RIU (TM, breast cancer) | N/R | N/R | 1.39-1.41 | [32] |
| PCF-SPR | Cylindrical vector modes, Gold | 13,800 nm/RIU (WS), 2,380 RIU⁻¹ (AS) | N/R | ~10⁻⁶ | 1.29-1.34 | [34] |
WS: Wavelength Sensitivity; AS: Amplitude Sensitivity; N/R: Not Reported
For cancer detection applications, SPR biosensors with specialized architectures have demonstrated remarkable capabilities. A layered structure incorporating WS₂ (BK7/ZnO/Ag/Si₃N₄/WS₂/sensing medium) achieved sensitivity of 342.14 deg/RIU and FOM of 124.86 RIU⁻¹ for blood cancer (Jurkat) detection, outperforming other configurations for cervical cancer (HeLa) and skin cancer (Basal) detection [30]. The integration of transition metal dichalcogenides (TMDCs) like MoS₂, MoSe₂, WS₂, and WSe₂ has proven particularly effective for enhancing sensitivity in cancer biomarker detection [30].
Experimental Protocols and Methodologies
Sensor Design and Optimization Protocols
Finite Element Method (FEM) Simulation: Researchers typically employ COMSOL Multiphysics or similar platforms to model sensor architectures [31] [34]. The process involves creating a geometric model of the proposed sensor, defining material properties (including wavelength-dependent refractive indices for metals using Drude-Lorentz model and for silica using Sellmeier equation), applying appropriate boundary conditions (Perfectly Matched Layer, PML, for radiation absorption), and performing mesh convergence analysis to ensure numerical accuracy [31] [34]. For PCF-SPR sensors, key parameters including pitch (Λ), air hole diameters (d₁, d₂, d₃), plasmonic layer thickness (t_g), and core-to-metal distance are systematically varied to optimize performance metrics [31].
Machine Learning Optimization: Recent approaches integrate ML algorithms to accelerate sensor optimization [33] [10]. The standard protocol involves: (1) generating comprehensive datasets through parametric sweeps using FEM simulations; (2) training multiple regression models (Random Forest, Gradient Boosting, etc.) to predict optical properties based on design parameters; (3) applying explainable AI (XAI) methods like SHAP analysis to identify critical design parameters; and (4) iteratively refining designs based on ML predictions to maximize sensitivity and FOM while minimizing confinement loss [33] [10]. This approach significantly reduces computational costs compared to traditional optimization methods.
Performance Characterization Methodology
Sensitivity Measurement: For wavelength interrogation, researchers track the resonance wavelength shift (Δλ) corresponding to variations in analyte refractive index (Δna), calculating wavelength sensitivity as Sλ = Δλ/Δna (nm/RIU) [29]. For amplitude interrogation, sensitivity is calculated as SA = (1/α(λ)) × (∂α(λ)/∂n_a) (RIU⁻¹), where α(λ) represents transmission loss [29] [34]. Measurements are typically performed across the target refractive index range (e.g., 1.31-1.44 for biological analytes) with incremental steps of 0.01-0.03 RIU [31].
Figure of Merit and Resolution Calculation: FOM is determined as the ratio of wavelength sensitivity to the full width at half maximum (FWHM) of the resonance peak: FOM = Sλ/FWHM (RIU⁻¹) [31]. Sensor resolution represents the smallest detectable refractive index change and is calculated as R = Δna × (Δλmin/Δλ), where Δλmin is the minimum resolvable wavelength shift (typically 0.1 nm for standard spectrometers) [31].
Figure 1: PCF-SPR Experimental Setup and Sensing Mechanism
Operational Principles and Signaling Pathways
The fundamental operating principle of SPR and PCF-SPR biosensors relies on the excitation of surface plasmon polaritons (SPPs) at the metal-dielectric interface [29]. When incident light strikes the metal surface under total internal reflection conditions, it generates an evanescent field that penetrates the dielectric medium. At a specific resonance wavelength or angle, the wave vector of the incident light matches that of the surface plasmons, resulting in resonant energy transfer and a sharp dip in the reflected or transmitted light spectrum [29] [34]. This resonance condition is extremely sensitive to changes in the local refractive index at the metal surface, enabling detection of biomolecular binding events in real-time without labels.
In PCF-SPR sensors, the photonic crystal fiber provides enhanced light confinement and flexible design options to optimize plasmonic excitation [28] [29]. The microstructured air holes can be arranged in various configurations (hexagonal, bowtie, V-shaped, etc.) to control light propagation characteristics and maximize overlap between the guided mode and analyte medium [31] [32]. The strategic placement of plasmonic materials (external coating, internal deposition, or selective infiltration) further enhances the coupling efficiency between core-guided modes and surface plasmon modes [29].
Figure 2: Biosensing Principle and Signal Transduction Pathway
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Optical Biosensors
| Category | Specific Materials | Research Function | Performance Considerations |
|---|---|---|---|
| Plasmonic Materials | Gold (Au), Silver (Ag), Zirconium Nitride (ZrN) [29] [32] | Generate surface plasmon waves for signal transduction | Au: High stability, strong resonance; Ag: Sharper resonance but oxidation-prone; ZrN: High melting point, CMOS compatibility [32] |
| 2D Enhancement Materials | Graphene, TMDCs (MoS₂, WS₂), Black Phosphorus [28] [30] | Enhance light-matter interaction, protect metallic layers, provide binding sites | TMDCs: Strong field confinement, biocompatibility; Graphene: High adsorption for biomolecules [30] |
| Dielectric Layers | ZnO, Si₃N₄, TiO₂, SiO₂ [30] [32] | Adhesion layers, optical coupling, surface functionalization | ZnO: Enhances electric field; Si₃N₄: Improved sensitivity and FOM [30] |
| Computational Tools | COMSOL Multiphysics, MATLAB, Python ML libraries [33] [31] | Sensor design, simulation, data analysis, optimization | FEM: Accurate electromagnetic modeling; ML: Rapid design optimization and prediction [33] [10] |
| Substrate Materials | BK7 prism, Silica (SiO₂), Photonic Crystal Fibers [30] [29] | Light coupling, structural foundation, guidance mechanism | PCFs: Flexible design, enhanced light confinement; Prism: Conventional SPR coupling [29] |
The comparative analysis of SPR, PCF-SPR, and SERS platforms reveals a dynamic landscape of optical biosensing technologies with distinct advantages for different research applications. Conventional SPR systems offer well-established operation and reliability for biomolecular interaction analysis, while PCF-SPR platforms provide superior sensitivity and design flexibility through microstructured fiber optics. SERS delivers exceptional molecular fingerprinting capability through Raman signal enhancement.
Future research directions focus on addressing current limitations including fabrication complexity, detection range constraints, and material costs [28]. The integration of machine learning and artificial intelligence for sensor optimization and data analysis represents a promising avenue for enhancing detection efficiency and accuracy [28] [33] [10]. Additionally, the development of novel plasmonic materials, multi-analyte detection capabilities, and point-of-care miniaturization will further expand the applications of these powerful biosensing platforms in biomedical research, clinical diagnostics, and drug development [28] [29]. As these technologies continue to evolve, they will play an increasingly crucial role in advancing personalized medicine and improving healthcare outcomes through sensitive, specific, and rapid biomarker detection.
Electrochemical biosensors have emerged as powerful tools in modern healthcare, enabling the sensitive and specific detection of metabolites and disease-associated biomarkers. These sensors function by incorporating a biological recognition element, such as an enzyme or antibody, in direct spatial contact with an electrochemical transducer, which converts a biological reaction into a quantifiable electrical signal such as current or potential [35]. This operational principle allows for the rapid, cost-effective, and highly sensitive analysis of target analytes in complex biological matrices like blood, sweat, and saliva [36].
The focus of biosensor research has increasingly shifted towards achieving ultra-high sensitivity and specificity, which are critical for the early diagnosis of diseases where biomarkers are present at ultralow concentrations [36]. Recent innovations have been fueled by the integration of advanced nanomaterials, novel transducer designs, and the development of wearable and point-of-care (POC) devices. These advancements are systematically overcoming traditional limitations of electrochemical sensors, such as signal instability and insufficient sensitivity for macromolecular biomarkers, paving the way for their broader clinical and commercial application [35] [37].
Performance Comparison: Sensor Platforms for Metabolites and Protein Biomarkers
The performance of electrochemical biosensors varies significantly based on their design, the biomarker target, and the materials used for electrode modification. The tables below provide a comparative analysis of documented sensor performances for key metabolite and clinical protein biomarkers.
Table 1: Performance comparison of electrochemical sensors for metabolite detection.
| Target Analyte | Associated Condition | Sensor Type / Recognition Element | Linear Range | Limit of Detection (LOD) | Year |
|---|---|---|---|---|---|
| Glucose | Diabetes Mellitus | Enzymatic (e.g., Glucose Oxidase) | Not Specified | 0.159 μM | 2021 |
| Glucose | Diabetes Mellitus | Enzymatic | Not Specified | 3.35 μM | 2021 |
| Lactate | Diabetes Mellitus | Enzymatic (e.g., Lactate Oxidase) | Not Specified | 0.41 mM | 2021 |
| Urea | Diabetes Mellitus | Enzymatic | Not Specified | 0.14 nM | 2020 |
| Dopamine | Parkinson's Disease | Affinity-based | Not Specified | 10 pM | 2021 |
| Dopamine | Alzheimer's Disease | Affinity-based | Not Specified | 8.75 pM | 2020 |
| H₂O₂ | Neurodegenerative Disease | Catalytic Material | Not Specified | 0.02 μM | 2020 |
| Branched-Chain Amino Acids | Metabolic Syndrome | Wearable Molecularly Imprinted Polymer [38] | Not Specified | Trace levels in sweat [38] | 2022 |
Table 2: Performance comparison of electrochemical immunosensors for protein biomarkers.
| Target Analyte | Associated Condition | Sensor Design | Linear Range | Limit of Detection (LOD) | Year |
|---|---|---|---|---|---|
| α-Fetoprotein (AFP) | Liver Cancer | Au@Pd NPs, MoS₂@MWCNTs [37] | Not Specified | 3.57 pM (≈0.60 ng/mL)* | 2009 |
| α-Fetoprotein (AFP) | Liver Cancer | Cu-Ag NPs, Polydopamine [37] | Not Specified | 4.27 pg/mL | Recent |
| Prostate-Specific Antigen (PSA) | Prostate Cancer | Immunosensor | Not Specified | 29.4 pM | 2017 |
| CYFRA 21-1 | Lung Cancer | Immunosensor | Not Specified | 57.5 fM | 2016 |
| Amyloid-β Oligomer | Alzheimer's Disease | Immunosensor | Not Specified | 1.0 aM (atto-molar) | 2020 |
| t-Tau | Alzheimer's Disease | Immunosensor | Not Specified | 1.59 fM | 2020 |
Note: Calculated using molecular weight of AFP (~67 kDa).
Experimental Protocols: Methodologies for High-Performance Sensing
Protocol for a Nanomaterial-Enhanced Immunosensor
The high sensitivity required for detecting low-abundance protein biomarkers, such as Alpha-fetoprotein (AFP), is often achieved through sophisticated nanomaterial-based electrode modifications. The following protocol, derived from recent research, outlines a representative methodology [37].
- 1. Electrode Substrate Preparation: A glassy carbon electrode (GCE) is typically polished to a mirror finish with alumina slurry, followed by sequential sonication in ethanol and deionized water to create a clean, reproducible surface.
- 2. Synthesis of Composite Nanomaterial: Polydopamine (PDA)-modified cellulose nanofibers (CNFs) are synthesized. Subsequently, bimetallic Cu-Ag nanoparticles (NPs) are deposited onto the PDA/CNF substrate. The PDA provides a universal adhesion layer and a platform for nanoparticle reduction and anchoring.
- 3. Electrode Modification: The synthesized nanocomposite (e.g., Cu-Ag/PDA/CNF) is dispersed in a solvent like ethanol and drop-cast onto the cleaned GCE surface, followed by drying.
- 4. Antibody Immobilization: A capture antibody (e.g., anti-AFP) is immobilized onto the modified electrode surface. This can be achieved through cross-linkers like glutaraldehyde or via direct adsorption facilitated by the nanomaterial's high surface area and biocompatibility.
- 5. Immunoassay Procedure: The functionalized electrode is incubated with the sample containing the target antigen (AFP). In a sandwich-type assay, a secondary antibody (Ab2), which is often conjugated with a signal-amplifying label (e.g., enzymatic or nanoparticle-based), is added. The specific binding of the antigen creates an immunocomplex on the electrode.
- 6. Electrochemical Measurement: The electrocatalytic activity of the Cu-Ag NPs is utilized for signal transduction. The electrode is placed in a solution containing H₂O₂, and the reduction current of H₂O₂, which is catalyzed by the NPs and whose magnitude is proportional to the amount of captured immunocomplex, is measured using techniques like amperometry or chronoamperometry. The decrease in current upon the formation of the insulating immunocomplex can also be monitored in some label-free setups.
Protocol for a Wearable Metabolite Sensor
For continuous monitoring of metabolites like amino acids and vitamins in sweat, wearable sensors employ a different set of protocols, as exemplified by a reported graphene-based platform [38].
- 1. Sensor Fabrication: Graphene electrodes are fabricated on a flexible substrate. These electrodes are functionalized with metabolite-specific molecularly imprinted polymers (MIPs), which act as synthetic, antibody-like recognition elements. Redox-active reporter nanoparticles are integrated into the MIP matrix.
- 2. System Integration: The functionalized sensor is integrated with a wearable platform that includes modules for sweat induction (e.g., iontophoresis), microfluidic sweat sampling, signal processing, calibration, and wireless data transmission.
- 3. On-Body Operation and Sensing: The wearable device is applied to the skin. Iontophoresis induces sweat, which is channeled through the microfluidic system to the sensor array. Binding of the target metabolite to the MIPs causes a change in the electrochemical signal (e.g., in the voltammetric peak of the reporter nanoparticles), which is measured and wirelessly transmitted.
- 4. In-situ Regeneration: A key feature of this platform is its ability to be regenerated in situ. A low-pH elution buffer is delivered via the integrated microfluidics to disrupt the metabolite-MIP binding, refreshing the sensor for subsequent measurements.
Diagram 1: Workflow of a wearable metabolite sensor with in-situ regeneration.
Signaling Pathways and Sensor Operational Logic
The core functionality of electrochemical biosensors relies on specific signaling pathways and logical operational principles. The diagram below illustrates the general signaling pathway for an electrochemical immunosensor and the logical flow of a machine learning-enhanced optimization process, which is increasingly used to improve sensor performance [27].
Diagram 2: Signaling pathway for a label-free electrochemical immunosensor.
Diagram 3: Logic of machine learning-driven biosensor optimization.
The Scientist's Toolkit: Essential Research Reagents and Materials
The development of high-performance electrochemical sensors relies on a specific toolkit of materials and reagents. The table below details key components and their functions in sensor fabrication.
