Strategies for Troubleshooting and Minimizing False Positives in Biosensor Assays
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on identifying, troubleshooting, and preventing false positives in biosensor assays.
Strategies for Troubleshooting and Minimizing False Positives in Biosensor Assays
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on identifying, troubleshooting, and preventing false positives in biosensor assays. Covering foundational principles to advanced technological integrations, it explores the multifaceted origins of false signals—from bioreceptor selection and sample matrix effects to transducer limitations. The content details systematic troubleshooting workflows, highlights the role of machine learning and dual-mode sensing for enhanced validation, and offers comparative analyses of optimization strategies. By synthesizing current research and practical methodologies, this resource aims to equip professionals with the knowledge to improve assay robustness, reliability, and clinical translatability.
Understanding the Core Principles and Common Pitfalls of Biosensor Assays
Defining Biosensor Components and Their Role in Signal Generation
Frequently Asked Questions
What are the core components of a biosensor? A biosensor is a self-contained analytical device consisting of five main components [1]:
- Analyte: The specific substance targeted for detection (e.g., glucose, a virus, or a protein biomarker).
- Bioreceptor: A biological element (e.g., enzyme, antibody, aptamer, or nucleic acid) that specifically recognizes and binds to the analyte. This interaction is called biorecognition.
- Transducer: The part that converts the biorecognition event into a measurable signal (e.g., optical or electrical). This energy conversion is called signalization [1].
- Electronics: The circuitry that processes the transducer's signal (e.g., amplifying it or converting it from analog to digital).
- Display: The interface that presents the final result in a user-comprehensible format, such as a numerical value or graph on a screen [1].
Why is understanding biosensor components critical for troubleshooting false positives? False positives occur when a biosensor indicates the presence of a target analyte when it is not actually there. The root cause of such errors can almost always be traced to a problem or interference at one of the core components [1]:
- Bioreceptor Issues: Loss of specificity, for instance from antibody cross-reactivity with similar molecules in a sample, can lead to false signals.
- Transducer & Electronics Issues: Environmental interference, electrical noise, or signal drift can be misinterpreted as a positive result.
- Overall System Design: Inadequate shielding from complex sample matrices (like blood or serum) can cause non-specific adsorption onto the sensor surface, generating a false signal.
What are some emerging technologies to reduce false results? Researchers are developing advanced biosensor designs to improve reliability:
- Dual-Modality Biosensors: These sensors integrate two independent detection methods (e.g., electrochemical and optical) into a single device. The two signals can cross-validate each other, significantly reducing the risk of false positives and negatives [2].
- Bio-Inspired Protection: New designs, like the SENSBIT system, mimic the human gut's protective mechanisms. A 3D nanoporous gold surface and a protective polymer coating shield the sensitive bioreceptor from interference and degradation in complex environments like flowing blood, enhancing signal stability and reliability [3].
- AI-Enhanced Biosensors: Artificial intelligence algorithms can process complex data from biosensors to identify patterns and distinguish specific signals from background noise, though they also require careful validation to avoid new sources of error from biased data or algorithms [1].
Troubleshooting Guide: False Positives
This guide helps you systematically diagnose and address the causes of false positive results. The following table outlines common issues and their solutions related to each biosensor component.
Table 1: Troubleshooting False Positives by Biosensor Component
| Faulty Component | Potential Cause of False Positive | Troubleshooting & Resolution Steps |
|---|---|---|
| Bioreceptor | Cross-reactivity with non-target molecules in the sample matrix [1]. | • Validate bioreceptor specificity against a panel of structurally similar interferents.• Switch to a higher-affinity or more specific bioreceptor (e.g., an aptamer). |
| Transducer | Non-specific adsorption of molecules to the transducer surface, generating a signal [4]. | • Improve the antifouling properties of the sensor interface with coatings like polyethylene glycol (PEG) or melanin-like polydopamine [5] [4].• Use a ratiometric measurement technique that internally corrects for background drift [4]. |
| Sample & Assay | Interfering substances in the complex sample matrix (e.g., proteins in blood) [4]. | • Dilute the sample or implement a sample purification/pre-treatment step.• Use standard addition methods to account for matrix effects. |
| System Design | Inability to self-validate the result due to a single measurement modality [2]. | • Adopt a dual-modality biosensor design that uses two different physical principles (e.g., electrochemical and optical) to detect the same analyte, providing built-in cross-validation [2]. |
Experimental Protocols for Diagnosis
Protocol 1: Validating Specificity via Cross-Reactivity Screening Purpose: To confirm that your biosensor's bioreceptor does not respond to molecules structurally related to your target analyte. Materials: Purified target analyte, structurally similar potential interferents, biosensor, buffer. Procedure:
- Prepare separate solutions of your target analyte and each potential interferent at physiologically relevant concentrations.
- Measure the biosensor's response to the buffer alone (blank).
- Measure the response to each interferent solution individually.
- Compare the signal generated by the interferents to the signal from the target. A significant response to an interferent indicates cross-reactivity. Interpretation: A specific biosensor should show a strong signal only for the target analyte and negligible signals for interferents.
Protocol 2: Assessing Matrix Effects with Standard Addition Purpose: To determine if components of the sample matrix itself are contributing to the false positive signal. Materials: Test sample (e.g., serum, blood), purified target analyte, buffer. Procedure:
- Measure the biosensor's response to the unspiked sample (this is your background signal).
- Spike the sample with a known, low concentration of the purified target analyte.
- Measure the biosensor's response to the spiked sample.
- Calculate the recovery:
(Measured concentration in spiked sample - Measured concentration in unspiked sample) / Known spiked concentration * 100%. Interpretation: A recovery value significantly different from 100% indicates substantial matrix interference, which may be causing false positives [6].
The Scientist's Toolkit: Key Reagent Solutions
The following table details essential materials used in modern biosensor development and troubleshooting.