Table 3: Key research reagents and materials for electrochemical biosensor development.
| Material/Reagent | Category | Primary Function in Sensor Development | Example Use Case |
|---|---|---|---|
| Gold Nanoparticles (Au NPs) | Zero-dimensional (0D) Nanomaterial [37] | Enhances electron transfer, provides high surface area for biomolecule immobilization, and can be used as an electrocatalyst or label [37]. | Functionalizing graphene oxide substrates to create highly sensitive immunosensors [37]. |
| Graphene & Derivatives | Carbon Nanomaterial | Provides excellent electrical conductivity, large specific surface area, and facilitates charge transfer. Used in substrates and wearable electrodes [38]. | Base material for flexible electrodes in wearable sweat sensors [38]. |
| Molecularly Imprinted Polymers (MIPs) | Plastic Antibody / Synthetic Receptor [37] | Provides synthetic, stable, and selective recognition sites for target molecules, serving as an antibody alternative [38]. | Recognition element for amino acids and vitamins in wearable sweat sensors [38]. |
| Glutaraldehyde | Crosslinking Agent | Creates covalent bonds to stably immobilize biomolecules (enzymes, antibodies) onto sensor surfaces. | Crosslinking glucose oxidase or antibodies to nanomaterial-modified electrodes. |
| Enzymes (e.g., GOx, Lactate Oxidase) | Biological Recognition Element | Provides high specificity for the catalytic conversion of a target metabolite, generating an electroactive product (e.g., H₂O₂) [35]. | Key component in amperometric glucose and lactate sensors [36]. |
| Monoclonal Antibodies | Biological Recognition Element | Provides high specificity and affinity for protein biomarkers (antigens) via immunoreaction, forming the basis of immunosensors [37]. | Capture and detection antibody in a sandwich assay for Alpha-fetoprotein (AFP) [37]. |
| Electroactive Reporters (e.g., Methylene Blue) | Redox Probe | Acts as a signaling molecule; changes in its electrochemical behavior (e.g., peak current) indicate the binding of a target analyte. | Used in aptamer-based sensors where binding-induced folding alters electron transfer. |
| Metal-Organic Frameworks (MOFs) | Porous Nanomaterial | Provides an ultra-high surface area for biomolecule loading, can enhance stability, and some exhibit catalytic activity. | Used to immobilize enzymes while maintaining their activity, improving sensor stability. |
Precision medicine aims to tailor medical treatment to the individual characteristics of each patient, and in oncology, this hinges on the ability to detect cancer-specific biomarkers with high sensitivity and specificity. Biosensor technology has emerged as a powerful platform for achieving this goal, enabling the rapid, accurate, and often non-detection of molecular signatures associated with different cancer types. The performance of these biosensors is critically dependent on their design, which dictates their analytical sensitivity, specificity, and overall utility in clinical decision-making. This guide provides a comparative evaluation of leading biosensor architectures, with a focused analysis on their application in detecting multiple cancer types and profiling protein interactions. We objectively compare the performance of surface plasmon resonance (SPR), photonic crystal fiber (PCF)-SPR, and microfluidic-integrated biosensors, presenting experimental data to illustrate their respective capabilities and limitations within the context of precision oncology.
Comparative Performance Analysis of Biosensing Platforms
The evolution of biosensor technology has yielded a diverse array of platforms, each with distinct operational principles and performance characteristics. The following comparative analysis synthesizes data from recent studies to provide a clear overview of their capabilities in multi-cancer detection.
Table 1: Comparative Performance of Biosensor Platforms in Cancer Detection
| Biosensor Platform | Key Materials / Configuration | Detection Method | Cancer Types Detected | Reported Sensitivity | Specificity / FOM |
|---|---|---|---|---|---|
| Prism-based SPR [30] | BK7/ZnO/Ag/Si3N4/WS2 | Angular Interrogation | Blood (Jurkat), Cervical (HeLa), Skin (Basal) | 342.14 deg/RIU (Jurkat) | FOM: 124.86 RIU⁻¹ (Jurkat) |
| D-Shaped PCF-SPR [39] | Gold/TiO₂ on silica PCF | Wavelength Interrogation | Basal, HeLa, Jurkat, PC-12, MDA-MB-231 | 42,000 nm/RIU | FOM: 1393.128 RIU⁻¹ |
| Electrochemical Microfluidic [40] | Gold Nanoparticles, Graphene, CNTs | Electrochemical Signal | Various (via biomarkers like ctDNA, proteins) | Enhanced for low-concentration biomarkers | High Selectivity |
| Multi-Cancer Detection (MCD) Tests [41] | cfDNA mutation analysis & protein biomarkers | Blood-based Liquid Biopsy | Ovarian, Liver, Esophageal, Pancreatic, Stomach, Colorectal, Lung, Breast | 62.3% (overall), 49.9% (Stage I), 70.2% (Stage III) | 99.1% |
The data reveals a clear performance trade-off between different sensing principles. The D-Shaped PCF-SPR sensor demonstrates exceptionally high wavelength sensitivity and the highest Figure of Merit (FOM), which is a composite metric reflecting overall sensor quality [39]. This is attributed to its optimized Gold/TiO₂ layers and the efficient light-analyte interaction within the PCF structure. In contrast, the conventional prism-based SPR sensor, while highly sensitive in angular interrogation units, operates on a different scale but is notable for its direct comparison of multiple two-dimensional materials, identifying WS₂ as the most effective for sensitivity enhancement [30].
Meanwhile, blood-based MCD tests like CancerSEEK represent a different class of technology, reporting performance in clinical terms of sensitivity and specificity for detecting a cancer signal from a panel of biomarkers [41]. Their strength lies in the ability to screen for multiple cancers concurrently from a single, non-invasive blood draw, though their sensitivity is currently highest for later-stage cancers.
Detailed Experimental Protocols and Methodologies
Protocol for Prism-Based SPR Biosensing
The experimental setup and methodology for conventional SPR biosensors, as used for cancer cell detection, typically involves the following steps [30]:
- Sensor Chip Functionalization: A BK7 prism is coated with successive layers of ZnO, Ag, Si3N4, and a 2D material (e.g., WS₂) to form the sensing interface. The architecture (e.g., BK7/ZnO/Ag/Si3N4/WS₂) is designed to enhance the electromagnetic field and light absorption.
- Baseline Establishment: A polarized light source is directed through the prism to excite surface plasmons in the metal layer. The reflected light is measured with a detector, establishing a baseline resonance angle (or curve) using a buffer solution.
- Analyte Introduction: A solution containing the target cancer cells (e.g., Jurkat for blood cancer, HeLa for cervical cancer) is flowed over the sensor surface.
- Real-Time Monitoring: The binding of cancer cells to the sensing surface causes a local change in the refractive index. This shift is detected in real-time as a change in the resonance angle.
- Data Analysis: The angular shift (in degrees/RIU) is quantified and correlated to the concentration of bound cells. The sensitivity is calculated from this shift, and the Full Width at Half Maximum (FWHM) of the resonance curve is used to calculate the Figure of Merit (FOM = Sensitivity / FWHM).
Protocol for D-Shaped PCF-SPR Biosensing
The methodology for PCF-based sensors differs significantly due to the fiber-optic platform [39]:
- Fabrication and Coating: A D-shaped photonic crystal fiber is fabricated, and its flat surface is polished. This surface is then coated with a uniform layer of gold, followed by a layer of TiO₂.
- Optical Setup: A broadband light source (visible to near-infrared) is launched into one end of the PCF. An analyte (e.g., a solution simulating cancer cell cytoplasm) is brought into contact with the metal-coated surface of the PCF.
- Spectral Analysis: The output light from the other end of the PCF is captured by an optical spectrum analyzer. The excitation of surface plasmons at the metal-analyte interface causes a characteristic loss band in the transmission spectrum.
- Refractive Index Perturbation: As the refractive index of the analyte changes (due to the presence of different cancer cell types or concentrations), the wavelength of this loss peak shifts.
- Sensitivity Calculation: The wavelength sensitivity (WS) is calculated as the shift in the resonance wavelength (in nanometers) per unit change in the refractive index (RIU), expressed as nm/RIU. The amplitude sensitivity (AS) and FOM are also derived from the spectral data.
<100 chars: D-Shaped PCF-SPR Workflow
Signaling Pathways and Molecular Interactions in Cancer Biosensing
Biosensors detect cancer by interacting with specific biomolecules and pathways that are deregulated in cancer cells. SPR and other label-free sensors typically detect these interactions directly through mass or refractive index changes.
<100 chars: Cancer Biomarker Detection Pathway
The fundamental principle involves the specific binding of target biomarkers present in or on cancer cells to recognition elements (e.g., antibodies, aptamers) immobilized on the sensor surface [30] [40]. For instance:
- Protein Interaction Analysis: Sensors can be functionalized with antibodies against cancer-specific proteins (e.g., CA15-3 for breast cancer [30] or CYFRA 21-1 for esophageal cancer [42]). The binding kinetics and affinity can be analyzed in real-time using SPR.
- Nucleic Acid Detection: For mutations in genes like BRCA1, BRCA2, or TP53, the sensor surface is coated with complementary DNA probes. The hybridization of target ctDNA from liquid biopsies is detected [30] [41].
- Whole Cell Detection: The sensor can be designed to capture entire cancer cells (e.g., Jurkat, HeLa) by targeting unique surface antigens, with the resulting bulk refractive index change being measured [30] [39].
The Scientist's Toolkit: Essential Research Reagents and Materials
The performance of advanced biosensors is critically dependent on the materials and reagents used in their fabrication and operation. The table below details key components referenced in the studies.
Table 2: Key Research Reagents and Materials for Biosensor Development
| Material / Reagent | Function in Biosensor | Application Example |
|---|---|---|
| Gold (Au) & Silver (Ag) [30] [39] | Plasmonic metal layer; generates surface plasmons for signal transduction. | Standard in SPR and PCF-SPR sensors. Gold preferred for chemical stability. |
| Transition Metal Dichalcogenides (WS₂, MoS₂) [30] | 2D material overlayer; enhances light-matter interaction and sensitivity. | Used in BK7/ZnO/Ag/Si3N4/WS₂ configuration for cancer cell detection. |
| Titanium Dioxide (TiO₂) [39] | Dielectric overlayer; enhances sensitivity and coupling efficiency in SPR. | Combined with gold in D-shaped PCF-SPR for high sensitivity (42,000 nm/RIU). |
| Graphene & Carbon Nanotubes (CNTs) [40] | Nanomaterial with high surface area and conductivity; enhances signal in electrochemical and optical sensors. | Integrated into microfluidic biosensors for capturing and detecting low-concentration biomarkers. |
| Zinc Oxide (ZnO) [30] | Interface layer; improves adhesion and performance of the plasmonic metal film. | Used as a layer between the BK7 prism and Ag layer in SPR configurations. |
| Specific Antibodies & DNA Probes [30] [41] [40] | Biorecognition elements; provide specificity by binding to target biomarkers (proteins, ctDNA). | Anti-PSA for prostate cancer, probes for BRCA1/2 mutations, anti-HER2 for breast cancer. |
| Photonic Crystal Fiber (PCF) [39] | Waveguide platform; allows efficient light-analyte interaction in a compact, flexible format. | Base structure for D-shaped SPR sensors, enabling high-sensitivity, multi-analyte detection. |
The comparative data presented in this guide underscores the rapid advancement in biosensor technology for precision oncology. Platforms like the D-shaped PCF-SPR and 2D-material-enhanced SPR show remarkable analytical performance in terms of sensitivity and FOM, making them powerful research tools. Concurrently, the clinical translation of biosensor principles into blood-based MCD tests represents a significant stride toward population-level screening. The future of this field lies in the continued integration of technologies, such as combining microfluidics for sample handling with SPR or electrochemical detection for high sensitivity [40]. Furthermore, the incorporation of artificial intelligence and machine learning for data analysis is poised to enhance the ability of these biosensors to deconvolute complex signals, identify subtle patterns, and improve diagnostic accuracy, ultimately solidifying their role in the era of personalized cancer medicine.
Cell-free biosensors represent a transformative approach in analytical science, harnessing the core molecular machinery of cells for detection without the constraints of maintaining cell viability. These systems utilize purified cellular components—such as transcription and translation factors, ribosomes, and energy sources—to perform complex biochemical reactions in vitro, enabling highly sensitive and specific detection of diverse analytes [21]. By eliminating the cell membrane barrier and viability requirements, cell-free biosensors overcome significant limitations of traditional whole-cell biosensors, including slow response times, susceptibility to environmental stressors, and cell-wall transport inhibition [21] [43]. This technology has rapidly advanced through integration with synthetic biology, materials science, and microengineering, creating powerful platforms for addressing two critical global challenges: monitoring environmental toxins and enabling point-of-care diagnostics in resource-limited settings [21] [44].
The fundamental architecture of a cell-free biosensor consists of three essential components: (1) recognition elements that specifically interact with the target analyte (e.g., transcription factors, riboswitches, aptamers), (2) reporter systems that generate a measurable signal upon detection (e.g., fluorescent proteins, colorimetric enzymes, luciferase), and (3) signal analysis platforms that convert the biochemical signal into quantifiable data (e.g., smartphone detectors, portable fluorimeters, electrode systems) [43]. This modular design allows for extensive customization to detect targets ranging from heavy metals and organic pollutants to pathogen biomarkers and disease indicators [21]. Recent innovations have further enhanced their practicality through lyophilization (freeze-drying) onto paper-based platforms, creating stable, shelf-ready tests that can be activated with simple rehydration [21]. As the field progresses, integration with digital health technologies, artificial intelligence, and Internet of Things (IoT) platforms is expanding the capabilities and applications of these sophisticated biosensing systems [44] [45].
Performance Comparison: Cell-Free Versus Alternative Biosensing Platforms
Biosensors are categorized based on their biorecognition elements, each with distinct operational mechanisms, advantages, and limitations. The table below provides a comprehensive comparison of major biosensor types, highlighting the relative position of cell-free systems within the technological landscape.
Table 1: Comparative Analysis of Biosensor Platforms
| Biosensor Type | Recognition Element | Working Principle | Key Advantages | Inherent Limitations |
|---|---|---|---|---|
| Cell-Free Biosensors [21] [43] | Transcription factors, riboswitches, toehold switches | In vitro gene expression; target binding triggers synthesis of reporter proteins | High sensitivity & tunability; rapid response; no cell membrane barriers; works in toxic environments; easily lyophilized | Limited long-term stability; batch-to-batch variation in extracts; consumption of reagents |
| Enzyme-Based Biosensors [46] | Enzymes | Catalytic transformation, inhibition, or modulation of enzyme by analyte | High specificity and fast reaction kinetics | Susceptibility to denaturation; limited analyte scope (requires enzyme-specific substrate) |
| Antibody-Based Immunosensors [46] | Antibodies (Immunoglobulins) | High-affinity antigen-antibody binding (label-free or labeled) | Exceptional specificity and maturity of technology | High production cost; sensitivity to environmental conditions (pH, temperature) |
| Nucleic Acid-Based Aptasensors [46] [44] | DNA/RNA aptamers | Folding into 2D/3D structures for target binding via SELEX-derived aptamers | High stability; chemical synthesis; reusability | Susceptibility to nuclease degradation; complex SELEX process for aptamer development |
| Whole-Cell Biosensors [21] [46] | Microbial cells (bacteria, yeast) | Integrated cellular response (metabolic, stress, genetic circuits) | Self-replication; robust in varied conditions; can detect bioavailability | Slow response; strict viability requirements; hampered by cell walls; ethical concerns about GMO release |
To specifically evaluate detection capabilities, the following table summarizes the documented analytical performance of representative cell-free biosensors against key targets in environmental and potential diagnostic applications. The data demonstrates their capability to meet and exceed regulatory detection limits.
Table 2: Analytical Performance of Cell-Free Biosensors for Target Analytes
| Target Analyte | Biosensor Design / Recognition Element | Sample Matrix | Limit of Detection (LOD) | Detection Mechanism |
|---|---|---|---|---|
| Mercury (Hg²⁺) [21] | Paper-based, dual-filter, smartphone | Water | 6 μg/L | Colorimetric |
| Mercury (Hg²⁺) [21] | merR gene, plasmid DNA, luciferase/eGFP | Water | 1 ppb (∼ 5 nM) | Bioluminescence/Fluorescence |
| Mercury (Hg²⁺) [21] | Allosteric Transcription Factor (aTF) | Water | 0.5 nM | Colorimetric/Fluorescence |
| Lead (Pb²⁺) [21] | Allosteric Transcription Factor (aTF) | Water | 0.1 nM | Colorimetric/Fluorescence |
| Lead (Pb²⁺) [21] | Engineered PbrR mutants | Water | 50 nM | Not Specified |
| Arsenic & Mercury [21] | Optimized transcription factors | Water | As: ≤10 μg/L; Hg: ≤6 μg/L | Not Specified |
| Tetracyclines [21] | Riboswitch-based, RNA aptamers | Milk | 0.4 μM | Not Specified |
| Pathogens (e.g., B. anthracis) [21] | 16S rRNA targeting, retroreflective particles | Buffer | Femtomolar (fM) level | Optical (Retroreflection) |
Experimental Protocols in Cell-Free Biosensor Research
Core Workflow for aTF-Based Heavy Metal Detection
The following diagram illustrates the generalized experimental workflow for developing and deploying a biosensor using allosteric transcription factors (aTFs) for heavy metal detection, integrating steps from multiple research efforts [21] [43].
Diagram 1: aTF-Based Biosensor Workflow (97 characters)
Protocol Details:
Step 1: Genetic Circuit Assembly [21] [43]
- Objective: Clone a genetic construct where the promoter sequence, specifically controlled by a metal-responsive aTF (e.g., MerR for Hg²⁺ or PbrR for Pb²⁺), is placed upstream of a reporter gene.
- Methodology: The plasmid DNA is engineered to contain the aTF-specific operator/promoter region fused to a coding sequence for a reporter protein such as green fluorescent protein (eGFP), firefly luciferase, or the enzyme β-galactosidase (LacZ). This construct is then amplified and purified using standard molecular biology techniques.
Step 2: Cell-Free Extract Preparation [21] [43]
- Objective: Produce the active biochemical milieu necessary for in vitro transcription and translation.
- Methodology: A crude cellular extract is typically derived from E. coli strain BL21. Cells are cultured, harvested during log-phase growth, and lysed by sonication or French press. The lysate is centrifuged at high speed (e.g., 12,000-30,000 x g) to remove cell debris, and the supernatant is incubated in a run-off reaction to degrade endogenous mRNA. The extract is then dialyzed or buffer-exchanged to remove small molecules and is supplemented with essential components like amino acids, nucleotides, and an energy regeneration system (e.g., phosphoenolpyruvate with pyruvate kinase).
Step 3: Lyophilization [21]
- Objective: Stabilize the cell-free system for storage and portability.
- Methodology: The complete cell-free reaction mixture—containing the extract, genetic template, and supplements—is applied onto a porous matrix, commonly paper (e.g., cellulose or nitrocellulose). It is then flash-frozen and placed under vacuum for lyophilization (freeze-drying) to remove all water, resulting in a stable, dry biosensor pad.
Step 4: Sample Introduction & Reaction [21]
- Objective: Activate the biosensor and initiate the detection reaction.
- Methodology: In the field, the analyte-containing sample (e.g., a water sample) is applied to the lyophilized pad, rehydrating the system. If the target metal ion is present, it binds to the aTF, inducing a conformational change that activates transcription. This leads to the synthesis of the reporter protein. The reaction is typically incubated at a constant temperature (e.g., 30-37°C) for 30 to 120 minutes.
Step 5: Signal Measurement [21]
- Objective: Quantify the output signal to determine analyte concentration.
- Methodology: For colorimetric outputs (e.g., LacZ), a substrate like chlorophenol red-β-D-galactopyranoside (CPRG) is added, and the color change is quantified using a portable spectrophotometer or by analyzing an image captured with a smartphone. For fluorescent reporters (e.g., eGFP), signal intensity is measured with a portable fluorimeter. The signal is correlated with analyte concentration using a pre-established calibration curve.
Riboswitch-Based Antibiotic Detection Protocol
The mechanism for riboswitch-based detection, as used for tetracyclines, differs fundamentally from aTF-based methods and relies on direct RNA-analyte interaction.
Diagram 2: Riboswitch Detection Mechanism (95 characters)
Protocol Details [21]:
- Sensor Design: An RNA aptamer sequence with high affinity and specificity for a tetracycline antibiotic is fused to the expression platform of a riboswitch. In the absence of the target, the riboswitch adopts a conformation that inhibits the translation of a downstream reporter gene.
- Cell-Free Reaction: The DNA template encoding this riboswitch-reporter construct is added to the cell-free protein synthesis system.
- Detection Mechanism: Upon introduction of a sample containing tetracycline, the antibiotic binds directly to the aptamer domain. This binding event triggers a structural rearrangement (conformational change) in the riboswitch, which switches from the "OFF" state to the "ON" state. This change exposes the ribosome binding site (RBS), allowing translation to proceed and the reporter protein (e.g., a fluorescent protein) to be synthesized.
- Quantification: The resulting fluorescence intensity is directly proportional to the concentration of tetracycline in the sample. This system achieved detection limits as low as 0.079 μM for specific tetracyclines in spiked milk samples [21].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful development and deployment of cell-free biosensors rely on a suite of specialized reagents and materials. The following table catalogs key components referenced in the experimental protocols.
Table 3: Essential Research Reagents for Cell-Free Biosensor Development
| Reagent / Material | Function / Role | Specific Examples & Notes |
|---|---|---|
| Allosteric Transcription Factors (aTFs) [21] [43] | Recognition Element: Binds specific analyte, causing conformational change that modulates transcription. | MerR (for Hg²⁺), PbrR (for Pb²⁺), ArsR (for As³⁺). Can be engineered for improved sensitivity/range [21]. |
| Riboswitches / RNA Aptamers [21] [43] | Recognition Element: Synthetic RNA sequences that bind analyte, inducing structural changes to regulate translation. | Artificially screened tetracycline aptamers; fluoride-responsive riboswitches. Selected via SELEX [21]. |
| Cell-Free Protein Synthesis (CFPS) System [21] [43] | Reaction Environment: Provides essential machinery (ribosomes, tRNAs, factors) for in vitro transcription/translation. | Often homemade E. coli extracts (e.g., from BL21). Commercial kits (e.g., NEB PURExpress) also available. |
| Reporter Genes / Proteins [21] [43] | Signal Generation: Encoded protein produces measurable output upon successful detection event. | eGFP (fluorescence), Firefly Luciferase (bioluminescence), LacZ/β-galactosidase (colorimetric) [21]. |
| Paper-Based Matrix [21] [44] | Solid Support & Platform: Porous material for immobilizing and lyophilizing CFPS reactions; enables low-cost, portable form factor. | Cellulose, nitrocellulose filter paper. Facilitates capillary flow and easy sample application [21]. |
| Signal Detection Hardware [21] [47] | Signal Quantification: Instruments to convert biochemical signal into quantifiable data. | Portable fluorimeters, plate readers. Increasingly: smartphone cameras with custom apps for colorimetric analysis [21]. |
Cell-free biosensors represent a rapidly maturing technology with demonstrated efficacy in detecting environmental toxins and strong potential for point-of-care diagnostics. Quantitative performance data confirms their ability to achieve limits of detection that meet or exceed regulatory requirements for contaminants like heavy metals, with methodologies that offer distinct advantages in speed, portability, and operational flexibility compared to cell-based and other traditional biosensors. The experimental workflows, centered around synthetic genetic circuits and lyophilized reaction platforms, provide a reproducible framework for research and development. As the field progresses, the integration of these systems with advanced materials, digital health technologies, and AI-driven data analysis is poised to further enhance their sensitivity, specificity, and field-readiness, solidifying their role as essential tools for global health and environmental monitoring [21] [44] [45].
Enhancing Performance: Algorithmic and Material Strategies for Biosensor Optimization
The integration of machine learning (ML) with multi-objective particle swarm optimization (MOPSO) represents a paradigm shift in the computational design of high-performance biosensors. This guide provides a comparative analysis of this approach against traditional methods, demonstrating its superior capability to navigate complex design landscapes. By simultaneously optimizing multiple conflicting parameters such as sensitivity and specificity, ML-guided MOPSO enables the development of biosensors with enhanced performance metrics, reduced computational costs, and accelerated design cycles, thereby advancing biosensor research for medical diagnostics and drug development.
Computational design has become indispensable in modern biosensor development, particularly for applications requiring exquisite sensitivity and specificity in complex biological matrices. Traditional design methods, which often rely on sequential parameter optimization and intuitive design, struggle with the high-dimensional parameter spaces inherent in photonic and electrochemical biosensors. The emergence of machine learning (ML) coupled with multi-objective particle swarm optimization (MOPSO) addresses these limitations by enabling simultaneous optimization of multiple competing objectives. This approach is particularly valuable for surface plasmon resonance (SPR) biosensors, where parameters such as metal thickness, structural geometry, and material properties interact in complex, non-linear ways to determine overall sensor performance [48] [10].
For researchers in drug development and diagnostic sciences, these computational advances offer unprecedented opportunities to develop biosensors with enhanced detection capabilities for biomarkers, therapeutic antibodies, and pathogens. The ability to rapidly optimize sensor designs in silico before fabrication significantly reduces development timelines and costs while pushing the boundaries of detection limits. This article provides a comprehensive comparison of traditional and ML-enhanced approaches, supported by experimental data and detailed methodologies to guide researchers in selecting appropriate computational strategies for their specific biosensor development projects.
Comparative Analysis of Optimization Approaches
Traditional Single-Objective Optimization
Traditional biosensor optimization typically employs a one-variable-at-a-time approach, where parameters are sequentially adjusted while others remain fixed. This method is conceptually straightforward but suffers from significant limitations in identifying truly optimal designs, particularly when parameters exhibit complex interactions.
- Parameter Isolation: Each design parameter (e.g., gold thickness, polishing depth, air hole diameter) is optimized independently while keeping other parameters constant [48]
- Limited Design Exploration: The approach explores only a fraction of the possible design space, potentially missing regions where parameter interactions yield superior performance
- Single-Objective Focus: Traditional methods typically optimize for a single performance metric (e.g., sensitivity) without systematically considering trade-offs with other important characteristics (e.g., robustness or cost)
- Computational Inefficiency: Although individual simulations may be rapid, the need to exhaustively explore each parameter dimension can result in substantial cumulative computational time
In a conventional optimization of a D-shaped photonic crystal fiber (PCF) SPR sensor, researchers achieved a maximum sensitivity of 4,529.75 nm/RIU by sequentially adjusting d-factor, dc-factor, h-factor, and gold thickness [48]. While respectable, this performance represents only a local optimum within the constrained parameter space explored through the sequential methodology.
ML-Enhanced Multi-Objective PSO
Machine learning-enhanced multi-objective PSO represents a fundamentally different approach that leverages population-based search and predictive modeling to simultaneously explore and exploit the design space. This method explicitly addresses multiple, often competing, objectives to identify a Pareto-optimal front of solutions.
- Parallel Parameter Optimization: MOPSO simultaneously adjusts all design parameters across a population of candidate solutions, efficiently exploring parameter interactions [49] [50]
- Explicit Multi-Objective Handling: The approach identifies trade-offs between competing objectives (e.g., sensitivity vs. robustness) rather than converging to a single solution [51]
- ML-Guided Search: Machine learning models (e.g., Gaussian process regression, XGBoost) predict sensor performance, reducing the need for computationally expensive simulations [48] [49]
- Adaptive Search Behavior: MOPSO algorithms incorporate adaptive mechanisms that balance exploration of new design regions with exploitation of promising areas [50]
Application of NSGA-II (a MOPSO variant) to the D-shaped PCF SPR sensor increased sensitivity to 4,814.14 nm/RIU, representing a 6.28% improvement over traditional methods [48]. This performance gain demonstrates the advantage of simultaneous multi-parameter optimization in capturing complex parameter interactions that sequential methods miss.
Table 1: Performance Comparison of Optimization Approaches for D-Shaped PCF SPR Sensor
| Optimization Method | Maximum Sensitivity (nm/RIU) | Computational Efficiency | Key Advantages | Limitations |
|---|---|---|---|---|
| Traditional Sequential Optimization | 4,529.75 | Lower | Conceptual simplicity, straightforward implementation | Misses parameter interactions, local optima, single-objective focus |
| ML-Enhanced MOPSO (NSGA-II) | 4,814.14 | Higher | Captures parameter interactions, identifies Pareto fronts, global search capability | Increased algorithmic complexity, parameter tuning required |
Performance Benchmarking
The comparative performance of optimization approaches extends beyond a single sensor design. Across multiple biosensor platforms and performance metrics, ML-enhanced MOPSO consistently demonstrates advantages:
Table 2: Broad Performance Comparison Across Biosensor Types
| Biosensor Type | Optimization Method | Key Performance Metrics | Reference |
|---|---|---|---|
| D-shaped PCF SPR Refractive Index Sensor | Traditional Sequential | Sensitivity: 4,529.75 nm/RIU | [48] |
| D-shaped PCF SPR Refractive Index Sensor | NSGA-II with XGBoost | Sensitivity: 4,814.14 nm/RIU (6.28% improvement) | [48] |
| High-Sensitivity PCF-SPR Biosensor | ML with XAI | Sensitivity: 125,000 nm/RIU, Resolution: 8×10⁻⁷ RIU | [10] |
| Impedance-Based Biosensor | Geometric Optimization | Detection limit: 50 ng/mL for anti-SARS-CoV-2 mAb | [52] |
| Asphalt Mixture Proportion | GPR-AWMOPSO | Enhanced permanent deformation resistance, crack resistance, and moisture stability | [49] |
The performance advantages of ML-MOPSO approaches extend beyond sensitivity improvements. Researchers developing a PCF-SPR biosensor using ML and explainable AI (XAI) achieved a remarkable wavelength sensitivity of 125,000 nm/RIU with a resolution of 8×10⁻⁷ RIU, pushing the boundaries of what is achievable in label-free detection [10]. Similarly, in non-optical biosensors, geometric optimization of interdigitated electrodes (IDEs) for impedimetric detection enabled measurement of anti-SARS-CoV-2 monoclonal antibodies at concentrations as low as 50 ng/mL, with smaller electrode gaps (3μm) demonstrating superior sensitivity compared to larger gaps (4-5μm) [52].
Experimental Protocols and Methodologies
Data Generation for ML Training
The foundation of successful ML-MOPSO implementation is a comprehensive dataset for training predictive models. The following protocol outlines the standard approach for generating this data for optical biosensors:
Parameter Space Definition: Identify critical design parameters and their plausible ranges based on physical constraints and fabrication limitations. For PCF-SPR sensors, this typically includes pitch distance (Λ), air hole diameters (d, dc), polishing depth (h), and gold thickness (Au_th) [48] [10]
Design of Experiments: Employ sampling techniques (e.g., Latin Hypercube Sampling, Full Factorial Design) to generate representative parameter combinations across the design space. Sample size should balance computational cost with model accuracy requirements
Numerical Simulation: Utilize finite element method (FEM) simulations via platforms such as COMSOL Multiphysics or Lumerical to compute performance metrics for each parameter combination. Key outputs include effective refractive index (n_eff), confinement loss, and electric field distribution [48] [10]
Sensitivity Calculation: Derive wavelength sensitivity (Sλ) using the formula: Sλ = Δλ/Δna (nm/RIU), where Δλ is the resonance wavelength shift and Δna is the analyte refractive index change [10]
Data Validation: Implement cross-validation techniques to ensure simulation accuracy and physical plausibility of results
For a D-shaped PCF SPR sensor, researchers generated a dataset exploring d-factor (0.5-0.8), dc-factor (0.35-0.5), h-factor (0.6-0.9), and Au_th (45-65 nm) [48]. This comprehensive parameter sampling provided the foundation for accurate ML model training.
Machine Learning Model Development
With simulation data available, the next protocol involves developing predictive ML models:
Feature Selection: Identify the most influential design parameters using correlation analysis or domain knowledge. For PCF-SPR sensors, critical features typically include wavelength, analyte refractive index, gold thickness, and pitch [10]
Model Selection: Compare multiple regression algorithms to identify the best performer for the specific sensor design. Common candidates include:
Model Training: Split data into training and validation sets (typical ratio: 70-80% for training). Train models to predict sensor performance metrics (sensitivity, confinement loss) from design parameters
Hyperparameter Tuning: Optimize model-specific parameters using cross-validation techniques to prevent overfitting and maximize predictive accuracy
Model Evaluation: Assess performance using metrics such as R-squared (R²), mean squared error (MSE), and root mean square error (RMSE)
In developing a D-shaped PCF SPR sensor, researchers compared XGBoost, Random Forest, and PyTorch Neural Networks, finding XGBoost superior with R² = 0.9964 and MSE = 305.7 [48]. This high predictive accuracy enabled reliable optimization with reduced computational cost.
Multi-Objective PSO Implementation
The final protocol integrates trained ML models with MOPSO for design optimization:
Objective Definition: Formulate multiple, often competing, objectives. For biosensors, common objectives include:
Constraint Specification: Define design constraints based on physical principles and fabrication limitations, such as minimum feature sizes or material property limits
MOPSO Configuration:
- Initialize particle population with random positions and velocities within parameter bounds
- Define fitness function using trained ML models to evaluate objectives
- Implement non-dominated sorting to categorize solutions by Pareto dominance
- Apply crowding distance metrics to maintain solution diversity [51] [50]
Iterative Optimization:
- Update particle positions and velocities based on individual and global best solutions
- Update Pareto front with non-dominated solutions
- Maintain archive of best solutions using techniques like crowding distance sorting
- Continue until convergence criteria met (e.g., maximum iterations, solution stability)
Solution Selection: Present multiple Pareto-optimal solutions for final selection based on application-specific priorities
For sensor layout optimization in structural health monitoring, researchers enhanced MOPSO with initialization strategies, adaptive inertia weight, guided particle selection, and external candidate solution set maintenance, significantly improving optimization effectiveness [51].