Table 2: Key Research Reagents and Materials for Biosensor Development
| Item | Function in Biosensor Development | Specific Example & Application |
|---|---|---|
| Aptamers | Synthetic single-stranded DNA or RNA molecules that act as bioreceptors; offer high specificity and stability [5]. | Used for detecting hazards in food; can be selected via SELEX to bind diverse targets from small molecules to whole cells [5]. |
| Nanoporous Gold Electrodes | A nanostructured material providing a high surface area for bioreceptor immobilization, enhancing signal strength and stability [3]. | Used as a 3D scaffold in the SENSBIT system to protect molecular recognition elements and enable long-term monitoring in blood [3]. |
| Organic Electrochemical Transistors (OECTs) | Signal transducers that provide massive signal amplification (1000-7000x) and improve the signal-to-noise ratio [7]. | Used to amplify weak signals from enzymatic or microbial fuel cells for highly sensitive detection of targets like lactate or arsenite [7]. |
| Melanin-like Coatings (e.g., Polydopamine) | Versatile, biocompatible coatings that improve surface adhesion and provide antifouling properties [5]. | Used to modify electrode surfaces, reducing non-specific binding in environmental and food monitoring sensors [5]. |
| CRISPR/Cas Systems | Provides an enzymatic mechanism for signal amplification, enabling extremely high sensitivity and specificity for nucleic acid detection [4]. | Integrated into lateral flow assays for attomolar-level detection of viral genomic DNA or RNA, as demonstrated during the COVID-19 pandemic [4]. |
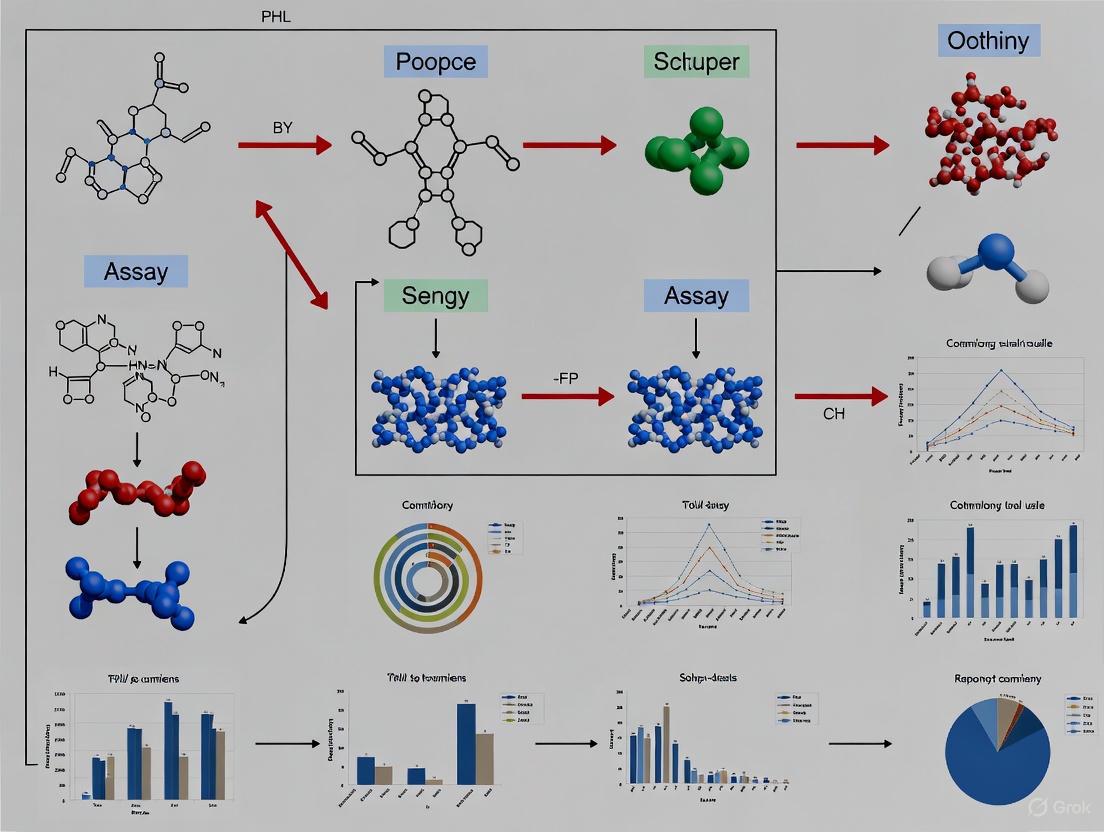
Technical Diagrams
Diagram 1: Biosensor Core Components and False Positive Triggers
This diagram illustrates the signal flow through the core components of a biosensor and pinpoints where specific failures can lead to a false positive result.
Diagram 2: Dual-Modality Biosensor Cross-Validation Workflow
This workflow shows how a dual-modality biosensor provides built-in cross-validation. An interferent may trigger one signal path, but the lack of a corresponding signal from the second, independent path flags the result as a potential false positive.
Systematic Classification of False Positive Triggers and Root Causes
False positive results present a significant challenge in biosensor applications, potentially leading to incorrect diagnostic, environmental, or research conclusions. Understanding their triggers and root causes is essential for developing robust analytical systems. False positives occur when a biosensor incorrectly indicates the presence of a target analyte, and they can arise from multiple sources including biological recognition elements, transducer systems, sample matrix effects, and operational protocols [1].
The COVID-19 pandemic highlighted the critical implications of false results in diagnostic systems, underscoring that no diagnostic tool is infallible [1]. Both conventional and AI-powered biosensors remain susceptible to these inaccuracies, which can stem from various causes including cross-reactivity, environmental interference, signal noise, calibration difficulties, and non-specific binding events [1] [2].
Classification of False Positive Triggers
Biological Recognition Elements
Biological recognition elements form the foundation of biosensor specificity, yet they represent a primary source of false positive triggers.
Antibody-Based Recognition Issues: Antibodies, while highly specific, can generate false positives through several mechanisms. Cross-reactivity with structurally similar molecules represents a major concern, particularly when antibodies bind to epitopes shared among different analytes. Batch-to-batch variability in antibody production can also lead to inconsistent sensitivity and specificity between production lots. Furthermore, degradation of antibodies during storage or use compromises their binding specificity, potentially increasing non-specific interactions [8].
Nucleic Acid Recognition Challenges: DNA-based recognition systems, including hybridization probes and aptamers, face distinct false positive triggers. Non-specific hybridization can occur when probe sequences interact with partially complementary targets under suboptimal hybridization conditions. The susceptibility of DNA to nuclease degradation in complex sample matrices can generate fragments that produce detectable signals. Additionally, variations in temperature, pH, or ionic strength significantly impact hybridization efficiency and specificity [8].
Enzyme-Related False Positives: Enzyme-based biosensors can produce false positives when endogenous enzymes in samples catalyze similar reactions to the recognition enzyme, or when sample components interfere with the enzymatic reaction. Enzymes also require strict environmental control, particularly precise temperature regulation, to maintain catalytic specificity [8].
Table: Classification of False Positives by Biological Recognition Element
| Recognition Element | Primary False Positive Triggers | Common Analytical Contexts |
|---|---|---|
| Antibodies | Cross-reactivity, Batch variability, Degradation | Clinical diagnostics, Food safety |
| Nucleic Acids | Non-specific hybridization, Degradation, Suboptimal conditions | Genetic testing, Pathogen detection |
| Enzymes | Interfering substrates, Environmental sensitivity, Endogenous enzymes | Metabolite monitoring, Environmental sensing |
Transducer and Signal Generation Mechanisms
The transducer component converts biological recognition events into measurable signals, and its limitations constitute another major category of false positive sources.
Optical Biosensor Artifacts: In surface plasmon resonance (SPR) systems, non-specific adsorption of materials to the sensor surface can generate signals indistinguishable from specific binding events. Contamination of optical components or light source instability may create baseline drift or spurious signals. For fluorescence-based systems, autofluorescence from sample components or container materials can produce background signals misinterpreted as positive results [9] [10].
Electrochemical Biosensor Interferences: Electroactive compounds present in samples can undergo oxidation or reduction at electrode surfaces, generating currents mistaken for target detection. Electrode fouling through protein adsorption or other matrix components alters electrode properties and response characteristics. Additionally, reference electrode potential drift leads to miscalibration and incorrect signal interpretation [2] [8].
Piezoelectric and Thermal Transducers: Mass-based sensors like cantilevers respond non-specifically to viscosity changes or non-target adsorption. Thermal biosensors detect heat from non-specific biochemical reactions or environmental temperature fluctuations [11].
Sample Matrix and Environmental Factors
Complex sample matrices introduce numerous interferents that can trigger false positive responses across various biosensor platforms.
Table: Sample Matrix Interferents and Their Effects
| Interferent Category | Example Interferents | Biosystems Affected |
|---|---|---|
| Biomolecules | Proteins, Lipids, Carbohydrates | Optical, Electrochemical, Mass-based |
| Small Molecules | Medications, Metabolites, Antioxidants | Electrochemical, Enzyme-based |
| Ionic Components | High salt concentrations, Metal ions | Electrochemical, Nucleic acid-based |
| Particulate Matter | Cells, Debris, Bubbles | Optical, Mass-based |
Biosensor performance is also compromised by improper storage conditions, temperature fluctuations during analysis or transport, and humidity variations that affect reagent stability [1] [12]. In resource-limited settings, additional challenges include inadequate cold chain maintenance, power supply instability affecting electronic components, and limited quality control infrastructure [12].
Troubleshooting Guide: Frequently Asked Questions
FAQ 1: How can I distinguish true TLR4 activation from false positives in cell-based biosensor assays?
Challenge: Lipopolysaccharide (LPS) from different bacterial sources can produce varying signaling patterns that may be misinterpreted. For instance, LPS from E. coli and S. minnesota induce distinct dynamic mass redistribution (DMR) profiles in TLR4 biosensors [9].