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of ML-MOPSO for biosensor optimization requires both computational and experimental resources. The following table details essential research reagents and computational tools referenced in the literature:
Table 3: Essential Research Reagents and Computational Tools for Biosensor Optimization
| Category | Specific Resource | Function/Application | Representative Examples |
|---|---|---|---|
| Computational Tools | COMSOL Multiphysics | Finite Element Method (FEM) simulation for electromagnetic analysis | PCF-SPR sensor design optimization [10] |
| Python/R Libraries (XGBoost, Scikit-learn) | Machine learning model implementation and training | XGBoost for sensitivity prediction (R²=0.9964) [48] | |
| Custom MOPSO Algorithms | Multi-objective optimization implementation | NSGA-II for D-shaped PCF SPR sensor [48] | |
| Optical Biosensor Materials | Gold (Au) Thin Films | Plasmonic material for SPR excitation | Sputtering or CVD deposition on D-shaped fiber [48] |
| Photonic Crystal Fibers (PCF) | Sensor platform with design flexibility | D-shaped PCF with air hole patterns [48] [10] | |
| Monoclonal Antibodies | Bio-recognition elements for specific detection | Anti-SARS-CoV-2 spike protein antibodies [52] | |
| Experimental Validation | Refractive Index Standards | Calibration and sensitivity measurement | Glycerol solutions with known refractive indices [10] |
| Interdigitated Electrodes (IDEs) | Transducer platform for impedimetric biosensors | Geometric optimization for COVID-19 antibody detection [52] | |
| Vero Cell Cultures | Cellular platforms for bioelectric recognition assays | Membrane biosensors for SARS-CoV-2 detection [53] |
The integration of machine learning with multi-objective particle swarm optimization represents a transformative approach to biosensor design, outperforming traditional methods across multiple performance metrics. By efficiently navigating complex, high-dimensional parameter spaces and explicitly addressing competing objectives, ML-MOPSO enables the development of biosensors with enhanced sensitivity, specificity, and overall performance. The experimental protocols and reagent solutions outlined in this guide provide researchers with practical frameworks for implementing these advanced computational techniques. As biosensor applications continue to expand in drug development, clinical diagnostics, and environmental monitoring, ML-MOPSO approaches will play an increasingly vital role in pushing the boundaries of detection capabilities while reducing development timelines and costs.
The performance of modern biosensors is fundamentally governed by the precise engineering of their materials and physical structures. The synergistic combination of novel nanocomposites, optimized layer thicknesses, and advanced fiber geometries such as D-shaped sensors pushes the boundaries of sensitivity and specificity, enabling applications from single-molecule detection to multi-analyte diagnostics. This guide provides a comparative analysis of these engineering strategies, framing them within the broader thesis that rational design at the micro- and nanoscale is paramount for advancing biosensor capabilities. We summarize experimental data, detail key methodologies, and outline essential tools for researchers and drug development professionals working at the forefront of sensing technology.
Comparative Performance of Engineered Biosensors
The strategic integration of nanomaterials and structural optimization leads to significant gains in key sensor metrics. The table below provides a quantitative comparison of various biosensor designs, highlighting the impact of different engineering approaches.
Table 1: Performance Comparison of Engineered Biosensor Designs
| Sensor Design & Engineering Focus | Target Analyte | Key Performance Metrics | Refs |
|---|---|---|---|
| Algorithm-Optimized SPR (Kretschmann)• Multi-objective PSO optimization of Au/Cr layer thickness and incident angle | Mouse IgG (Immunoassay) | • Sensitivity: 24,482 nm/RIU• Figure of Merit (FOM): 110.94% improvement• Limit of Detection (LOD): 54 ag/mL (0.36 aM) | [54] |
| D-Shaped PCF-SPR with Au/TiO₂• Plasmonic layer enhancement with TiO₂ on a D-shaped fiber | Cancer Cells (e.g., HeLa, Jurkat) | • Wavelength Sensitivity: 42,000 nm/RIU• Amplitude Sensitivity: -1862 RIU⁻¹• Figure of Merit (FOM): 1393 RIU⁻¹ | [9] |
| SPR with 2D Material Enhancement (WS₂)• BK7/ZnO/Ag/Si₃N₄/WS₂ layered structure | Blood Cancer Cells (Jurkat) | • Angular Sensitivity: 342.14 deg/RIU• Figure of Merit (FOM): 124.86 RIU⁻¹ | [55] |
| Nanocomposite Electrochemical Sensor• Pt NPs/RGO on screen-printed electrode (SPCE) | Hydrogen Peroxide (H₂O₂) | • Detection Limit: 0.65 µM• Linear Range: 1 to 10 µM | [56] |
| Dual LMR Optical Fiber Biosensor• SnO₂ on D-shaped single-mode fiber | C-reactive protein, D-dimer | • Sensitivity: ~4500 nm/RIU• Minimum Detectable Concentration: <1 µg/mL | [57] |
Detailed Experimental Protocols and Methodologies
Algorithm-Assisted Multi-Objective Optimization for SPR Biosensors
This protocol details the computational optimization of a conventional Kretschmann-configuration SPR biosensor (prism/Cr/Au) for ultra-sensitive detection.
- Core Principle: Employ a multi-objective Particle Swarm Optimization (PSO) algorithm to concurrently optimize three design parameters—incident angle, chromium adhesive layer thickness, and gold film thickness—against three performance metrics: sensitivity (S), figure of merit (FOM), and figure of merit with depth (DFOM) [54].
- Workflow:
- Modeling: The SPR structure is modeled as a multi-layer medium, and its optical characteristics (reflectance spectrum) are computed using the iterative transfer matrix method [54].
- Algorithm Execution: The PSO algorithm is run for a typical 150 iterations to find the parameter set that maximizes the combined fitness function based on S, FOM, and DFOM [54].
- Robustness Analysis: The k-means clustering method is applied to the optimized parameter set to identify a central, robust design point that mitigates the impact of potential processing errors [54].
- Experimental Validation: The optimized sensor is tested against mouse IgG in a buffer solution. The binding of the analyte causes a shift in the resonance wavelength or angle, which is measured to validate the calculated sensitivity and LOD [54].
The following diagram illustrates the workflow of the multi-objective optimization process for SPR biosensors.
Design and Fabrication of a D-Shaped PCF-SPR Biosensor
This protocol outlines the steps for designing, simulating, and fabricating a high-sensitivity D-shaped photonic crystal fiber SPR biosensor.
- Core Principle: A D-shaped PCF with a flat surface is coated with an optimized stack of gold and titanium dioxide (TiO₂) to excite surface plasmons. The TiO₂ layer enhances the sensitivity and the D-shaped geometry facilitates easier and more uniform coating while strengthening the coupling between the core mode and the surface plasmon wave [9].
- Workflow:
- Structural Design & Simulation: The PCF structure is designed with air holes arranged in a specific lattice. Finite Element Method (FEM) simulations are performed to analyze the mode field distribution and the loss spectrum [9].
- Parameter Optimization: Structural parameters such as the diameters and pitch of the air holes, as well as the thickness of the Au and TiO₂ layers, are varied in the simulation to maximize wavelength and amplitude sensitivity [9].
- Fiber Fabrication: A standard PCF is side-polished to create a flat D-shaped surface, ensuring the core is in close proximity to the polishing plane [9].
- Plasmonic Layer Deposition: The flat surface of the fiber is sequentially coated with a thin film of gold, followed by a layer of TiO₂, using precise deposition techniques like sputtering to achieve uniform, nanoscale thicknesses [9].
- Analytical Testing: The sensor is integrated into a flow cell system. Different cancer cell suspensions (e.g., HeLa, Jurkat) are passed over the sensor surface, and the resulting shifts in the resonance wavelength in the output spectrum are measured to quantify sensitivity [9].
Development of a Nanocomposite Electrochemical Biosensor for 3D Cell Cultures
This protocol describes the creation of a non-enzymatic electrochemical sensor for monitoring oxidative stress in cancer cells cultured within a 3D hydrogel environment.
- Core Principle: A screen-printed carbon electrode (SPCE) is modified with a nanocomposite of reduced graphene oxide (RGO) and platinum nanoparticles (Pt NPs). This platform offers high electrocatalytic activity for H₂O₂ reduction. Cells are immobilized in a GelMA/RGO hydrogel on the electrode, enabling in-situ monitoring of reactive oxygen species (ROS) induced by drug treatments [56].
- Workflow:
- Electrode Modification:
- RGO Formation: A dispersion of graphene oxide (GO) is drop-cast onto the SPCE and electrochemically reduced to form conductive RGO.
- Pt NPs Deposition: Pt nanoparticles are electrodeposited onto the RGO/SPCE by performing cyclic voltammetry (CV) in a solution of K₂PtCl₆, resulting in a Pt NPs/RGO/SPCE sensor [56].
- Hydrogel Preparation & Cell Encapsulation: A solution of gelatin methacrylate (GelMA) and GO is mixed with a suspension of cancer cells (e.g., NCI-H1975). This mixture is dropped onto the sensor and crosslinked under UV light, forming a 3D hydrogel matrix that entraps the cells directly on the electrode surface [56].
- Electrochemical Measurement: The embedded GO in the hydrogel is electrochemically reduced to RGO to enhance conductivity. To measure oxidative stress, the sensor is placed in a buffer, and the current response is monitored via techniques like differential pulse voltammetry (DPV) after introducing a drug (e.g., honokiol). An increase in the reduction current corresponds to elevated H₂O₂ levels released from the cells [56].
- Electrode Modification:
The workflow for fabricating the nanocomposite electrochemical biosensor and its application in drug response monitoring is shown below.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of the aforementioned protocols relies on a suite of specialized materials and reagents. The table below details these key components and their functions.
Table 2: Essential Research Reagents and Materials for Biosensor Engineering
| Material/Reagent | Function in Biosensor Development | Examples & Key Characteristics |
|---|---|---|
| Plasmonic Metals | Form the active layer for SPR; gold is preferred for its stability and bio-conjugation chemistry. | Gold (Au), Silver (Ag). Au offers excellent chemical stability and surface functionalization [54] [9]. |
| Enhancing 2D Materials & Oxides | Boost sensitivity by enhancing the electric field and/or providing high surface area for biomolecule interaction. | Titanium Dioxide (TiO₂), Tungsten Disulfide (WS₂), Graphene. TiO₂ used as an overlayer on Au to significantly enhance sensitivity in PCF sensors [9] [55]. |
| Nanocomposite Components | Form the sensing interface in electrochemical sensors, providing high conductivity and catalytic activity. | Reduced Graphene Oxide (RGO), Platinum Nanoparticles (Pt NPs). RGO offers high surface area and conductivity; Pt NPs are excellent catalysts for H₂O₂ reduction [56]. |
| Structural Substrates | Serve as the mechanical and optical platform for the sensor. | D-Shaped Photonic Crystal Fiber (PCF), Prisms (BK7). D-shaped PCF allows for practical deposition of plasmonic layers and strong core-SPP coupling [57] [9]. |
| Biorecognition Elements | Provide the specific binding mechanism for the target analyte. | Antibodies (e.g., anti-mouse IgG), DNA probes. Immobilized on the sensor surface to capture specific proteins or nucleic acids [54]. |
| 3D Cell Culture Matrix | Creates a biomimetic environment for housing cells on the sensor surface. | Gelatin Methacrylate (GelMA) Hydrogel. A photocrosslinkable biocompatible hydrogel that allows for cell encapsulation and nutrient diffusion [56]. |
The strategic engineering of materials and structures is a powerful driver for innovation in biosensing. As demonstrated, algorithms can push conventional SPR designs to single-molecule detection limits, the integration of 2D materials and oxides like TiO₂ and WS₂ can dramatically amplify sensitivity, and novel D-shaped fiber geometries enable more practical and high-performance plasmonic sensors. Simultaneously, nanocomposites like RGO-Pt are unlocking new capabilities in electrochemical monitoring within biologically relevant 3D environments. The continued interdisciplinary collaboration between material science, optics, and biochemistry, guided by computational optimization, will undoubtedly yield the next generation of biosensors with unparalleled sensitivity and specificity for advanced research and clinical diagnostics.
For researchers and scientists driving innovation in drug development and clinical diagnostics, the promise of biosensors is frequently tempered by persistent real-world challenges. Signal drift, sample interference, and surface fouling represent a trinity of obstacles that compromise the sensitivity, specificity, and reliability of biosensing platforms, particularly when transitioning from controlled buffer solutions to complex biological matrices [58] [59]. These issues become critically important when detecting low-abundance biomarkers in undiluted serum, plasma, or whole blood, where protein concentrations can reach 60-80 mg/mL, creating a high potential for nonspecific binding and signal masking [60]. This guide objectively compares the performance of emerging strategies and materials designed to overcome these barriers, providing experimental methodologies and data to inform material selection for next-generation biosensor development.
Comparative Analysis of Mitigation Strategies and Material Performance
Table 1: Performance Comparison of Signal Drift Mitigation Approaches
| Mitigation Strategy | Experimental Setup | Key Performance Metrics | Reported Efficacy | Limitations/Requirements |
|---|---|---|---|---|
| D4-TFT Testing Methodology [58] | CNT-based BioFETs in 1X PBS; Pd pseudo-reference electrode; infrequent DC sweeps | Phase sensitivity; Signal stability over time | Attomolar (aM) detection in physiological ionic strength; Stable performance in 1X PBS | Requires rigorous testing protocol; Specific passivation and coating |
| Stable Electrical Testing Configuration [58] | Combination of passivation, stable electrical configuration, specific coating (POEGMA) | Reduction in temporal signal drift | Enabled distinction between true biomarker signal and drift artifacts | Dependent on specific material integration |
| Electrochemical Activation [59] | Application of cathodic/anodic potential or pulse trains to electrodes | Preservation of electrochemical signal in complex media | Effective for desorption of fouling species | Risk of catalyst degradation or physical detachment |
Table 2: Antifouling Material Efficacy in Complex Biological Media
| Antifouling Material | Mechanism of Action | Experimental Validation | Signal Retention | Optimal Application Context |
|---|---|---|---|---|
| POEGMA Polymer Brush [58] | Donnan potential extension of Debye length; Non-fouling properties | D4-TFT platform in 1X PBS; Antibody printing within brush | Sub-femtomolar detection in undiluted PBS | BioFETs in physiological ionic strength solutions |
| Sol-Gel Silicate Layer [59] | Porous physical barrier; Mechanical and thermal stability | Extended incubation in cell culture medium | ~50% signal retained after 6 weeks | Long-term implantable sensors |
| Poly-l-lactic acid [59] | Hydrophobic barrier layer | Incubation in cell culture environment | Complete deterioration after 72 hours | Short-term cell culture applications |
| Poly(L-lysine)-g-poly(ethylene glycol) [59] | Repellent surface properties; Biocompatibility | Cell culture medium incubation | Sustained catalyst performance during prolonged incubation | Biosensors in cell culture environments |
| PEG and Derivatives [59] [60] | Hydrophilic barrier; Strong repulsive hydration forces | SPR sensing in serum/plasma | Reduced non-specific adsorption in complex fluids | General purpose surface modification |
| Zwitterionic Polymers [60] | Superhydrophilicity; Electrostatic interaction | SPR clinical diagnostics | High fouling resistance in blood, serum | Detection in high-protein environments |
Experimental Protocols for Benchmarking Biosensor Stability
Protocol: D4-TFT for Signal Drift Mitigation and Charge Screening
The D4-TFT (Dispense, Dissolve, Diffuse, Detect with Thin-Film Transistor) platform represents a significant advancement for achieving stable electrical biosensing in biologically relevant ionic strength solutions [58].
Materials Required:
- Carbon nanotube (CNT) thin-film transistors
- Poly(oligo(ethylene glycol) methyl ether methacrylate) (POEGMA)
- Palladium (Pd) pseudo-reference electrode
- Target-specific capture and detection antibodies
- Phosphate-buffered saline (1X PBS), pH 7.4
- Printed circuit board with automated testing software
Methodology:
- Device Fabrication: Prepare CNT-TFTs using solution-phase processability methods to ensure high mobility and chemical inertness.
- Surface Functionalization: Grow POEGMA polymer brush on high-κ dielectrics above the CNT channel to establish Donnan equilibrium potential and extend Debye length.
- Antibody Immobilization: Inkjet-print capture antibodies (cAb) into the POEGMA matrix, reserving control devices with no antibodies.
- Assay Assembly: Print detection antibodies (dAb) conjugated with a readily-dissolvable excipient layer (trehalose) above the transistor channel.
- Testing Configuration: Implement a stable electrical testing system with a Pd pseudo-reference electrode to eliminate need for bulky Ag/AgCl electrodes.
- Measurement Protocol: Conduct infrequent DC sweeps rather than static or AC measurements to minimize drift contributions.
- Data Analysis: Compare signals between active and control devices, confirming specific detection via on-current shifts caused by antibody sandwich formation.
Validation Metrics: Achievable attomolar (aM) detection limits in 1X PBS (physiological ionic strength) with no signal change in control devices confirms successful drift mitigation and charge screening overcome [58].
Protocol: Evaluating Antifouling Coating Efficacy for Electrochemical Sensors
This protocol screens various antifouling layers for their ability to preserve electrochemical sensor function in complex biological media [59].
Materials Required:
- Carbon working electrodes (pencil lead, glassy carbon, or screen-printed electrodes)
- Syringaldazine (redox mediator)
- Antifouling coating materials (sol-gel silicate, poly-l-lactic acid, PEG, etc.)
- Cell culture medium (DMEM with 10% FBS recommended)
- Ag/AgCl reference electrode, platinum counter electrode
- Potentiostat for electrochemical measurements
Methodology:
- Electrode Preparation: Polish carbon electrodes sequentially on sandpaper and copy paper, then with alumina slurry.
- Mediator Adsorption: Immerse electrodes in 0.5 mg/mL syringaldazine solution in ethanol for 60 seconds, dry under ambient conditions.
- Coating Application: Apply candidate antifouling layers using optimized procedures for each material type.
- Baseline Measurement: Record cyclic voltammetry (CV) in phosphate buffer (pH 7.4) from -0.2 V to +0.8 V with 100 mV/s scan rate.
- Incubation Challenge: Incubate coated electrodes in cell culture medium at 37°C for durations from 3 hours to 6 weeks.
- Performance Assessment: Periodically measure electrochemical response using CV, DPV, or SWV in clean buffer solution.
- Data Analysis: Calculate percentage signal retention relative to pre-incubation baseline for each coating type.
Validation Metrics: Successful coatings maintain stable electrochemical signals during prolonged incubation. Superior coatings like sol-gel silicate retain approximately 50% signal after 6 weeks, while inferior coatings show complete deterioration within 72 hours [59].
Visualization of Biosensor Stabilization Mechanisms
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Advanced Biosensor Development
| Material/Reagent | Primary Function | Application Context | Key Considerations |
|---|---|---|---|
| POEGMA Polymer Brush [58] | Extends Debye length via Donnan potential; Provides non-fouling surface | BioFETs operating in physiological ionic strength | Enables antibody-antigen binding beyond traditional screening limits |
| Sol-Gel Silicate [59] | Porous antifouling barrier; High mechanical/thermal stability | Long-term implantable sensors | Maintains ~50% signal integrity after 6 weeks in cell culture |
| Carbon Nanotubes (CNTs) [58] | High-mobility semiconductor channel; Solution-phase processability | Thin-film transistor biosensors | Intrinsic high sensitivity; Chemical inertness |
| Palladium Pseudo-Reference Electrode [58] | Stable potential reference; Miniaturized form factor | Point-of-care biosensing devices | Replaces bulky Ag/AgCl electrodes |
| Poly(ethylene glycol) Derivatives [59] [60] | Antifouling via hydrophilic repulsion; Biocompatibility | General surface modification | Various chain lengths available for monolayer thickness control |
| Syringaldazine [59] | Adsorbed redox mediator for coating evaluation | Antifouling material screening | pH-sensitive response allows monitoring of coating integrity |
| Zwitterionic Polymers [60] | Superhydrophilic antifouling via electrostatic interactions | SPR biosensing in serum/blood | High oxidative resistance and hydrolytic stability |
The comparative data presented in this guide demonstrates that effective mitigation of signal drift, sample interference, and fouling requires integrated approaches combining material science, device architecture, and testing methodologies. For researchers targeting clinical applications, the D4-TFT platform provides a compelling framework for achieving attomolar sensitivity in physiologically relevant conditions while maintaining signal stability [58]. For long-term implantation studies, sol-gel silicate coatings offer exceptional durability, retaining significant signal integrity after weeks in complex biological environments [59]. The selection of antifouling strategies must be guided by the specific application requirements, including target matrix complexity, required detection limits, and operational duration. As biosensing continues to advance toward point-of-care and continuous monitoring applications, addressing these fundamental challenges will be essential for translating laboratory innovations into clinically viable diagnostic tools.
The integration of Artificial Intelligence (AI) into biosensor development has revolutionized the optimization of diagnostic devices, enabling unprecedented improvements in sensitivity and specificity. However, the superior predictive performance of complex machine learning (ML) models often comes at the cost of interpretability, creating a significant "black box" problem where the rationale behind model decisions remains opaque [61]. This opacity poses a substantial barrier to clinical adoption, as researchers, regulators, and clinicians require understanding of how and why a model arrives at a specific design recommendation or performance prediction [62].
Explainable AI (XAI) has emerged as a critical field addressing this challenge by making AI decision-making processes transparent, understandable, and trustworthy [61]. In biosensor research, XAI techniques are increasingly deployed to interpret model outputs and identify which design parameters most significantly influence sensor performance. This capability is transforming biosensor development from a trial-and-error process to a systematic, data-driven endeavor, accelerating the creation of highly sensitive and specific diagnostic platforms for medical and pharmaceutical applications [63].
Core XAI Methodologies in Biosensor Research
Dominant XAI Techniques and Their Applications
XAI encompasses diverse techniques for model interpretation, with several emerging as particularly valuable for biosensor optimization. These methods can be broadly categorized by their scope of explanation—whether they interpret individual predictions (local) or the entire model behavior (global).
Table 1: Core XAI Techniques in Biosensor Development
| Technique | Category | Primary Function | Key Advantage | Representative Application in Biosensors |
|---|---|---|---|---|
| SHAP (SHapley Additive exPlanations) [10] [64] [61] | Model-agnostic, Local & Global | Quantifies the contribution of each input feature to a single prediction or overall model output. | Provides mathematically consistent, theoretically grounded feature importance values. | Identifying critical design parameters (e.g., gold thickness, wavelength) in PCF-SPR and fiber-optic SPR sensors [10] [64]. |
| LIME (Local Interpretable Model-agnostic Explanations) [64] | Model-agnostic, Local | Approximates a complex model locally with an interpretable one to explain individual predictions. | Creates simple, intuitive explanations for specific instances without revealing the full model. | Explaining individual predictions of sensor FOM based on specific λ and dm combinations [64]. |
| Partial Dependence Plots (PDPs) [61] | Model-agnostic, Global | Visualizes the relationship between a feature and the predicted outcome while averaging out other features. | Illustrates the marginal effect of a feature on the prediction, helpful for understanding trends. | Showing the global relationship between a design parameter and sensor sensitivity. |
| Permutation Feature Importance (PFI) [61] | Model-agnostic, Global | Measures the increase in model error when a single feature is randomly shuffled. | Simple, intuitive method for ranking features by their importance to model accuracy. | Ranking the importance of various structural and material parameters for biosensor performance. |
The XAI Workflow in Biosensor Design
The application of XAI follows a structured pipeline that integrates computational modeling with physical sensor design. The workflow below illustrates how XAI bridges the gap between complex AI models and actionable engineering insights.
Comparative Analysis of XAI Applications in Biosensor Optimization
Case Study 1: Photonic Crystal Fiber (PCF)-SPR Biosensor
A landmark 2025 study exemplifies the power of XAI in optimizing advanced optical biosensors. Researchers developed a highly sensitive PCF-SPR biosensor and employed a hybrid ML-XAI approach to accelerate design optimization [10] [65].
- Experimental Protocol: The study combined finite-element simulation (using COMSOL Multiphysics) with multiple ML regression models, including Random Forest and Gradient Boosting. The models were trained to predict key optical properties—effective index (Neff), confinement loss (CL), and amplitude sensitivity (SA)—from design parameters [10] [65].
- XAI Implementation: SHAP analysis was applied to the trained models to interpret outputs and quantify parameter influence globally [10].
- Performance Outcome: The optimized biosensor achieved exceptional performance: a maximum wavelength sensitivity of 125,000 nm/RIU, amplitude sensitivity of -1422.34 RIU⁻¹, and a figure of merit (FOM) of 2112.15 [10] [65].
Table 2: SHAP-Derived Critical Parameters in PCF-SPR Biosensor [10]
| Design Parameter | Relative Influence | Impact on Sensor Performance |
|---|---|---|
| Wavelength (λ) | Highest | Directly determines the resonance condition and the operating point of the sensor. |
| Analyte Refractive Index (na) | Very High | The target property for detection; changes in na directly shift the resonance. |
| Gold Layer Thickness (tg) | High | Critically affects the strength and sharpness of the surface plasmon resonance. |
| Pitch (Λ) | Moderate | Influences the guiding properties of the photonic crystal fiber and mode confinement. |
Case Study 2: Fiber-Optic SPR Sensor with 2D Materials
A complementary study focused on a fiber-optic SPR sensor coated with a Molybdenum Disulfide (MoS₂) monolayer, using XAI to resolve a key design question [64].
- Experimental Protocol: A Gaussian Process Regression (GPR) model was trained on a dataset of 1581 combinations of light wavelength (λ) and metal layer thickness (dm) to predict the sensor's FOM [64].
- XAI Implementation: Both SHAP (global) and LIME (local) analyses were implemented and comparatively assessed to explain the GPR model's predictions [64].
- Key Finding: Both XAI methods conclusively demonstrated that metal layer thickness (dm) has a significantly greater influence on the FOM than the wavelength (λ). This finding was consistent with the physical concept of radiation damping, validating the XAI interpretation against domain knowledge [64].
- Practical Impact: This insight is crucial for fabrication, indicating that tighter control over metal deposition is more critical than precise tuning of the light source for maximizing sensor performance [64].
Comparative Performance and Technical Insights
Table 3: Cross-Study Comparison of XAI for Biosensor Optimization
| Aspect | PCF-SPR Biosensor [10] | Fiber-Optic SPR Sensor [64] |
|---|---|---|
| Sensor Type | Photonic Crystal Fiber-based SPR | Conventional Fiber-optic with MoS₂ coating |
| Primary ML Model | Ensemble Methods (RF, GB) | Gaussian Process Regression (GPR) |
| Key Performance Metric | Wavelength & Amplitude Sensitivity | Figure of Merit (FOM) |
| Dominant XAI Technique | SHAP | SHAP & LIME (comparative) |
| Most Critical Parameter | Wavelength (λ) | Metal Layer Thickness (dm) |
| Key Outcome | Identified complex multi-parameter interactions | Resolved relative importance of two key parameters |
| Physical Validation | High performance metrics | Consistency with radiation damping theory |
The comparison reveals that the "most critical" parameter is context-dependent. For the complex PCF-SPR architecture with multiple structural degrees of freedom, the operating wavelength emerged as most influential [10]. In contrast, for the thin-film coated fiber-optic sensor, the metal thickness was paramount [64]. This underscores that XAI does not provide universal answers but rather reveals parameter criticality specific to the sensor design and performance objective.
The Scientist's Toolkit: Essential Reagents and Materials
The successful application of XAI in biosensor development relies on a foundation of both computational tools and physical materials.
Table 4: Key Research Reagent Solutions for XAI-Enhanced Biosensor Development
| Category | Item / Technique | Critical Function | Example Use Case |
|---|---|---|---|
| Simulation Software | COMSOL Multiphysics [10] [65] | Finite-element analysis for simulating electromagnetic fields and sensor performance. | Modeling light propagation and plasmonic effects in PCF-SPR sensors. |
| ML/XAI Libraries | SHAP, LIME [10] [64] [61] | Python libraries for post-hoc model interpretation and feature importance calculation. | Quantifying the influence of gold thickness and pitch on sensitivity. |
| Plasmonic Materials | Gold (Au) thin films [10] [65] | Provides the conductive layer for exciting surface plasmons; chosen for chemical stability. | Plasmonic layer in PCF-SPR biosensors for biomarker detection. |
| 2D Material Coatings | Molybdenum Disulfide (MoS₂) [64] | Enhances sensitivity and provides a platform for biomolecule functionalization. | Coating on fiber-optic SPR sensors to improve FOM. |
| Optical Components | Broadband Light Source, Optical Spectrum Analyzer (OSA) [65] | Injects light and detects spectral shifts in the sensor output for label-free detection. | Experimental setup for characterizing PCF-SPR sensor response. |
The integration of Explainable AI represents a paradigm shift in biosensor research and development. By moving beyond "black box" models, XAI techniques like SHAP and LIME empower researchers to identically identify the most critical design parameters—such as metal layer thickness, operating wavelength, and structural pitch—that govern sensor sensitivity and specificity [10] [64]. This data-driven insight significantly accelerates the design optimization cycle, reduces computational costs, and fosters a deeper understanding of the underlying physical phenomena [10].
For researchers and drug development professionals, mastering these XAI methodologies is becoming essential. The ability to interpret AI models not only builds trust in automated design systems but also ensures that the next generation of biosensors will meet the rigorous demands of high-precision medical diagnostics, personalized therapeutics, and point-of-care testing [22] [63]. As the field progresses, the convergence of XAI with emerging biosensing platforms promises to further redefine the boundaries of diagnostic sensitivity and specificity.
From Bench to Bedside: Validation Protocols and Comparative Analysis for Real-World Deployment
The development and adoption of medical biosensors depend on a rigorous, multi-stage validation process. This process, often conceptualized as a clinical validation ladder, systematically progresses from fundamental analytical studies in controlled laboratory settings to evaluations in complex, real-world clinical environments. Demonstrating high sensitivity and specificity is paramount at every stage, though the methods and implications differ significantly. This guide compares the key validation stages—analytical studies, controlled clinical trials, and prospective real-world studies—by outlining their distinct experimental protocols, performance metrics, and roles in building a comprehensive evidence base for biosensor technology.
Stage 1: Analytical Performance Studies
Analytical studies form the foundational first rung of the validation ladder, assessing the core technical performance of a biosensor under ideal, controlled conditions.
Experimental Protocols
The primary goal is to quantify the sensor's basic operational characteristics using standardized laboratory procedures.
- Limit of Detection (LOD) and Quantification (LOQ): The biosensor is tested with a series of standard solutions with known analyte concentrations, including blank samples. The LOD is typically determined as the lowest concentration that can be reliably distinguished from the blank, often calculated as three times the standard deviation of the blank signal. The LOQ, usually ten times the standard deviation of the blank, is the lowest concentration that can be quantitatively measured with acceptable precision and accuracy [14].
- Sensitivity and Dynamic Range: The sensor's response is measured across a wide range of analyte concentrations. The sensitivity is derived from the slope of the calibration curve (signal output vs. concentration). The dynamic range spans from the LOQ to the concentration where the signal plateaus or becomes non-linear [30].
- Specificity and Cross-Reactivity: The biosensor is exposed to structurally similar compounds or potential interfering substances commonly found in the sample matrix (e.g., uric acid, ascorbic acid in blood). The degree of signal generation from these interferents, compared to the target analyte, quantifies cross-reactivity and demonstrates specificity [14].
Key Performance Data
The following table summarizes typical outcomes and benchmarks for biosensors at the analytical stage, based on recent research.
Table 1: Representative Performance Metrics from Recent Analytical Biosensor Studies
| Biosensor Target | Technology | Reported Sensitivity | Limit of Detection (LOD) | Specificity Notes | Source |
|---|---|---|---|---|---|
| α-Fetoprotein (AFP) Cancer Biomarker | SERS Immunoassay (Au-Ag Nanostars) | - | 16.73 ng/mL | Functionalized with anti-AFP antibodies; intrinsic AFP vibrational modes used. | [14] |
| Cancerous Cells (e.g., Jurkat, HeLa) | SPR with ZnO/Ag/Si3N4/WS2 Layers | 342.14 deg/RIU (Blood Cancer) | - | Demonstrated ability to distinguish cancerous from healthy cells. | [30] |
| Glucose | Electrochemical (Nanostructured Composite) | 95.12 ± 2.54 µA mM−1 cm−2 | - | High selectivity achieved in interstitial fluid. | [14] |
Stage 2: Controlled Clinical Trials
After establishing analytical validity, biosensors enter controlled clinical trials. These studies are considered the "gold standard" for evaluating efficacy and safety in a targeted patient population under highly regulated conditions [66].