Solution: Implement a multi-pronged verification approach:
- Include control experiments with TLR4-specific antagonists like TAK-242 to confirm receptor-specific signaling
- Use multiple LPS chemotypes to compare response patterns
- Employ cytoskeletal inhibitors (cytochalasin B, latrunculin A, nocodazole) to verify that signals depend on cellular structural reorganization
- Validate findings in control cell lines lacking TLR4 expression to identify non-specific responses
Experimental Protocol: TLR4 Signaling Specificity Verification
- Culture HEK293 TLR4/MD-2/CD14 reporter cells in antibiotic-free media
- Passage cells every 48-72 hours, maintaining ≤80% confluence to prevent background FRET
- Plate cells in 96-well plates at 20,000 cells/well 24 hours before treatment
- Prepare LPS dilutions in Opti-MEM and equilibrate to room temperature
- Mix samples with Lipofectamine 2000 (1.5μl reagent + 28.5μl Opti-MEM, 5min incubation)
- Combine LPS and transfection mixtures, incubate 30min at room temperature
- Divide mixtures among 3 replicate wells
- After 48 hours, trypsinize and fix cells in 2% PFA for flow cytometry analysis
- Include TAK-242 controls and TLR4-negative cell lines in each experiment [9]
FAQ 2: What strategies can reduce false positives in nucleic acid detection using SPR biosensors?
Challenge: Non-specific DNA adsorption and reflective angle misinterpretation can generate false positives in SPR-based DNA detection [10].
Solution: Apply machine learning classification to differentiate specific binding from non-specific adsorption:
- Collect comprehensive reflective angle data across multiple gold surface thicknesses
- Utilize feature selection algorithms (t-SNE) to identify patterns associated with true binding events
- Implement random forest classifiers that achieve 94% accuracy in DNA classification tasks
- Normalize data using min-max normalization before analysis to improve classifier performance
Experimental Protocol: ML-Enhanced DNA Detection Validation
- Prepare gold surfaces with varying thicknesses for SPR analysis
- Measure reflective angles of 632.8nm light at 0.05° intervals from 40°-89°
- Collect data at three binding stages: bare surface, immobilized ssDNA, and hybridized dsDNA
- Apply min-max normalization to reflective angle data
- Implement t-SNE feature extraction to reduce dimensionality and identify clustering patterns
- Train random forest classifiers on labeled datasets of known true and false positive outcomes
- Validate model performance using 10-fold cross-validation
- Deploy optimized classifier to distinguish specific DNA binding from non-specific adsorption [10]
FAQ 3: How can I minimize cross-reactivity in antibody-based biosensors for mycotoxin detection?
Challenge: Antibodies against mycotoxins like aflatoxins, ochratoxin A, and zearalenone may cross-react with structurally similar compounds in food samples [8].
Solution: Implement dual modality biosensing with cross-validation:
- Combine electrochemical and optical detection methods to verify results through two independent mechanisms
- Incorporate aptamer-based recognition elements as they offer higher batch-to-batch consistency
- Use sample pre-treatment to remove interfering compounds
- Employ signal amplification strategies with nanomaterials that improve specificity
Experimental Protocol: Dual Modality Mycotoxin Detection
- Functionalize electrode surface with anti-mycotoxin antibodies or aptamers
- For optical channel, integrate SERS-active nanoparticles functionalized with same recognition element
- Apply sample to biosensor and record both electrochemical impedance and SERS signals
- Process signals independently through separate transduction pathways
- Compare results from both modalities - concordant signals indicate true positives
- Discordant signals suggest interference or cross-reactivity requiring further investigation
- Validate against chromatographic standards for confirmation [2] [8]
FAQ 4: What approaches can identify instrument-generated false positives versus true biological signals?
Challenge: Signal drift, electronic noise, and transducer artifacts can mimic true biological responses [11].
Solution: Implement theory-guided deep learning to distinguish instrument artifacts from biological signals:
- Record dynamic biosensor responses rather than single endpoint measurements
- Apply data augmentation to address sparsity in calibration datasets
- Use cost function supervision incorporating biosensor theory to guide machine learning models
- Validate with known standards across the concentration range to establish signal patterns
Experimental Protocol: Artifact Identification Using Dynamic Signals
- Collect time-series data from biosensor during analyte detection
- Augment dataset through synthetic data generation to address class imbalance
- Train recurrent neural networks (RNN) with theory-guided constraints
- Incorporate domain knowledge of binding kinetics into model cost function
- Use theory-guided RNN classifiers to identify signal patterns characteristic of instrument artifacts
- Achieve up to 98.5% accuracy in distinguishing true signals from false positives
- Implement continuous monitoring with dynamic signal analysis to reduce time delay [11]
Research Reagent Solutions for False Positive Mitigation
Table: Essential Reagents for False Positive Control
| Reagent Category | Specific Examples | Function in False Positive Control |
|---|---|---|
| Specific Inhibitors | TAK-242 (TLR4), Cytochalasin B (actin) | Confirm pathway-specific signaling and cytoskeletal dependence |
| Cytoskeletal Inhibitors | Latrunculin A, Nocodazole | Verify morphological changes in whole-cell biosensors |
| Binding Blockers | BSA, Casein, Synthetic blocking peptides | Reduce non-specific adsorption to surfaces |
| Reference Materials | LPS from different bacterial species | Distinguish specific response patterns from non-specific effects |
| Surface Chemistry | PEG-based coatings, Zwitterionic polymers | Minimize non-specific binding in optical and electrochemical sensors |
| ML Training Standards | Labeled datasets of true/false positives | Train classifiers for automatic artifact recognition |
Visualization of False Positive Mitigation Workflows
Comprehensive False Positive Diagnosis Pathway
Dual Modality Biosensor Verification System
Systematic classification of false positive triggers enables researchers to develop targeted mitigation strategies that enhance biosensor reliability. The integration of dual modality sensing, theory-guided machine learning, and comprehensive troubleshooting protocols provides a multifaceted approach to false positive reduction. As biosensor technologies evolve toward greater sensitivity and automation, robust false positive identification and management will remain essential for research validity, clinical diagnostics, and environmental monitoring applications.
Analyzing the Impact of Bioreceptor-Antigen Interactions on Specificity
Core Concepts: Bioreceptors and Specificity
What are bioreceptors and why are they critical for biosensor specificity?
Bioreceptors are biological or biomimetic molecules immobilized on a biosensor that specifically recognize and bind to a target analyte (antigen). This specific interaction is the foundation of biosensor specificity, as the bioreceptor determines which molecules will be detected. Common bioreceptors include antibodies, enzymes, nucleic acids, aptamers, and whole cells [1] [13].
The specificity of a biosensor refers to its ability to accurately detect and measure a target analyte while ignoring interfering substances in a sample. This characteristic is primarily determined by the selective binding affinity between the bioreceptor and its target antigen [14].
What are the most common types of bioreceptors used in diagnostic assays?
Table 1: Common Bioreceptor Types and Their Characteristics
| Bioreceptor Type | Description | Key Advantages | Common Sources of False Positives |
|---|---|---|---|
| Antibodies [14] | Y-shaped proteins produced by the immune system that bind to specific antigens. | High specificity and affinity; well-established immobilization methods. | Cross-reactivity with similar epitopes; non-specific adsorption. |
| Engineered Antibody Fragments [14] (e.g., scFv, Fab, nanobodies) | Genetically modified fragments of full antibodies. | Smaller size can improve binding site access and signal; often more stable. | Similar to full antibodies, though reduced Fc region can minimize some non-specific binding. |
| Enzymes [1] | Proteins that catalyze specific biochemical reactions. | Signal amplification via catalytic activity. | Cross-talk with similar substrates or inhibitors in sample. |
| Nucleic Acids [1] [13] (DNA, RNA, aptamers) | Strands with specific sequences that bind complementary strands (hybridization) or specific targets (aptamers). | High stability; synthetic production; aptamers can be selected for a wide range of targets. | Non-specific hybridization; secondary structure formation in aptamers. |
| Whole Cells [1] | Microorganisms or eukaryotic cells used as sensing elements. | Can report on functional responses (e.g., toxicity). | Often lack the selectivity of enzyme- or antibody-based sensors. |
Troubleshooting False Positives: FAQs and Guides
Our assay consistently produces false positives. How can we determine if the cause is bioreceptor-related?
A systematic investigation is required to isolate the variable of the bioreceptor-antigen interaction. The following workflow diagram outlines a recommended diagnostic process.
Experimental Protocol: Diagnosing Bioreceptor-Related False Positives
- Blank Solution Test: Run the biosensor assay using the complete protocol with a sample matrix that is identical to your test samples but is guaranteed to contain zero target analyte. A positive signal indicates significant non-specific binding or interference from the sample matrix [15].
- Cross-Reactivity Test: Repeat the assay with a sample containing a known, structurally similar compound (an interferent) that is not the target analyte. A positive signal confirms the bioreceptor lacks sufficient specificity and is cross-reacting [14].
- Bioreceptor Batch Test: Repeat the original assay with a fresh, properly validated batch of the bioreceptor. If the false positive signal disappears, the original bioreceptor batch may have been degraded, denatured, or contaminated [1].
We use antibody bioreceptors. What are the primary causes of false positives in immunosensors?
False positives in immunosensors (antibody-based biosensors) often stem from the following issues:
- Cross-Reactivity: The antibody binds to epitopes on non-target molecules that are structurally similar to the intended antigen [14]. This is a primary failure mode of specificity.
- Non-Specific Adsorption (NSA): Proteins or other components in the sample matrix adhere to the sensor surface or parts of the antibody (like the Fc region) through non-specific interactions (e.g., hydrophobic, ionic), generating a signal indistinguishable from the specific binding event [14] [15].
- Incomplete Washing: Failure to adequately remove unbound or loosely bound molecules after the binding step can leave behind non-specifically trapped analytes or interferents [1].
- Antibody Degradation: Improper storage or handling can lead to antibody aggregation, denaturation, or fragmentation, which can expose hydrophobic regions and increase non-specific binding [1].
How can antibody engineering help minimize false positives?
Antibody engineering creates optimized fragments that can enhance specificity and reduce non-specific binding. The following table details common engineered formats.
Table 2: Engineered Antibody Fragments for Enhanced Biosensing
| Engineered Format | Description | Mechanism for Reducing False Positives | Common Application in Biosensors |
|---|---|---|---|
| Single-Chain Variable Fragment (scFv) | The variable regions of the heavy and light chains linked by a peptide linker. | Smaller size allows for denser immobilization and better orientation, reducing nonspecific binding from the Fc region. | Electrochemical and optical immunosensors for small molecules [14]. |
| Antigen-Binding Fragment (Fab) | A fragment containing one constant and one variable domain of both the heavy and light chains. | Lacks the Fc region, eliminating a major source of non-specific adsorption. | Diagnostic assays requiring high stability [14]. |
| Nanobodies (VHH) | Single-domain antibodies derived from heavy-chain-only antibodies in camellids. | Extremely small size and simple structure improve stability and access to concave epitopes, enhancing specificity. | Detection of complex targets like viruses and cancer biomarkers [14]. |
| Bispecific Antibodies | Antibodies engineered to have two different antigen-binding sites. | Can be designed for "AND-gate" logic, requiring two antigens for a signal, drastically increasing specificity. | Highly specific cell detection and targeted therapies [14]. |
Beyond the bioreceptor itself, what other factors can lead to false signals?
The bioreceptor is only one component of the system. The following factors are also critical:
- Transducer Limitations: The physical transducer (e.g., FET, electrode) may be sensitive to environmental changes like pH, temperature, or ionic strength, producing a signal shift that can be misinterpreted [1] [15]. Sensor design and surface topology can also limit the probability of target molecules adsorbing to the active detection area [15].
- Assay Conditions: Suboptimal pH, ionic strength, or temperature can disrupt the precise binding kinetics of the bioreceptor-antigen interaction, promoting non-specific binding [1] [16].
- Sample Matrix Effects: Complex samples (e.g., blood, serum, food homogenates) contain numerous proteins, lipids, and other molecules that can foul the sensor surface or interfere with the binding reaction [13].
Advanced Experimental Protocols
Protocol: Surface Passivation to Minimize Non-Specific Adsorption
Objective: To block reactive sites on the sensor surface surrounding the immobilized bioreceptor to prevent non-specific binding of sample components.
Reagent Solutions:
- Blocking Agent: Bovine Serum Albumin (BSA) at 1-5% w/v, casein, or commercial blocking buffers.
- Wash Buffer: Phosphate Buffered Saline (PBS) with a mild detergent (e.g., 0.05% Tween-20).
Methodology:
- After immobilizing the bioreceptor on the sensor surface, rinse the surface three times with wash buffer.
- Incubate the sensor with the blocking solution for 30-60 minutes at room temperature.
- Thoroughly wash the sensor surface with wash buffer to remove any unbound blocking agent.
- The sensor is now ready for use. Validate the passivation by testing with a blank sample.
Protocol: Using Isotype Controls for Immunosensors
Objective: To distinguish specific signal from non-specific background signal in antibody-based assays.
Reagent Solutions:
- Isotype Control: An antibody of the same isotype (e.g., IgG1, IgG2a) and from the same host species as your primary bioreceptor antibody, but with no specificity for your target antigen.
Methodology:
- Run your assay in parallel on two identical sensor platforms.
- On the test sensor, immobilize the specific primary antibody.
- On the control sensor, immobilize the isotype control antibody at the same concentration.
- Expose both sensors to the same sample and run the identical protocol.
- The signal generated by the isotype control sensor represents the non-specific background. Subtract this value from the signal of the test sensor to obtain the specific signal.
Protocol: Assessing Binding Kinetics and Specificity using a SOI-FET Biosensor
Objective: To theoretically model and understand the probabilistic nature of detection and how it impacts accuracy, particularly at low analyte concentrations.
Background: The adsorption of "antibody + antigen" (AB+AG) complexes on a sensor surface like a Silicon-on-Insulator Field-Effect Transistor (SOI-FET) is a random event influenced by diffusion, concentration, and temperature. The probability of a target molecule hitting the sensor surface is described by the Poisson distribution [15]. At very low concentrations (e.g., femtomolar), this probability becomes very low, leading to false negatives. Conversely, non-specific binding of background particles can lead to false positives [15].
Methodology & Visualization: The logical flow of the detection process and its failure points can be modeled as follows:
Key Consideration: This model highlights that achieving a reliable signal requires not only specific bioreceptors but also a system design that maximizes the probability of correct complex adsorption. Using a larger number of biosensors on a single chip can improve accuracy and reduce detection time by increasing the total capture area and statistical probability of detection [15].
Assessing Sample Matrix Effects and Interfering Substances in Complex Fluids
Matrix effects present a significant challenge in the translation of biosensors from controlled laboratory settings to clinical use. These effects refer to the interference caused by the complex components of biological samples, which can alter the sensor's response and lead to inaccurate results, including false positives and negatives [17]. The core of the problem lies in the fact that while a biosensor may demonstrate exceptional sensitivity and a low limit of detection (LOD) under pristine buffer conditions, this performance often degrades when the sensor is applied to real-world samples such as serum, urine, sputum, or saliva [17] [18]. Molecules present in these matrices can interact with the analyte, the sensor surface, or the biorecognition elements, causing nonspecific adsorption, signal suppression, signal enhancement, or cross-reactivity [17] [19]. Overcoming these effects is therefore not merely an optimization step but a fundamental requirement for developing reliable diagnostic biosensors.
FAQs on Matrix Effects and Interference
Q1: What are the most common sources of interference in complex biological fluids? Interference in complex fluids can arise from a wide variety of sources, which can be broadly categorized as follows [19]:
- Analyte-Independent Interference: This includes factors related to sample handling and general composition, such as hemolysis (rupture of red blood cells), lipemia (high lipid content), the choice of anticoagulants in blood samples, and the overall viscosity of the sample.
- Analyte-Dependent Interference: This involves specific compounds within the sample that actively interfere with the assay's biochemistry. Key examples include:
- Human Anti-Animal Antibodies (HAAA): Such as Human Anti-Mouse Antibodies (HAMA), which can bind to assay antibodies and create a signal.
- Autoantibodies: Like the rheumatoid factor, which targets the Fc portion of immunoglobulin G (IgG).
- Cross-reactivity: Occurs when the biorecognition element (e.g., an antibody) binds to molecules structurally similar to the target analyte.
- Exogenous Interference: This category covers external factors, including:
- Drugs and Metabolites: Common examples are biotin supplements (which interfere with streptavidin-biotin systems) and certain corticosteroids.