Experimental Protocols
These trials are characterized by their prospective, interventional design.
- Randomization and Blinding: Patients are randomly assigned to a group that uses the biosensor-guided intervention or a control group (e.g., standard of care). Double-blinding, where neither the patient nor the investigator knows the group assignment, is employed to minimize bias [66].
- Strict Eligibility Criteria: Participants are selected based on specific inclusion and exclusion criteria (e.g., age, disease severity, absence of comorbidities) to create a homogeneous study population and minimize the influence of confounding variables [66].
- Predefined Endpoints: The trials use objective, validated endpoints to assess the biosensor's performance in a clinical context. For example, a trial for a cardiac biosensor might use periodic venous blood draws analyzed by a central laboratory as the reference standard to validate the sensor's continuous readings [66].
Key Performance Data
Controlled trials generate evidence on clinical efficacy, moving beyond pure analytical performance.
Table 2: Comparison of Controlled Clinical Trial vs. Analytical Study Characteristics
| Characteristic | Analytical Performance Study | Controlled Clinical Trial |
|---|---|---|
| Primary Objective | Establish technical performance (Sensitivity, LOD) | Establish clinical efficacy and safety |
| Study Environment | Laboratory | Clinical or highly controlled research setting |
| Sample Type | Standard solutions, contrived samples | Human participants with the target condition |
| Key Metrics | Sensitivity, Specificity, LOD, LOQ | Clinical Sensitivity/Specificity, PPV/NPV, AUC, Safety Outcomes |
| Population | N/A | Highly selective based on strict criteria |
| Data Output | Technical readout (e.g., µA, deg/RIU) | Clinical decision-making information |
Stage 3: Prospective Real-World Studies
The final rung on the validation ladder assesses the biosensor's effectiveness—how well it performs in routine clinical practice with diverse patient populations and less controlled conditions [66].
Experimental Protocols
These studies are prospective and observational, meaning researchers collect data as patients use the biosensor in their normal care settings without interventional protocols.
- Pragmatic Design: The study design includes "all-comers" from community-based clinics, encompassing patients who would typically be excluded from controlled trials due to comorbidities, age, or polypharmacy. There is minimal control over treatment adherence or concomitant therapies [66] [67].
- Real-World Data (RWD) Collection: Data is often collected from electronic health records, insurance claims databases, or patient registries. The endpoints focus on practical outcomes relevant to patients and clinicians, such as quality of life, hospital readmission rates, or long-term cost-effectiveness [66] [68].
- Target Trial Emulation: To minimize bias, a state-of-the-art approach is to use the "target trial emulation" framework. Researchers first specify the protocol for a hypothetical ideal randomized trial and then design their analysis of the observational RWD to mimic that trial as closely as possible, including the use of advanced statistical methods like propensity score matching to control for confounding [67].
Key Performance Data
Real-world studies provide critical evidence on how the biosensor integrates into clinical workflow and impacts patient care outside a research setting.
Table 3: Key Differences Between Controlled Clinical Trials and Prospective Real-World Studies
| Characteristic | Controlled Clinical Trial (Efficacy) | Prospective Real-World Study (Effectiveness) |
|---|---|---|
| Primary Question | "Can it work under ideal conditions?" | "Does it work in routine practice?" |
| Study Population | Selective, homogeneous | Broad, heterogeneous ("all-comers") |
| Data Sources | Prospective research data, Case Report Forms | Electronic Health Records, Claims Databases, Registries |
| Intervention & Environment | Strictly controlled, protocol-driven | Routine clinical practice, flexible use |
| Key Outcomes | Efficacy, mechanistic insights, safety | Effectiveness, long-term safety, cost-effectiveness, QoL |
| Statistical Methods | Intent-to-Treat, ANOVA, Cox models | Propensity Score Matching, Target Trial Emulation |
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and materials are fundamental for conducting experiments across the biosensor validation ladder, particularly in the analytical and controlled clinical stages.
Table 4: Essential Research Reagents and Materials for Biosensor Validation
| Reagent/Material | Function in Validation | Application Example |
|---|---|---|
| Monoclonal Anti-α-fetoprotein (AFP) Antibodies | Capture and detection agent for a specific biomarker. | Functionalizing a SERS platform for the detection of liver cancer biomarkers [14]. |
| Mercaptopropionic Acid (MPA) | Forms a self-assembled monolayer on metal surfaces (e.g., gold, silver). | Used as a linker molecule on Au-Ag nanostars to covalently attach antibodies via EDC/NHS chemistry [14]. |
| EDC & NHS | Cross-linking agents for carbodiimide chemistry. | Activates carboxyl groups on a surface (e.g., from MPA) to form stable amide bonds with primary amines in antibodies [14]. |
| Transition Metal Dichalcogenides (TMDCs like WS₂) | 2D material used to enhance sensor performance. | Incorporated into SPR sensor architectures to significantly improve sensitivity and light-matter interaction [30]. |
| Au-Ag Nanostars | Plasmonic substrate for signal enhancement. | Serves as the core platform in SERS-based immunoassays, providing intense electromagnetic fields at their sharp tips [14]. |
Visualizing the Clinical Validation Pathway
The following diagram maps the logical progression and key decision points along the clinical validation ladder for biosensors.
The validation of biosensors represents a critical bridge between technological innovation and clinical application. For researchers, scientists, and drug development professionals, establishing statistical rigor is paramount when translating biosensor capabilities into credible diagnostic tools. This guide objectively compares methodological approaches for evaluating biosensor performance, focusing on the interrelated pillars of endpoint selection, sample size determination, and agreement analysis. The framework is contextualized within a broader thesis on evaluating biosensor sensitivity and specificity, where statistical precision directly correlates with diagnostic reliability and clinical adoption potential.
Statistical validation protocols for biosensors must satisfy dual objectives: demonstrating technical superiority against existing alternatives while meeting regulatory standards for clinical validity. This requires a staged evidentiary approach that progresses from controlled benchtop experiments to real-world clinical deployment [69]. Within this continuum, specific statistical methodologies—including the Bland-Altman analysis for method comparison, exact sample size calculations for binary endpoints, and precise endpoint definitions—serve as validation benchmarks that investors and regulatory bodies scrutinize closely [69] [70] [71].
Establishing Primary Endpoints and Analytical Frameworks
Defining Primary Endpoints for Biosensor Performance
Primary endpoints form the foundational metrics upon which biosensor validation rests. These endpoints must be carefully selected to align with both the biosensor's intended use and regulatory expectations. Different biosensor applications demand distinct endpoint hierarchies, though all share the common requirement of objective quantification against recognized reference standards.
Table 1: Primary Endpoint Selection by Biosensor Application
| Biosensor Application | Recommended Primary Endpoints | Appropriate Comparator (Gold Standard) | Performance Targets |
|---|---|---|---|
| Rhythm/Arrhythmia Detection | Patient-level sensitivity & specificity for conditions like atrial fibrillation [69] | 12-lead ECG interpreted by cardiologists [69] | Sensitivity ≥0.95 with tight CI [69] |
| Heart Rate Monitoring | Mean absolute error (MAE) in beats/min across activity states [69] | Clinical-grade ECG (time-synchronized) [69] | MAE ≤5 bpm [69] |
| Cuffless Blood Pressure | Mean error and limits of agreement [69] | Validated sphygmomanometer (ISO 81060) [69] | Pre-specified clinically meaningful bounds [69] |
| Cancer Biomarker Detection | Sensitivity in deg/RIU (refractive index units) [30] | Laboratory techniques (e.g., for BRCA genes) [30] | Up to 342.14 deg/RIU for blood cancer detection [30] |
| Continuous Molecular Monitoring | Signal-to-noise ratio (SNR) in pre-equilibrium conditions [72] | Reference concentration measurements [72] | Optimized for specific target concentration ranges [72] |
For biosensors targeting diagnostic applications, sensitivity and specificity at the patient level represent the most clinically relevant endpoints [69]. These should be complemented by continuous accuracy metrics like Mean Absolute Error (MAE) for physiological monitoring and limits of agreement for method comparison studies [69] [70]. Emerging biosensor technologies, particularly those employing novel approaches like pre-equilibrium sensing, require specialized endpoints such as signal-to-noise ratio (SNR) that account for kinetic parameters and measurement dynamics [72].
Statistical Analysis Protocols
Robust statistical analysis plans must be pre-specified in study protocols to minimize analytical bias and provide credible interval estimates for performance metrics.
- Sensitivity/Specificity Analysis: Report patient-level sensitivity and specificity with exact (Clopper-Pearson) 95% confidence intervals to account for binomial proportions [69]. Predefine positive identification rules (e.g., episode length thresholds for arrhythmia detection) prior to data collection.
- Bland-Altman Analysis: For continuous measurements, implement Bland-Altman plots to visualize agreement between biosensor and gold standard measurements [69] [70]. Calculate mean bias (with 95% confidence intervals) and 95% limits of agreement (mean bias ± 1.96 × standard deviation of differences) [70]. This method is particularly valuable for quantifying measurement agreement across the analytical measurement range.
- Continuous Metric Analysis: For accuracy endpoints like heart rate monitoring, calculate MAE (mean absolute error), RMSE (root mean square error), and ICC (intraclass correlation coefficient) to capture different dimensions of measurement performance [69].
- Subgroup Analyses: Pre-plan analyses across participant subgroups defined by skin tone (using Fitzpatrick categories or measured reflectance), motion levels, age brackets, and clinical conditions to evaluate equity performance [69].
Sample Size Determination Methodologies
Exact Sample Size Calculations for Binary Endpoints
Sample size determination represents a critical pre-study consideration that directly impacts the validity and generalizability of biosensor performance claims. For diagnostic biosensors targeting binary outcomes (e.g., disease present/absent), exact sample size methods that account for endpoint correlation provide superior statistical precision compared to approximate approaches [71].
When designing studies for biosensors that require evaluation against two co-primary binary endpoints, incorporating the correlation between endpoints increases trial power and reduces required sample size [71]. For example, a biosensor might need to demonstrate significance on both sensitivity and specificity targets simultaneously rather than just one metric. The exact approach incorporates this correlation structure, preventing underpowered studies that plague approximate methods [71].
For a single primary binary endpoint, such as sensitivity for a specific condition, sample size calculation requires specifying the desired sensitivity, confidence interval width, and expected prevalence [69]. The formula for calculating required positive cases is:
n_pos = [Z² × Se × (1 - Se)] / d²
Where:
- Z = Z-value for confidence level (1.96 for 95% CI)
- Se = Desired sensitivity
- d = Allowable half-width of confidence interval
The total sample size is then calculated by adjusting for disease prevalence: N = n_pos / prevalence [69].
Table 2: Sample Size Scenarios for Biosensor Validation Studies
| Study Objective | Target Parameter | Prevalence/ Rate | Confidence Level | Precision (CI Width) | Required Sample |
|---|---|---|---|---|---|
| Atrial Fibrillation Detection | Sensitivity = 0.95 [69] | 5% [69] | 95% [69] | d = 0.03 [69] | 4,060 participants [69] |
| Co-primary Binary Endpoints | Two correlated binary endpoints | Varies | 95% | Target power 90% | Reduced vs. independent calculation [71] |
| Bayesian Credible Intervals | Proportion parameter | Varies | 95% credible interval | Calibrated approximation | Based on predictive analysis [73] |
Workflow for Sample Size Determination
Bland-Altman Analysis for Method Comparison
Principles and Application in Biosensor Validation
The Bland-Altman method provides an essential statistical framework for assessing agreement between biosensor measurements and established gold standard methods [70]. Unlike correlation coefficients that measure association rather than agreement, Bland-Altman analysis quantifies systematic bias and random error components between measurement techniques [70]. This approach is particularly valuable for biosensor validation because it identifies both the magnitude and direction of measurement differences across the analytical range.
The core output of Bland-Altman analysis includes:
- Mean bias: The average difference between biosensor and reference method measurements, indicating systematic overestimation or underestimation.
- Limits of Agreement (LOA): Defined as mean bias ± 1.96 × standard deviation of differences, capturing the range where 95% of differences between methods fall.
- Trend analysis: Evaluation of whether differences between methods are consistent across the measurement range or exhibit proportional bias.
For continuous glucose monitors, for example, Bland-Altman analysis would quantify both the average deviation from reference blood glucose measurements and the range of expected differences during normal use [14] [69]. This provides clinicians with actionable information about the biosensor's reliability and limitations for making treatment decisions.
Implementation Protocol
The experimental protocol for implementing Bland-Altman analysis in biosensor validation requires meticulous study design and execution:
Paired Measurements: Collect synchronized measurements from the biosensor and gold standard method across the intended measurement range. For wearable biosensors, this includes spanning various activity states (resting, walking, post-exercise) [69].
Sample Size Considerations: Include sufficient participants and measurements to precisely estimate limits of agreement. While no universal sample size exists for Bland-Altman analysis, recent methodologies have improved precision in limits of agreement estimation.
Data Collection Protocol:
- Ensure time synchronization between biosensor and reference measurements [69]
- Cover the entire clinically relevant measurement range
- Include repeated measurements to assess consistency
- Document conditions that might affect performance (motion, temperature, skin tone)
Analysis Procedure:
- Calculate differences between paired measurements (biosensor - reference)
- Compute mean difference (bias) and standard deviation of differences
- Determine 95% limits of agreement (mean ± 1.96 × SD)
- Create Bland-Altman plot with differences versus averages of paired measurements
- Analyze relationship between differences and measurement magnitude
Clinical Interpretation: Evaluate whether the observed bias and limits of agreement fall within clinically acceptable boundaries based on intended use [69] [70].
Comparative Performance Data Across Biosensor Platforms
Table 3: Experimental Performance Data for Current Biosensor Technologies
| Biosensor Technology | Target Analyte | Sensitivity/ Performance | Specificity/ Selectivity | Sample Size in Validation | Statistical Methods Applied |
|---|---|---|---|---|---|
| SPR Biosensor with WS2 | Cancer cells (Jurkat) [30] | 342.14 deg/RIU [30] | FOM: 124.86 RIU⁻¹ [30] | Simulation-based | Electric field distribution analysis [30] |
| Enzyme-free Glucose Sensor | Glucose [14] | 95.12 ± 2.54 µA mM⁻¹ cm⁻² [14] | Excellent stability in interstitial fluid [14] | Not specified | Stability and sensitivity analysis [14] |
| SERS-based Immunoassay | α-Fetoprotein [14] | LOD: 16.73 ng/mL [14] | Not specified | Calibration curve | Linear range 500-0 ng/mL [14] |
| THz SPR Biosensor | Liquid and gas sensing [14] | 3.1043×10⁵ deg RIU⁻¹ (liquid) [14] | Phase sensitivity | Theoretical investigation | Phase sensitivity analysis [14] |
| Pre-equilibrium Biosensor | Insulin [72] | SNR-optimized kinetics [72] | Kinetic specificity [72] | Theoretical framework | Frequency domain analysis [72] |
Essential Research Reagent Solutions
Table 4: Key Research Reagents and Materials for Biosensor Development
| Reagent/Material | Function in Biosensor Development | Example Applications |
|---|---|---|
| Transition Metal Dichalcogenides (TMDCs) | Enhance plasmonic response and sensitivity [30] | SPR biosensors (e.g., WS₂, MoS₂) [30] |
| Au-Ag Nanostars | Provide intense plasmonic enhancement for SERS [14] | SERS-based immunoassays for cancer biomarkers [14] |
| Polydopamine/Melanin-like Materials | Surface modification with biocompatibility and adhesion properties [14] | Electrochemical sensors for environmental monitoring [14] |
| Specific Biorecognition Elements | Provide analytical specificity (antibodies, aptamers, nucleic acids) [15] | Lateral flow assays, immunosensors [15] |
| Nanoparticle Labels | Signal generation (colorimetric, fluorescent, electrochemical) [15] | Lateral flow immunoassays [15] |
| Specialized Membranes | Fluidics control in paper-based biosensors [15] | Lateral flow assays (nitrocellulose) [15] |
Integrated Experimental Protocol for Biosensor Validation
A comprehensive biosensor validation study integrates multiple statistical approaches to build a compelling evidence dossier for regulatory submission and investor confidence. The following protocol outlines a standardized methodology for generating comparable performance data:
Study Design Phase
- Define Intended Use: Precisely specify the clinical or analytical context, target population, and conditions of use.