- Sample Carryover: Contamination from previous runs in automated systems.
- Assay Conditions: Suboptimal pH or ionic strength of the assay buffer.
Q2: How does the sample matrix lead to false positives and false negatives? The matrix causes inaccurate results through several distinct mechanisms [1] [19]:
False Positives are typically caused by:
- Nonspecific Binding: Matrix proteins or other molecules adsorbing to the sensor surface, creating a background signal.
- Cross-reactivity: The capture agent binding to non-target molecules with similar epitopes.
- Interfering Antibodies: HAAAs can bridge capture and detection antibodies in a sandwich assay, mimicking the presence of the target analyte.
False Negatives are often the result of:
- Signal Suppression: Matrix components can sterically hinder access to the sensor surface or quench the output signal (e.g., in optical assays).
- The "Hook Effect": In sandwich assays, extremely high analyte concentrations can saturate both the capture and detection antibodies, preventing the formation of the "sandwich" complex and leading to a falsely low signal.
- Analyte Degradation: Enzymes in the sample may break down the target analyte before it can be detected.
Q3: Why do some biosensors work perfectly in buffer but fail with patient samples? This failure is primarily due to the "matrix effect," a term that encapsulates all the ways a complex sample differs from a simple buffer [17] [18]. Biological fluids contain a high and variable concentration of proteins, lipids, salts, and cells. These components can foul the sensor surface, change the local pH or ionic environment at the sensor interface (critically affecting charge-based sensors like nanowires or electrochemical sensors), or contribute to a high background signal in optical assays due to autofluorescence or turbidity [17] [20]. In essence, the controlled, "clean" environment of the buffer is replaced by a "dirty" and unpredictable one in a clinical sample.
Q4: What are the best strategies to identify and mitigate matrix effects? A systematic approach is required to identify and overcome matrix interference [19]:
Identification:
- Spike-and-Recovery Experiments: This is a cornerstone validation test. A known amount of analyte is spiked into the sample matrix, and the measured concentration is compared to the expected value. Recovery outside the 80-120% range indicates interference.
- Parallel Analysis: Comparing results with a reference method (e.g., LC-MS or a different immunoassay format) helps verify accuracy.
- Linearity-of-Dilution: Diluting the sample and assessing if the measured analyte concentration decreases linearly can reveal matrix effects.
Mitigation:
- Sample Pre-treatment: Dilution, filtration, or extraction can reduce the concentration of interferents.
- Surface Blocking: Using blockers like BSA, casein, or normal serum to saturate non-specific binding sites on the sensor surface.
- Improved Assay Design: Using matched antibody pairs to reduce cross-reactivity, or switching assay formats (e.g., to mitigate the hook effect).
- Choice of Biosensor Technology: Label-free optical sensors like Surface Plasmon Resonance (SPR) are sensitive to matrix effects, while magnetic nanosensors have been shown to be largely matrix-insensitive, as they are unaffected by sample turbidity, pH, or ionic strength within a broad range [20].
Troubleshooting Guide: Common Problems and Solutions
The table below outlines common symptoms, their potential causes, and actionable solutions.
| Symptom | Potential Cause | Troubleshooting Solution |
|---|---|---|
| High background signal/noise | Nonspecific adsorption of matrix proteins to sensor surface. | Improve surface blocking with BSA, casein, or commercial blockers; include a reference sensor; use more stringent wash buffers [21] [19]. |
| Signal drift during measurement | Sensor surface not equilibrated; bulk refractive index shifts (SPR). | Equilibrate the sensor surface with running buffer overnight or with multiple injections; match the composition of the sample and running buffers [21]. |
| Low signal recovery in spiked samples | Matrix components suppressing signal or degrading analyte. | Dilute the sample to reduce interferent concentration; add enzyme inhibitors; use a sample purification step [19]. |
| Inconsistent results between replicates | Sample carryover or dispersion; heterogeneous or viscous sample. | Increase wash steps between runs; ensure proper sample mixing and homogenization; implement a sample liquefaction step for sputum/mucus [21] [22]. |
| Falsely low signal at high analyte concentration (Hook Effect) | Saturation of both capture and detection antibodies in a sandwich assay. | Test sample at multiple dilutions; switch to a competitive assay format or an assay design with a larger dynamic range [19]. |
| Poor sensitivity compared to buffer tests | Fouling of sensor surface, limiting analyte access. | Implement robust antifouling surface chemistries (e.g., PEGylation); use nanostructured surfaces to minimize fouling [17]. |
Experimental Protocols for Assessing Interference
Protocol: Spike-and-Recovery Experiment
This protocol is a fundamental test to quantify matrix interference [19].
Objective: To determine whether components in a sample matrix are suppressing or enhancing the detected signal of the target analyte.
Materials:
- Neat (unspiked) sample matrix (e.g., pooled human serum)
- Assay buffer
- Pure analyte standard
- Standard equipment for your biosensor (plate reader, etc.)
Method:
- Prepare three sets of samples in duplicate or triplicate:
- Neat Matrix: The sample matrix with no added analyte.
- Spiked Buffer (Control): A known concentration of analyte spiked into the standard assay buffer.
- Spiked Matrix (Test): The same known concentration of analyte spiked into the sample matrix.
- It is recommended to test at least three different analyte concentrations (low, medium, and high).
- Run all samples according to your established biosensor assay protocol.
- Calculation: Determine the percentage recovery using the formula:
- % Recovery = ( [Spiked Matrix] - [Neat Matrix] ) / [Spiked Buffer] × 100
Interpretation of Results:
| % Recovery | Interpretation |
|---|---|
| 80% - 120% | Acceptable, minimal interference. |
| < 80% | Signal suppression (indicative of matrix interference). |
| > 120% | Signal enhancement (possible interference or cross-reactivity). |
Case Study: Overcoming Sputum Matrix Effects with a Paper Biosensor
Background: Detecting pyocyanin (PYO) in sputum for diagnosing Pseudomonas aeruginosa infections is challenging due to the highly viscous and complex sputum matrix, which causes significant variability in traditional competitive ELISAs [22].
Innovative Solution: A paper-based biosensor was developed to mitigate these effects.
Workflow Diagram:
Key Advantages and Outcomes:
- Rapid Results: The entire assay is completed within 6 minutes, compared to 2 hours for ELISA.
- Reduced Matrix Effects: The paper platform and mild enzymatic liquefaction (using hydrogen peroxide) minimized the variability caused by the sputum matrix, leading to a lower relative standard deviation than ELISA.
- Point-of-Care Applicability: The simplicity and speed make it a strong candidate for bedside testing [22].
Key Research Reagent Solutions
The following table details essential reagents used to combat interference in biosensor assays, as discussed in the cited research.
| Research Reagent | Function in Troubleshooting | Brief Explanation |
|---|---|---|
| Bovine Serum Albumin (BSA) | Blocking Agent | Used to saturate non-specific binding sites on the sensor surface, reducing background noise from protein adsorption [19] [22]. |
| Casein Buffer | Blocking Agent | An effective alternative to BSA for blocking, often used in immunoassays to prevent non-specific binding [19]. |
| Heterophilic Blocking Reagents | Interference Blocker | Specifically designed to bind and neutralize Human Anti-Mouse Antibodies (HAMA) and other heterophilic antibodies, preventing false positives [19]. |
| Polystyrene sulfonate (PSS) | Sensor Platform Material | Used to functionalize paper in biosensors, creating a reservoir for reagents like antibody-conjugated nanoparticles [22]. |
| Streptavidin-Coated Magnetic Nanoparticles | Signal Generation & Separation | Used in matrix-insensitive assays (e.g., GMR sensors). The magnetic tag is detected without interference from optical properties of the sample, and magnetic fields facilitate washing and separation [20]. |
| PC1-BSA Bioconjugate | Competing Antigen | A synthesized molecule used in competitive assays (e.g., for pyocyanin detection) where it competes with the analyte for binding sites on the detection antibody [22]. |
Comparison of Biosensor Technologies and Matrix Effects
Different biosensor transduction principles exhibit varying degrees of susceptibility to matrix effects. The table below summarizes the advantages and disadvantages of several common technologies in this context.
| Biosensor Technology | Key Advantage | Susceptibility to Matrix Effects | Mitigation Strategy |
|---|---|---|---|
| Surface Plasmon Resonance (SPR) [17] [18] | Real-time, label-free kinetic data. | High. Sensitive to bulk refractive index changes from sample matrix; surface fouling. | Reference channel subtraction; extensive buffer matching; advanced antifouling coatings. |
| Electrochemical (Amperometric) [17] [18] | Simple design, highly miniaturizable. | High. Sensitive to pH and ionic strength; surface fouling limits access. | Use of mediators; protective membranes; sample dilution. |
| Magnetic Nanosensor (GMR) [20] | Highly matrix-insensitive. | Very Low. Unaffected by sample turbidity, autofluorescence, pH (4-10), or ionic strength. | Requires minimal sample pre-treatment; no complex mitigation needed. |
| Lateral Flow Assays (LFA) [17] | Low cost, rapid, simple use. | Medium. Viscosity affects flow; non-specific binding can occur. | Optimized sample pad chemistry; inclusion of detergent in buffers. |
| Biolayer Interferometry (BLI) [23] | Label-free, "dip-and-read", real-time kinetics. | Medium. Can be sensitive to nonspecific binding and refractive index shifts. | Includes onboard shake to reduce nonspecific binding; reference sensor subtraction. |
The Role of Transducer Stability and Non-Specific Binding in Signal Noise
Troubleshooting Guide: Frequently Asked Questions
Q1: What are the primary sources of signal noise and false positives in biosensor assays?
The main sources are non-specific binding (NSB) of molecules to the sensor surface and transducer instability caused by environmental factors. NSB occurs when biomolecules interact with the sensor through means other than the intended specific biorecognition, creating a false signal that is indistinguishable from a true positive [1] [24]. Transducer instability can arise from temperature fluctuations, electromagnetic interference, or poor power supply regulation, which introduce noise and drift into the measurement signal [25] [26] [27].
Q2: How can I experimentally confirm that my signal is caused by non-specific binding and not a true positive?
You can employ a dielectrophoretic (DEP) repulsion method. This technique uses a calibrated electric field to apply a controlled physical force to bound particles or molecules. Specifically bound analytes, which have stronger binding affinity, will remain attached, while non-specifically bound entities, with weaker interactions, will be detached [24]. A significant drop in signal post-DEP application confirms the presence of NSB. Alternatively, using surface plasmon resonance (SPR) or similar techniques to monitor binding kinetics in real-time can help, as NSB often shows fast, nonsensical on/off rates compared to the characteristic kinetics of specific binding.
Q3: What practical steps can I take to reduce non-specific binding in my assay?
The following table summarizes key reagents and their functions for minimizing NSB [28]:
Table: Research Reagent Solutions for Minimizing Non-Specific Binding
| Reagent | Function/Brief Explanation |
|---|---|
| Betaine | Organic additive that disrupts secondary structure formation in primers and templates, improving assay specificity. |
| Dimethyl Sulfoxide (DMSO) | Helps in strand separation of DNA and inhibits nonspecific primer interactions. |
| Uracil-DNA-Glycosylase (UDG) | Enzyme that degrades uracil-containing DNA from previous amplification reactions, effectively controlling carry-over contamination. |
| Gold Nanoparticles (AuNPs) | Can be used to create a hot-start effect, suppressing enzyme activity until the optimal temperature is reached, thus reducing nonspecific amplification. |
| PEG (Polyethylene Glycol) | Used in surface backfilling to create a dense, inert layer that sterically hinders non-specific adsorption of proteins and other biomolecules. |
| Bovine Serum Albumin (BSA) | A common blocking agent that occupies potential non-specific binding sites on the transducer surface. |
Q4: My biosensor signal is unstable and drifts over time. How can I troubleshoot the transducer's stability?
Follow this systematic approach:
- Verify the Power Supply: Use a multimeter to ensure the power source provides a stable, clean voltage that matches the transducer's specifications. Noise or voltage fluctuations from the supply can directly manifest as signal noise [25].
- Inspect for Environmental Interference: Ensure the transducer is properly shielded and grounded. Keep it away from sources of electromagnetic interference (EMI) such as motors, power cables, and radio transmitters [25] [26].
- Analyze Environmental Conditions: Check that the operating temperature and humidity are within the sensor's specified limits. Temperature extremes and rapid cycling can cause significant accuracy drift and mechanical stress [26].
- Check Physical Connections: Inspect all wiring and terminals for loose connections, damage, or corrosion, which can cause intermittent signals and noise [25].
Q5: How can I optimize the Signal-to-Noise Ratio (SNR) in my optical biosensor readings?
Optimizing SNR involves maximizing your desired signal while minimizing noise sources.
- For the Signal: Ensure your biorecognition elements (e.g., antibodies, aptamers) are fresh and properly immobilized. For optical sensors, you can increase the excitation light intensity, but this must be balanced against power consumption and potential photobleaching [27].
- For the Noise: Implement the stability measures listed above. Furthermore, when analyzing data such as photoplethysmography (PPG) signals, you can apply band-pass filtering in the frequency domain to isolate the biologically relevant signal (e.g., below 20 Hz) from higher-frequency electronic and environmental noise [27]. The optimal configuration is a balance between high SNR and acceptable system power consumption.
Experimental Protocols
Protocol 1: Discriminating Specific from Non-Specific Binding Using Dielectrophoretic (DEP) Forces
This protocol is adapted from Liu et al. and is designed for on-chip magnetic bio-assays [24].
1. Objective: To apply a controlled rupture force via DEP to remove non-specifically bound magnetic particles while leaving specifically bound particles intact.
2. Materials:
- Functionalized biosensor chip with integrated electrodes and magnetoresistive (e.g., GMR) sensors.
- Streptavidin-coated magnetic particles (MPs).
- Target analyte (e.g., biotinylated molecules for specific binding).
- Non-functionalized or PEG-coated surface for NSB control.
- Function generator for creating AC electric fields.
- Buffer solution.
3. Methodology:
- Step 1: Surface Preparation. Functionalize different regions of the sensor chip with specific capture molecules (e.g., biotin) and non-specific blocking agents (e.g., PEG).
- Step 2: Incubation. Incubate the chip with a solution containing the target analyte and the magnetic particles. Allow binding to occur.
- Step 3: Baseline Measurement. Use the magnetoresistive sensors to measure the initial magnetic signal, which represents total binding (specific + non-specific).
- Step 4: DEP Force Application. Apply a non-uniform AC electric field across the integrated electrodes to generate a repulsive DEP force. The frequency and voltage must be optimized to exert a force strong enough to break weaker non-specific bonds but not stronger specific ones.
- Step 5: Post-DEP Measurement. Re-measure the magnetic signal. A significant decrease indicates the removal of non-specifically bound MPs.
4. Data Analysis: Compare the magnetic signals before and after DEP application. The remaining signal is attributed to specific binding. The percentage signal loss quantifies the level of non-specific binding in the assay.
Protocol 2: Reducing False-Positives in Amplification-Based Biosensors Using UDG Enzyme
This protocol is for loop-mediated isothermal amplification (LAMP) assays but can be adapted for other nucleic acid amplification techniques [28].
1. Objective: To eliminate false-positive results caused by carry-over contamination of amplicons from previous reactions.
2. Materials:
- LAMP reaction mix (Bst DNA polymerase, primers, dNTPs, etc.).
- Uracil-DNA-Glycosylase (UDG).
- dUTP (incorporated in place of dTTP during amplification).
- Template DNA.
3. Methodology:
- Step 1: Reaction Setup. Prepare the LAMP master mix, substituting dTTP with dUTP. Add UDG enzyme to the mix before the template is added.
- Step 2: Contamination Degradation. Incubate the reaction mix (without Bst polymerase, or at a low temperature where Bst is inactive) for a short period (e.g., 10-30 minutes at 25-37°C). During this step, UDG will actively degrade any uracil-containing contaminating DNA from previous runs, breaking the DNA backbone and rendering it unamplifiable.