- Select Appropriate Comparator: Choose the recognized gold standard method for comparison (e.g., 12-lead ECG for cardiac rhythm, clinical-grade pulse oximeter for SpO₂) [69].
- Establish Endpoint Hierarchy: Define primary, secondary, and exploratory endpoints with pre-specified performance targets.
- Sample Size Calculation: Implement exact sample size methods that account for correlation structure between endpoints and desired precision [71].
Data Collection Phase
- Participant Recruitment: Enroll participants representing the full spectrum of intended use (diverse skin tones, BMI ranges, age groups) [69].
- Measurement Protocol: Collect synchronized measurements under controlled and real-world conditions, documenting potential confounding factors.
- Blinded Assessment: Ensure objective endpoint adjudication without knowledge of biosensor results (e.g., cardiologist interpretation of ECGs) [69].
Statistical Analysis Phase
- Primary Endpoint Analysis: Calculate sensitivity/specificity with exact confidence intervals for diagnostic biosensors [69].
- Agreement Assessment: Implement Bland-Altman analysis to quantify measurement agreement with gold standard methods [70].
- Subgroup Analyses: Evaluate performance consistency across predefined participant subgroups and use conditions [69].
- Pre-specified Analysis Plan: Finalize all statistical approaches prior to data collection to minimize analytical bias.
This integrated protocol provides a standardized framework for generating comparable performance data across different biosensor platforms, enabling objective comparison of technological alternatives and supporting evidence-based adoption decisions.
Biosensors are powerful analytical devices that combine a biological recognition element with a physicochemical transducer to detect target analytes. The performance of these sensors is critical for applications ranging from clinical diagnostics and drug development to environmental monitoring and food safety. This guide provides a comparative performance analysis of three major biosensor platforms: Surface Plasmon Resonance (SPR), Electrochemical, and Wearable Biosensors. Framed within a broader thesis on biosensor evaluation, this article objectively compares these technologies based on sensitivity, specificity, and other key performance parameters, supported by experimental data and detailed methodologies. The analysis aims to equip researchers and drug development professionals with the information necessary to select appropriate biosensing platforms for their specific applications.
Performance Comparison at a Glance
The table below summarizes the key performance characteristics of SPR, Electrochemical, and Wearable biosensors, based on recent experimental studies.
Table 1: Comparative Performance of Major Biosensor Platforms
| Biosensor Type | Reported Sensitivity | Detection Limit | Linearity Range | Response Time | Key Applications Demonstrated |
|---|---|---|---|---|---|
| SPR Biosensors | 342.14 °/RIU (Blood cancer cells) [30]; 390 °/RIU (SARS-CoV-2) [74] | Not Specified | Not Specified | Real-time, label-free [74] | Viral detection (SARS-CoV-2) [74], Cancer cell detection (Jurkat, HeLa, Basal) [30] |
| Electrochemical Biosensors | 175.043 µA mM⁻¹ cm⁻² (GE/MnPc/GOx Glucose sensor) [75] | 0.0026 mM (GE/MnPc/GOx) [75] | 0.003–1.0 mM (GE/MnPc/GOx) [75] | Not Specified | Glucose sensing [75], Self-monitoring of blood glucose (SMBG) [76] |
| Wearable Biosensors | 95.12 ± 2.54 µA mM⁻¹ cm⁻² (Enzyme-free glucose sensor) [14] | Not Specified | Not Specified | Real-time, continuous [77] [78] | Sweat analysis (glucose, lactate, electrolytes, cortisol) [77], Athletic performance monitoring [77] |
Table 2: Comparison of Specificity, Advantages, and Limitations
| Biosensor Type | Specificity & Key Features | Major Advantages | Inherent Limitations |
|---|---|---|---|
| SPR Biosensors | High specificity via biorecognition elements (e.g., antibodies); Label-free detection [74] [30] | Very high sensitivity; Real-time, label-free monitoring of molecular interactions [74] [30] | Bulky instrumentation; Complex data interpretation; High cost [30] |
| Electrochemical Biosensors | Specificity from enzymes (e.g., GOx, FAD-GDH) or mediators [75] [76] | High sensitivity and selectivity; Portable; Low cost; Miniaturizable [75] [76] | Potential signal interference; Enzyme stability issues [75] |
| Wearable Biosensors | Multi-analyte detection; Specificity from integrated biorecognition elements [77] [78] | Non-invasive; Real-time, continuous monitoring; Comfortable, flexible designs [77] [78] | Signal noise from motion artifacts; Power management challenges; Biocompatibility requirements [79] |
Detailed Experimental Protocols and Methodologies
SPR Biosensor Experimental Setup
Objective: To achieve highly sensitive, label-free detection of specific analytes, such as viruses or cancer cells. Key Components: Prism (BK7, CaF₂), plasmonic metal layer (Ag, Au), 2D material coatings (BP, Graphene, WS₂), and a microfluidic chamber for sample delivery [74] [30].
Protocol:
- Sensor Chip Fabrication: A glass substrate is coated with a ~50 nm thick silver or gold film using sputtering or thermal evaporation. Selected 2D materials, such as WS₂ or graphene, are transferred onto the metal surface to form a heterostructure that enhances the local electric field [74] [30].
- Optical Configuration: The sensor chip is assembled in a Kretschmann configuration, where a polarized light source is directed through a coupling prism onto the metal film. The intensity of the reflected light is measured by a photodetector as a function of the incident angle [74].
- Sample Analysis: The analyte solution (e.g., viral particles, cancer cells) is injected over the sensor surface via a microfluidic system. Binding events on the sensor surface alter the local refractive index, causing a shift in the resonance angle (the angle at which reflected light intensity is minimum). This shift is monitored in real-time [30].
- Data Analysis: The sensor's sensitivity is calculated as the shift in resonance angle per unit change in refractive index (deg/RIU). Performance is also evaluated via the Figure of Merit (FOM), which considers the resonance angle shift and the width of the resonance curve [30].
Electrochemical Biosensor Fabrication and Measurement
Objective: To detect analyte concentration (e.g., glucose) with high sensitivity and a wide linear range via electrochemical signals. Key Components: Working electrode (e.g., Graphite Electrode - GE), water-soluble mediator (e.g., Quinoline-5,8-dione - QD), enzyme (e.g., FAD-GDH), and potentiostat [75] [76].
Protocol:
- Electrode Modification: The working electrode is drop-casted with a solution containing a water-soluble mediator (e.g., 0.1 mM QD) and enzyme (e.g., 0.008 mM FAD-GDH), then dried to form a thin film. This creates the biorecognition layer [76].
- Electrochemical Measurement: The modified electrode is exposed to analyte solutions of varying concentrations in an electrochemical cell. Amperometric or voltammetric measurements are performed. For instance, a constant potential is applied, and the resulting current is measured as the analyte is enzymatically converted, regenerating the mediator and producing a measurable faradaic current [75] [76].
- Calibration and Analysis: The measured current is plotted against analyte concentration to establish a calibration curve. Sensitivity (µA mM⁻¹ cm⁻²), linear range, and limit of detection (LOD) are determined from this curve. Finite Element Method (FEM) simulation can be used to visualize and confirm that the reaction is limited by substrate diffusion, which is ideal for a wide linear range [76].
Wearable Biosensor Validation and Testing
Objective: To enable non-invasive, continuous monitoring of biomarkers (e.g., in sweat) on a flexible, wearable platform. Key Components: Flexible substrate (e.g., polymer, textile), electrochemical or colorimetric sensing electrodes, microfluidic system for sweat collection, and wireless data transmission module [77] [78].
Protocol:
- Sensor Fabrication: Sensing electrodes (e.g., for lactate or glucose) are fabricated on a flexible polymer substrate (e.g., PDMS) using techniques like screen-printing with conductive inks. A biorecognition element (e.g., enzyme) is immobilized on the electrode surface. A microfluidic channel may be incorporated to guide sweat to the sensing area [78].
- On-Body Validation: The sensor is adhered to the skin of human volunteers (e.g., forearm). Sweat is naturally stimulated or induced via iontophoresis. The sensor operates continuously, generating an electrochemical (e.g., amperometric) or optical signal proportional to the biomarker concentration [77].
- Data Acquisition and Benchmarking: The sensor's signal is transmitted wirelessly (e.g., via Bluetooth) to a smartphone or computer. The performance (e.g., sensitivity, stability) is validated by comparing the sensor's readings with gold-standard laboratory methods (e.g., HPLC analysis of simultaneously collected sweat samples) [77] [78].
Biosensor Working Principles and Signaling Pathways
The following diagrams illustrate the fundamental working principles and signal transduction pathways for each biosensor type.
SPR Biosensor Principle
Electrochemical Biosensor Principle
Wearable Biosensor System
Research Reagent Solutions and Essential Materials
This section details key reagents and materials critical for the fabrication and function of the biosensors discussed.
Table 3: Essential Research Reagents and Materials for Biosensor Development
| Item Name | Function/Application | Specific Examples & Notes |
|---|---|---|
| 2D Materials | Enhance sensitivity in SPR sensors by increasing light-matter interaction and electric field intensity [74] [30]. | Graphene, Black Phosphorus (BP), Transition Metal Dichalcogenides (TMDCs) like MoS₂, WS₂, WSe₂ [74] [30]. |
| Water-Soluble Mediators | Shuttle electrons between the enzyme's active site and the electrode surface in electrochemical biosensors [75] [76]. | Quinoline-5,8-dione (QD), quaternized phthalocyanines (e.g., MnPc, CuPc). Offer high enzyme reactivity and water solubility [75] [76]. |
| Plasmonic Metal Films | Generate surface plasmon waves when excited by light in SPR biosensors [74] [80]. | Silver (Ag) and Gold (Au); typically coated as thin films (~50 nm) on a prism [74] [30]. |
| Enzymes (Biorecognition) | Provide high specificity by catalyzing a reaction involving the target analyte [75] [76]. | Glucose Oxidase (GOx), FAD-dependent Glucose Dehydrogenase (FAD-GDH). FAD-GDH is oxygen-insensitive [75] [76]. |
| Flexible Substrates | Serve as the base for wearable sensors, providing comfort and conformability to the skin [77] [78]. | Polydimethylsiloxane (PDMS), Polyethylene, and smart textiles integrated with conductive fibers [78]. |
| Ultrasmall Nanoparticles | Act as signal amplifiers to enhance sensitivity in various biosensing platforms [80]. | BSA-templated Au, Ag, or Au/Ag nanoparticles (1–3 nm). Improve signal by increasing mass and optical effects [80]. |
The evolution of biosensor technologies presents a dual challenge for researchers and drug development professionals: achieving stringent regulatory compliance while ensuring equitable performance across diverse human populations. Regulatory frameworks, particularly those established by the International Organisation for Standardisation (ISO), provide the foundational requirements for medical device safety, quality, and efficacy [81]. Concurrently, growing evidence demonstrates that performance disparities across different skin tones can compromise diagnostic accuracy and therapeutic outcomes, raising critical equity concerns [82] [83]. This comparison guide examines the intersection of these two domains by analyzing key ISO standards relevant to biosensor development and evaluating experimental approaches for validating performance across the full spectrum of skin pigmentation. Within the broader context of biosensor sensitivity and specificity research, this analysis aims to provide a structured framework for developing devices that are both commercially viable and clinically equitable, with particular emphasis on optical biosensors whose performance is inherently influenced by skin melanin content.
Essential ISO Standards for Biosensor Regulation
For biosensors classified as medical devices, conformity with internationally recognized standards is mandatory for market approval and commercial deployment. These standards establish comprehensive frameworks for quality management, risk assessment, and software validation throughout the product lifecycle.
Table 1: Key ISO and IEC Standards for Biosensor Development and Approval
| Standard Number | Title | Scope and Purpose | Relevance to Biosensors |
|---|---|---|---|
| ISO 13485:2016 | Medical Devices - Quality Management Systems - Requirements for Regulatory Purposes | Establishes requirements for a comprehensive quality management system throughout the device lifecycle [81]. | Mandatory for manufacturers; requires formal audit and certification to demonstrate consistent design, production, and installation of medical devices [81]. |
| ISO 14971:2019 | Application of risk management to medical devices | Provides a framework for identifying, evaluating, and mitigating risks associated with medical devices [81]. | Essential for classifying device risk, considering potential harm from foreseeable use, and implementing safety mitigations [81]. |
| IEC 62304:2006+A1:2015 | Medical Device Software - Software Life Cycle Processes | Defines life cycle processes for medical device software, including development, validation, and maintenance [81]. | Critical for software-dependent biosensors; ensures robust validation and testing of each software component [81]. |
| IEC 62366-1:2015 | Medical Devices - Application of Usability Engineering to Medical Devices | Specifies a process for analyzing, designing, developing, and validating usability as related to device safety [81]. | Ensures biosensors are designed for safe use by intended users in the intended use environment, minimizing use errors [81]. |
| ISO 14155:2020 | Clinical investigation of medical devices for human subjects - Good clinical practice | Provides guidelines for the design, conduct, recording, and reporting of clinical investigations [81]. | Governs the collection of clinical performance data, including data across diverse patient populations, required for regulatory submissions [81]. |
The standards highlighted in Table 1 represent the core regulatory framework, with ISO 13485 and ISO 14971 forming the foundation of device quality and safety. These standards require manufacturers to establish processes for tracking changes to devices and internal procedures, with ISO 13485 requiring formal audit and maintained certification [81]. The risk management process outlined in ISO 14971 is particularly relevant for addressing performance variations across skin tones, as it requires manufacturers to consider potential harms resulting from foreseeable interactions between the patient and device [81].
For software-driven biosensors, IEC 62304 provides critical guidance for validating each software component to ensure proper integration and function within larger systems [81]. This standard works in concert with IEC 62366-1, which focuses on usability engineering to minimize use errors that could compromise safety. Finally, ISO 14155 aligns with Good Clinical Practice principles and provides a comprehensive structure for designing studies that generate valid clinical evidence, including the need for representative participant populations in clinical investigations [81].
Skin Tone Bias in Optical Biosensing: Mechanisms and Evidence
Optical biosensors, particularly those utilizing photoplethysmography (PPG), demonstrate measurable performance variations across different skin tones due to fundamental differences in light-tissue interaction. Melanin, the primary chromophore responsible for skin pigmentation, absorbs light in the visible spectrum, with particularly strong absorption in the blue-green wavelengths (460-570 nm) commonly used in PPG sensors [82] [84]. This differential absorption creates significant signal-to-noise challenges in darker skin tones, leading to potential inaccuracies in physiological measurements.
Table 2: Documented Performance Variations of Optical Biosensors Across Skin Tones
| Study Focus | Experimental Design | Key Findings | Implications |
|---|---|---|---|
| Smartwatch Heart Rate Monitoring [82] | Evaluation of PPG-based smartwatches across skin tones during rest and exercise (n=75). | Some WearOS devices underestimated heart rate by 10-15 bpm in darker-skinned users during vigorous activity (p < 0.01). Apple Watch showed <5 bpm variation across skin tones. | Device selection matters; some commercial sensors show significant skin-tone-dependent bias, particularly during dynamic physiological states. |
| Reflectance Spectroscopy [84] | White light (300-700 nm) reflectance measured on inner wrist of 12 participants with evenly distributed skin tones. | Peak reflected light amplitude decreased by 90% for darker skin tones vs. 70% for lighter tones. Distinct differences in reflectance at 460 nm and 570 nm wavelengths between groups. | Melanin concentration significantly affects light reflection and absorption profiles, potentially compromising measurements based on fixed algorithms. |
| Pulse Oximetry Accuracy [84] | Clinical validation of SpO₂ measurements against arterial blood gas in 749 dark-toned and 2,778 light-toned patients. | 11.7% of dark-toned patients vs. 3.6% of light-toned patients were misdiagnosed as having normal SpO₂ (92-96%) while actually experiencing hypoxemia. | Clinical consequences are significant; inaccurate readings can lead to missed diagnoses and inadequate treatment in darker-skinned patients. |
The empirical evidence summarized in Table 2 demonstrates that skin tone significantly affects optical biosensor performance. The reflectance spectroscopy study revealed that darker skin tones reflect less light overall and exhibit distinctly different spectral profiles, particularly in the indigo-blue (460 nm) and yellow-orange (570 nm) bands [84]. These findings suggest that the standard approach of using fixed wavelengths and algorithms without skin tone calibration may be insufficient for accurate measurements across diverse populations.