- Step 3: Enzyme Inactivation & Amplification. Heat the reaction to the LAMP operating temperature (60-65°C). This heat step simultaneously inactivates UDG (which is thermolabile) and activates the hot-start Bst DNA polymerase, allowing only the intended, pristine template to be amplified.
4. Data Analysis: Compare results from UDG-treated and untreated reactions. A reduction in false-positive amplification in negative controls for the UDG-treated reactions confirms the effectiveness of the method.
Data Presentation
Table 1: Comparison of Physical Forces for Discriminating Non-Specific Binding
| Force Method | Mechanism | Advantages | Limitations |
|---|---|---|---|
| Dielectrophoretic (DEP) Repulsion [24] | Applies electric field gradient to exert force on bound particles. | Easy electrode fabrication; availability of repulsive forces; low thermal dissipation. | Requires specialized chips with integrated electrodes; optimization of voltage/frequency is needed. |
| Fluidic Shear Forces | Uses buffer flow to create a washing force. | Conceptually simple; can be integrated into microfluidics. | Can be less controllable; may not generate sufficient localized force for strong discrimination. |
| Magnetic Forces | Uses magnetic field gradient to pull magnetic particles. | Highly specific to magnetic labels. | Force generation can be poor due to size mismatch; requires magnetic particles and equipment. |
Table 2: Methods for Confirming True vs. False-Positive Signals Post-Amplification
| Confirmation Method | Analyte | Principle | Reference |
|---|---|---|---|
| CRISPR/Cas System | Nucleic Acids | Uses guide RNA to specifically recognize and cleave target LAMP amplicons, generating a signal only for specific products. | [28] |
| DNAzyme Formation | Nucleic Acids | LAMP amplicons with a G-quadruplex sequence react with hemin to form a DNAzyme that causes a colorimetric change, distinguishing it from nonspecific products. | [28] |
| Lateral Flow Immunoassay (LFA) | Nucleic Acids/Proteins | Uses hybridized probes to accurately recognize and bind to specific LAMP amplicons, providing a visual readout on a test strip. | [28] |
Diagram Specifications
Diagram Title: Biosensor Workflow and Noise Source Map
Diagram 2: DEP Force Discrimination Workflow
Diagram Title: DEP Force NSB Discrimination Protocol
Diagram 3: Signal-to-Noise Optimization Logic
Diagram Title: SNR Troubleshooting Decision Tree
Leveraging Advanced Technologies and Assay Designs for Enhanced Specificity
Integrating Machine Learning for Signal Pattern Recognition and Noise Reduction
Frequently Asked Questions (FAQs)
General ML Integration
Q1: What are the most suitable machine learning algorithms for reducing noise in biosensor signals? The choice of algorithm depends on your data type and the nature of the noise. For supervised tasks with labeled data, Convolutional Neural Networks (CNNs) are highly effective for processing signal and image data from platforms like lateral flow assays, as they can learn to ignore noise and extract robust features. [29] Support Vector Machines (SVMs) and Random Forests are also widely used for classification tasks, such as distinguishing true positive signals from false positives. [30] [29] For unlabeled data or discovering hidden patterns in signal datasets, unsupervised learning methods like clustering can be valuable. [31] [30]
Q2: How can I quickly check if my ML model is suffering from overfitting during biosensor signal analysis? A primary indicator of overfitting is a significant performance gap between your training and validation datasets. If your model achieves high accuracy on the training data but performs poorly on the separate validation data, it has likely memorized the training data instead of learning generalizable patterns. [29] To mitigate this, ensure you use a rigorous data splitting protocol, typically 60% for training, 20% for validation, and 20% for blind testing. [29]
Q3: What is the role of data preprocessing in improving ML-based biosensor signal analysis? Data preprocessing is a critical step that dramatically improves ML model performance. It involves:
- Data denoising and background subtraction to enhance the signal-to-noise ratio. [29]
- Data normalization to reduce variability from different sensors or experimental conditions. [29]
- Data augmentation to artificially expand your dataset, which can improve model robustness. [29] These steps help minimize the impact of outlier samples and the inherent variabilities present in raw biosensor signals. [29]
Troubleshooting False Positives
Q4: My ML-powered optical biosensor is producing false positives. What are the common causes? False positives can arise from multiple sources, which should be investigated systematically. The following table outlines common causes and their respective troubleshooting actions.
| Cause | Troubleshooting Action |
|---|---|
| Nonspecific Binding | Review bioreceptor specificity (e.g., antibody/aptamer cross-reactivity); optimize blocking conditions and wash steps. [1] |
| Contaminated Reagents | Implement fresh reagent controls; ensure proper storage of critical components like enzymes and antibodies. [1] |
| Insufficient Model Training | Increase training dataset size, ensuring it includes adequate negative samples and examples of common interferents. [1] [30] |
| Signal Noise Misinterpretation | Apply advanced signal processing filters (e.g., digital smoothing); re-train the model with noisier data to improve robustness. [30] [29] |
| Inconsistent Sample Matrix | Standardize sample preparation protocols; include matrix-matched calibration standards in your experiments. [1] |
Q5: What experimental controls are essential for validating an ML-integrated biosensor and minimizing false results? Robust validation requires several key controls [32]:
- Donor-only and Acceptor-only controls: Essential for calculating and correcting for bleed-through in optical signals (e.g., FRET biosensors).
- Biosensor mutant controls: Use biosensors with inactivating mutations to establish a baseline for non-specific signals.
- Non-specific regulator controls: Co-express proteins that do not regulate your target activity to confirm the specificity of the biosensor's response.
- Positive and negative regulator controls: For dynamic biosensors, co-express known activators and inhibitors to confirm the sensor's expected response range.
Troubleshooting Guides
Problem 1: High Signal Noise in Electrochemical Biosensor Data
Symptoms: Unstable baseline, erratic signal output, poor signal-to-noise ratio that obscures the target analyte signal.
Investigation and Resolution Protocol:
Verify Experimental Conditions:
- Check the stability and purity of your buffer solutions. Prepare fresh solutions if necessary.
- Confirm that all electrical connections are secure and that the instrument is properly grounded.
Apply Signal Processing Techniques:
- Implement Digital Filtering: Apply a moving average filter or a low-pass filter to the raw signal data to smooth out high-frequency noise. [29]
- Utilize Machine Learning: Train a model, such as a denoising autoencoder, on a dataset of clean and noisy signals. The model can learn to map noisy input to a clean output, effectively filtering the signal. [30]
Optimize Biosensor Design (if possible):
Problem 2: False Positives in a Colorimetric Lateral Flow Assay Analyzed by a CNN
Symptoms: The convolutional neural network incorrectly classifies a negative sample as positive.
Investigation and Resolution Protocol:
Inspect Test Line Characteristics:
- Visually inspect the false positive test line. Is it a faint, diffuse band versus a sharp, solid band in true positives? This could indicate non-specific binding.
Augment and Re-train the ML Model:
- Expand Training Dataset: Systematically collect more negative samples that produce these faint, non-specific lines.
- Implement Data Augmentation: Artificially create variations of your existing negative sample images (e.g., by adjusting brightness, contrast, or adding slight blur) to teach the model to ignore these artifacts. [29]
- Review Model Architecture: Ensure the CNN is deep enough to learn complex features but use techniques like dropout layers to prevent overfitting to minor, irrelevant image artifacts. [29]
Optimize Immunoassay Chemistry:
- Increase the concentration of the blocking agent (e.g., BSA, casein) in the running buffer and on the nitrocellulose membrane to reduce non-specific binding. [1]
- Titrate the concentration of the capture antibody on the test line to find the optimal level that maximizes specificity.
Problem 3: Poor Dynamic Range in an ML-Enhanced Biosensor
Symptoms: The biosensor and its ML model fail to accurately quantify analyte concentrations across a wide range, either saturating too early or lacking sensitivity at low concentrations.
Investigation and Resolution Protocol:
Characterize the Raw Biosensor Response:
- Perform a dose-response experiment without the ML model. Plot the raw output signal (e.g., voltage, fluorescence intensity, FRET ratio) against the analyte concentration on a log scale. [33] This will reveal the intrinsic dynamic range of the biosensor hardware.