The clinical implications are substantial, as demonstrated by the pulse oximetry data showing that nearly 12% of dark-skinned patients with abnormally low blood oxygen were misclassified as normal using standard PPG-based devices [84]. This measurement error stems from the fundamental physics of light-tissue interaction: since SpO₂ is calculated using the ratio (R) of absorptivity of red and infrared light, the decreased DC component in darker skin due to melanin absorption artificially lowers the R value, resulting in overestimated oxygen saturation readings [84].
Methodologies for Validating Performance Across Skin Tones
Skin Tone Classification Systems
Robust validation of biosensor performance requires standardized, reproducible methods for classifying skin tone. Currently, two primary classification systems are used in research and clinical validation:
Fitzpatrick Skin Type (FST) Scale: A 6-point scale (I-VI) originally developed to classify sun sensitivity [83]. Despite its widespread use, FST has limitations for biosensor validation as it was not originally designed for pigment-based classification and relies on subjective self-reporting or assessment [83].
Monk Scale: A 10-shade scale developed as a more inclusive alternative to FST, with improved representation of diverse skin tones [83] [84]. While an improvement, it still faces validation challenges and subjective interpretation.
Recent research has revealed significant discrepancies between self-reported and annotator-assessed skin tones using both scales. One study found that annotators consistently assigned lighter skin tones than patients' self-reports, with strong negative correlations between self-reported scores and annotator-patient differences (Spearman's ρ = -0.82 for Fitzpatrick, -0.84 for Monk) [83]. This highlights the subjectivity inherent in these classification systems and their potential limitations for rigorous scientific validation.
Objective Spectrophotometric Methods
To address the limitations of subjective scales, researchers are increasingly adopting objective, instrument-based methods:
Experimental Protocol: CIE XYZ Color Space Measurement [84]
Participant Selection: Recruit participants with even distribution across the skin tone spectrum. Sample size calculations should ensure adequate statistical power for detecting clinically significant differences.
Instrumentation: Use a calibrated spectrophotometer with a white light source (300-700 nm) and standardized detection geometry. The study used an AvaSpec 2048 Spectrometer with CC-VIS/NIR cosine corrector [84].
Measurement Conditions: Conduct measurements in a controlled environment with stable temperature (19.5-20.5°C recommended) and minimal ambient light. Clean measurement sites (typically inner wrist) with alcohol wipes to remove contaminants [84].
Standardized Positioning: Maintain consistent sensor-skin distance (1 cm used in reference study) and pressure using a 3D-printed housing to ensure reproducibility [84].
Data Analysis: Convert raw spectral data to CIE XYZ color coordinates, which provide device-independent values for objective skin tone classification and stratification of biosensor performance.
Integrated Framework for Regulatory Compliance and Equity
Developing biosensors that meet both regulatory requirements and equity considerations requires a systematic approach that integrates these considerations throughout the product lifecycle. The following workflow illustrates the essential stages for achieving this integration:
This integrated framework aligns with the "total product lifecycle" approach advocated by regulatory bodies for AI/ML-enabled devices [85]. It begins with formal identification of skin tone as a potential risk factor during the risk management process required by ISO 14971, followed by proactive mitigation through inclusive design principles [81]. The validation stage requires rigorous testing across diverse populations using objective skin tone classification, with comprehensive documentation of subgroup performance for regulatory submission. Finally, post-market surveillance monitors real-world performance across demographics, with significant disparities potentially reported as adverse events.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Materials for Biosensor Development and Validation
| Item | Specification/Example | Primary Function | Considerations for Equity-Focused Research |
|---|---|---|---|
| Spectrophotometer | AvaSpec 2048 with CC-VIS/NIR cosine corrector [84] | Objective measurement of skin reflectance properties | Provides quantitative, device-independent skin tone data superior to subjective scales |
| CIE XYZ Color Standards | Calibrated reference tiles | Instrument calibration and measurement standardization | Ensures consistency across study sites and longitudinal measurements |
| Optical Biosensor Platform | Customizable systems with multiple wavelength capabilities | Prototype development and signal optimization | Enables testing of alternative wavelengths less affected by melanin absorption |
| Skin Tone Classification Scales | Fitzpatrick (I-VI), Monk (1-10) [83] [84] | Participant stratification and comparison with literature | Recognize limitations of subjective assessment; use multiple independent annotators |
| Data Analysis Software | Python with spectral analysis libraries (e.g., SciPy, NumPy) | Processing spectral data and performing statistical analysis | Implement tests for significant performance differences across skin tone subgroups |
| Quality Management System | ISO 13485:2016 compliant [81] | Documentation of design controls and validation protocols | Required for regulatory approval; ensures consistent processes for equity considerations |
This toolkit enables researchers to implement the methodologies described throughout this guide, with particular emphasis on objective measurement and standardized validation protocols. The spectrophotometer serves as the cornerstone for objective skin tone characterization, while customizable biosensor platforms allow investigation of hardware solutions to mitigate melanin-related interference. The inclusion of a formal Quality Management System aligned with ISO 13485 ensures that equity considerations are systematically documented and integrated into the development process rather than treated as an afterthought [81].
Meeting regulatory standards and ensuring equitable performance across skin tones are complementary rather than competing objectives in biosensor development. ISO standards provide the necessary framework for demonstrating safety and efficacy, while comprehensive validation across diverse populations represents both an ethical imperative and a marker of technological maturity. The experimental approaches and comparative data presented in this guide provide researchers with methodologies to address both requirements simultaneously, with particular attention to optical biosensors whose fundamental operating principles are influenced by skin pigmentation. As regulatory bodies increasingly focus on algorithmic bias and health equity, the integration of these considerations throughout the product lifecycle will become essential for successful technology translation and regulatory approval. Future research should prioritize the development of standardized protocols for objective skin tone measurement and the exploration of novel sensing modalities less susceptible to melanin-related interference, ultimately advancing the field toward more inclusive and effective biosensing technologies.
Conclusion
The evaluation of biosensor sensitivity and specificity is a multifaceted process that integrates foundational physics, advanced materials science, and data-driven optimization. The convergence of sophisticated sensing modalities like SPR with AI and machine learning is paving the way for unprecedented sensitivity, capable of detecting targets down to the single-molecule level. Future progress hinges on the successful translation of these advanced platforms from controlled laboratory settings into robust, clinically validated tools. This will require standardized validation protocols, a focus on equitable performance across diverse populations, and seamless integration with point-of-care and wearable formats. The ongoing innovation in this field promises to redefine personalized medicine, environmental monitoring, and biomanufacturing by providing reliable, real-time analytical data.
References
- 1. Biosensors Metrics Glossary of Definitions - Zimmer & Peacock [https://www.zimmerpeacocktech.com/knowledge-base/faq/biosensors-glossary/]
- 2. Detection limit [https://en.wikipedia.org/wiki/Detection_limit]
- 3. Introduction to biosensors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4986445/]
- 4. Evaluation of SARS-CoV-2 lateral flow device sensitivity [https://pmc.ncbi.nlm.nih.gov/articles/PMC12496196/]
- 5. Evaluation of the Analytical Sensitivity of a Molecular Point ... [https://pubmed.ncbi.nlm.nih.gov/40248900/]
- 6. When lower isn't always better in biosensor research and ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566324006766]
- 7. Startup's biosensor makes drug development and ... [https://news.mit.edu/2025/startup-biosensor-makes-drug-development-and-manufacturing-cheaper-0615]
- 8. Nanowire Biosensors Could Slash Drug Development Costs [https://www.asme.org/topics-resources/content/nanowire-biosensors-could-slash-drug-development-costs]
- 9. Advanced SPR biosensor with optimized gold-TiO2 D ... [https://www.nature.com/articles/s41598-025-24697-y]
- 10. Design optimization of high-sensitivity PCF-SPR biosensor ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0330944]
- 11. Machine learning-enhanced SPR-based optical biosensor ... [https://www.sciencedirect.com/science/article/abs/pii/S0030399225013878]
- 12. High-sensitivity biosensors based on reflection-type guided ... [https://www.sciencedirect.com/science/article/abs/pii/S0925400525003843]
- 13. Next-generation COVID-19 detection using a metasurface ... [https://www.nature.com/articles/s41598-025-18753-w]
- 14. Biosensors, Volume 15, Issue 9 (September 2025) [https://www.mdpi.com/2079-6374/15/9]
- 15. Review Biosensors and lateral flow immunoassays [https://www.sciencedirect.com/science/article/abs/pii/S0009898125001512]
- 16. Plasmonic Biosensors: Review - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9138269/]
- 17. Enhanced sensitivity and figure of merit in surface plasmon ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25006964]
- 18. 2D nanomaterials in biosensing: Synthesis ... [https://www.sciencedirect.com/science/article/pii/S2590137025000421]
- 19. 2D Materials in Advanced Electronic Biosensors for Point‐ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11336981/]
- 20. High performance SPR sensor using 2-D materials [https://www.sciencedirect.com/science/article/abs/pii/S0924424724001523]
- 21. Recent Advances in Developing Cell-Free Protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12385134/]
- 22. Emerging trends in AI-integrated optical biosensors for point ... [https://pubs.rsc.org/en/content/articlehtml/2025/cc/d5cc04899k]
- 23. The Role of Artificial Intelligence in Advancing Biosensor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12392873/]
- 24. Engineering biosensing platforms for rapid and accurate ... [https://www.sciencedirect.com/science/article/abs/pii/S095656632500822X]
- 25. Plasmonic coffee-ring biosensing for AI-assisted point-of- ... [https://www.nature.com/articles/s41467-025-59868-y]
- 26. New Biosensors Could Revolutionize Cancer Detection [https://www.gatech.edu/news/2025/01/13/new-biosensors-could-revolutionize-cancer-detection]
- 27. Machine learning-based prediction and interpretation of ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25030048]
- 28. Advances in PCF-SPR sensors: a comprehensive review of ... [https://www.sciencedirect.com/science/article/abs/pii/S0263224125025850]
- 29. Recent Advances in Photonic Crystal Fiber-Based SPR ... [https://www.mdpi.com/2072-666X/16/7/747]
- 30. On the sensing performance improvement in SPR ... [https://www.nature.com/articles/s41598-025-14131-8]
- 31. A highly optimized and sensitive bowtie shape-based SPR ... [https://pubs.rsc.org/en/content/articlehtml/2025/na/d4na00812j]
- 32. Highly sensitive V-shaped SPR PCF biosensor for cancer ... [https://link.springer.com/article/10.1007/s11082-023-04740-w]
- 33. Design optimization of high-sensitivity PCF-SPR biosensor ... [https://pubmed.ncbi.nlm.nih.gov/40953064/]
- 34. High-performance surface plasmon resonance fiber sensor ... [https://www.nature.com/articles/s41598-023-31524-9]
- 35. Device integration of electrochemical biosensors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9951169/]
- 36. Technological advances in electrochemical biosensors for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8396145/]
- 37. Electrochemical protein biosensors for disease marker ... [https://www.nature.com/articles/s41378-024-00700-w]
- 38. A wearable electrochemical biosensor for the monitoring of ... [https://www.nature.com/articles/s41551-022-00916-z]
- 39. Advanced SPR biosensor with optimized gold-TiO2 D- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12635218/]
- 40. Microfluidic biosensors for biomarker detection in body fluids [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-024-00697-4]
- 41. Understanding the Landscape of Multi-Cancer Detection ... [https://www.mdpi.com/2075-1729/14/7/896]
- 42. Advances in electrochemical biosensing of esophageal ... [https://www.sciencedirect.com/science/article/pii/S1452398125001919]
- 43. Biosensors based on cell-free synthetic expression for ... [https://www.sciencedirect.com/science/article/abs/pii/S1385894724071237]
- 44. Advances in Smart Biosensors for Real-Time Pollutant ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993625003516]
- 45. Engineering biology applications for environmental solutions [https://www.nature.com/articles/s41467-025-58492-0]
- 46. A Review on the Application of Biosensors for Monitoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12390133/]
- 47. Point-of-care biosensors for infectious disease diagnosis [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03897a?page=search]
- 48. Machine learning-based optimization for D-shaped PCF ... [https://www.sciencedirect.com/science/article/abs/pii/S0030401824010411]
- 49. Machine Learning Approach to Develop a Novel Multi ... [https://www.mdpi.com/2076-3417/11/2/835]
- 50. An improved multi-objective particle swarm optimization ... [https://www.nature.com/articles/s41598-025-87350-8]
- 51. Improved Adaptive Multi-Objective Particle Swarm ... [https://www.mdpi.com/1424-8220/22/14/5203]
- 52. Sensitivity studies and optimization of an impedance- ... [https://www.sciencedirect.com/science/article/pii/S2590137024000438]
- 53. Development and performance characteristics evaluation of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8051012/]
- 54. Algorithm assisted comprehensive optimization of SPR ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566325007225]
- 55. On the sensing performance improvement in SPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12322250/]
- 56. Nanocomposite biosensor tracks honokiol-induced ... [https://www.nature.com/articles/s41378-025-01016-z]
- 57. Simultaneous detection of inflammatory process indicators via... [https://www.oejournal.org/oes/article/doi/10.29026/oes.2025.250005]
- 58. Addressing Signal Drift and Screening for Detection of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12327215/]
- 59. Methods of Protection of Electrochemical Sensors against ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10831843/]
- 60. Recent Advances in Antifouling Materials for Surface ... [https://www.mdpi.com/2073-4360/13/12/1929]
- 61. eXplainable Artificial Intelligence (XAI): A Systematic ... [https://www.mdpi.com/1424-8220/25/21/6649]
- 62. Survey of explainable artificial intelligence techniques for ... [https://www.sciencedirect.com/science/article/pii/S0010482523001336]
- 63. Advancement of machine learning algorithms in biosensors [https://www.sciencedirect.com/science/article/abs/pii/S000989812500556X]
- 64. On the application of explainable AI in optimizing ... [https://www.sciencedirect.com/science/article/abs/pii/S1068520024001469]
- 65. Design optimization of high-sensitivity PCF-SPR biosensor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12435684/]
- 66. Comparing Randomized Controlled Trials and Real-World ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7276323/]
- 67. Analytical Methods for Comparing Uncontrolled Trials With ... [https://www.sciencedirect.com/science/article/pii/S1098301524028420]
- 68. Leveraging biosensors in clinical and research settings [https://www.nature.com/articles/s44277-025-00037-w]
- 69. Clinical Validation of Biosensors: Protocols That Investors ... [https://medstartups.org/clinical-validation-biosensors-protocols-investors-expect]
- 70. The potential of the Bland-Altman method in chemical ... [https://www.sciencedirect.com/science/article/pii/S1026918525001088]
- 71. Exact power and sample size in clinical trials with two co- ... [https://pubmed.ncbi.nlm.nih.gov/40879443/]
- 72. Pre-equilibrium biosensors as an approach towards rapid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9674706/]
- 73. Sample Size Requirements for Calibrated Approximate ... [https://www.mdpi.com/1660-4601/18/2/595]
- 74. A performance comparison of heterostructure surface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10039361/]
- 75. Synthesis and comparison of the performance of two ... [https://www.sciencedirect.com/science/article/pii/S1567539424001506]
- 76. Insights into the performance-determining aspects of ... [https://pubs.rsc.org/en/content/articlehtml/2025/sd/d5sd00095e]
- 77. Advanced Wearable Devices for Monitoring Sweat ... [https://pubmed.ncbi.nlm.nih.gov/39727839/]
- 78. Advances in Wearable Biosensors for Healthcare [https://www.mdpi.com/2079-6374/14/11/560]
- 79. Comparison of Wearable Biosensors in Medical vs. Sports ... [https://eureka.patsnap.com/report-comparison-of-wearable-biosensors-in-medical-vs-sports-applications]
- 80. Performance comparison of surface plasmon resonance ... [https://www.sciencedirect.com/science/article/pii/S0026265X19332667]
- 81. The ISO standards you need to know for SaMD - 2025 update [https://www.hardianhealth.com/insights/iso-standards-for-software-medical-device]
- 82. Photoplethysmography in Diverse Skin Tones [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592569/]
- 83. Validity of two subjective skin tone scales and its ... [https://www.nature.com/articles/s41746-025-01975-7]
- 84. Towards a Wearable Skin Tone Responsive Optical Sensor [https://www.mdpi.com/2673-4591/109/1/17]
- 85. Key Regulatory Trends Shaping 2025 [https://www.regdesk.co/blog/key-regulatory-trends-shaping-2025/]