Select an Appropriate ML Algorithm:
- For extending quantification, use regression-type supervised learning algorithms (e.g., Random Forest regression, Support Vector Regression) that are trained to map the complex input signal to a continuous concentration output. [30] [29]
- Ensure your training dataset is evenly populated with samples across the entire desired concentration range, including the upper and lower limits.
Engineer the Biosensor's Dynamic Range:
- If the hardware itself is the limitation, consider re-engineering the biosensor. For genetic biosensors, this can involve tuning promoter strength, ribosome binding sites, or the ligand-binding domain of the bioreceptor to adjust the sensor's operational range. [33]
Experimental Protocols
Protocol 1: Establishing a Training and Validation Dataset for ML Model Development
Purpose: To create a robust, high-quality dataset for training a machine learning model to recognize true biosensor signals and reject noise and false positives.
Reagents and Equipment:
- Functional biosensors (e.g., electrode strips, functionalized chips)
- Purified target analyte at known concentrations
- Negative control samples (blank buffer, sample matrix without analyte)
- Potential interfering substances relevant to the sample matrix
- Data acquisition system (potentiostat, fluorimeter, camera for colorimetric signals)
Methodology:
- Sample Preparation: Prepare a large set of samples (N > 100 is recommended for a good start). This set should include:
- A range of analyte concentrations spanning the expected dynamic range.
- Multiple replicates of negative controls.
- Samples containing common interferents at physiologically relevant concentrations.
- The exact number of samples required depends on the complexity of the task and the ML algorithm used.
Data Acquisition: For each sample, collect the raw signal output from your biosensor. For image-based sensors (e.g., LFAs), capture standardized images under consistent lighting conditions.
Data Labeling (for supervised learning): This is a critical step. Assign the "ground truth" label to each sample based on the known, prepared concentration, or a validated reference method. For example:
- Classification: Label as "Positive" or "Negative".
- Regression: Label with the exact concentration value.
Data Splitting: Randomly split the complete, labeled dataset into three distinct subsets [29]:
- Training Set (~60%): Used to train the ML model.
- Validation Set (~20%): Used to tune model hyperparameters and check for overfitting during training.
- Blind Test Set (~20%): Used only once for the final evaluation of the model's performance on unseen data.
Protocol 2: Validating an ML-Integrated Biosensor Using Upstream Regulators
Purpose: To rigorously test the specificity and dynamic response of a biosensor, particularly one reporting on dynamic cellular processes (e.g., GTPase activity), by co-expression with known activators and inhibitors. [32]
Reagents and Equipment:
- Cultured adherent cells (e.g., HEK293)
- DNA plasmids for:
- The biosensor itself
- A positive regulator (e.g., a constitutively active mutant or a guanine nucleotide exchange factor - GEF)
- A negative regulator (e.g., a dominant-negative mutant or a GTPase-activating protein - GAP)
- A non-functional control regulator
- 96-well microplate suitable for automated microscopy
- Automated fluorescence microscope
Methodology:
- Cell Transfection: Seed cells into a 96-well plate. Co-transfect the biosensor plasmid with a titration series of the regulator plasmids (positive, negative, and non-functional control). Keep the total DNA mass constant across wells using an empty vector. [32]
Image Acquisition: After an appropriate expression period, image the live cells using an automated microscope. Acquire images in the necessary channels (e.g., donor, FRET, and acceptor for a FRET biosensor).
Data Analysis:
- Calculate the biosensor's activity metric (e.g., FRET ratio) for each cell in each well.
- Plot the average biosensor activity against the mass of regulator DNA transfected.
- A valid and specific biosensor will show a strong, saturating increase in activity with the positive regulator, a decrease with the negative regulator, and no change with the non-functional control. [32]
Key Signaling Pathways and Workflows
Workflow of ML-Integrated Biosensor Data Analysis
This diagram illustrates the end-to-end pipeline for processing biosensor signals with machine learning, from raw data to actionable insights.
Data Preprocessing Pipeline for ML
This diagram details the critical data preprocessing steps required to prepare raw, noisy biosensor data for effective machine learning.
The Scientist's Toolkit: Research Reagent Solutions
This table lists key reagents and materials essential for developing and troubleshooting ML-integrated biosensor assays.
| Item | Function | Example Application |
|---|---|---|
| Positive/Negative Regulator Plasmids | To saturate and validate biosensor response range by providing maximal activation/inhibition. [32] | Co-transfection in cell-based assays to generate ground truth data for model training. [32] |
| Donor-only & Acceptor-only Biosensor Constructs | To measure and correct for spectral bleed-through in FRET-based optical biosensors. [32] | Essential control for calibrating fluorescence measurements and improving signal quantification. |
| Non-functional Control Regulators | To test for non-specific effects of protein overexpression on the biosensor signal. [32] | Serves as a critical negative control to confirm biosensor specificity. |
| High-Quality Blocking Agents | To reduce non-specific binding of detection reagents or analytes to the sensor surface. [1] | Minimizing false positives in immunoassays and aptamer-based sensors (e.g., BSA, casein). |
| Stable Reference Analytes | To generate consistent, reliable calibration curves for model training. | Creating a labeled training dataset with known ground truth concentrations. |
| Nanomaterial-enhanced Transducers | To boost the primary signal and improve the signal-to-noise ratio before ML analysis. [5] [30] | Using porous gold or graphene in electrochemical sensors; Au-Ag nanostars in SERS platforms. [5] |
Developing Dual-Mode Biosensors for Self-Validation and Cross-Checking
Conventional single-mode biosensors, despite their promising advancements, face significant challenges including signal noise, environmental variability, cross-reactivity, and calibration difficulties in miniaturized devices, all of which compromise their accuracy and reliability [2]. These limitations can lead to false positive and false negative results, which have substantial implications in clinical diagnostics, food safety, and drug development [1].
Dual-mode biosensors represent a transformative approach by integrating two complementary detection techniques within a single platform. This design allows for internal cross-validation of data, significantly reducing false results while providing reliable measurements in complex biological matrices [2]. The convergence of multiple sensing modalities enhances measurement accuracy, expands analyte detection capabilities, and improves sensitivity compared to single-mode systems [34] [2].
Frequently Asked Questions (FAQs): Core Concepts
Q1: What fundamentally distinguishes a dual-mode biosensor from a single-mode one? A dual-mode biosensor integrates two distinct transduction mechanisms (e.g., optical and electrochemical) to generate two independent signals for the same analyte. The key distinction is not merely having two outputs, but using these outputs for cross-validation and complementary data generation, thereby enhancing reliability and reducing the risk of false positives/negatives that plague single-mode systems [2].
Q2: How does cross-validation within a single biosensor improve diagnostic certainty? Cross-validation provides an internal mechanism for the sensor to "check itself." For example, a positive result is only confirmed if both detection modes generate a positive signal. This process significantly reduces false results caused by non-specific binding, matrix interference, or instrument calibration errors. The result from each mode can be used for cross-validation, and only a doubly confirmed positive or negative result is considered dependable [34] [2].
Q3: What are the most promising modality combinations for dual-mode detection? Recent research highlights several powerful combinations:
- Colorimetric and Photothermal: Leverages the photothermal effect of nanoparticles for quantitative measurement alongside visual color changes [34].
- Fluorescent and Colorimetric: Uses different signal generation mechanisms (e.g., SYBR Green I for fluorescence and streptavidin-modified alkaline phosphatase for colorimetry) for cross-validating detection [35].
- Electrochemical and Optical: Combines the high sensitivity of electrochemical detection with the visual interpretation or fingerprinting capability of optical methods [2].
Q4: What are the primary translational challenges for commercializing dual-mode biosensors? Key challenges include increased system complexity and cost, multistep fabrication processes, potential signal interference between modalities, and the need for precise calibration between different detection systems. Additionally, navigating regulatory approval for combination devices and ensuring user-friendly operation present significant hurdles [2].
Troubleshooting Guide: Common Experimental Issues
Signal Generation and Detection Issues
Problem: Inconsistent signals between the two detection modes.
- Potential Cause: Different optimal working conditions for each modality (e.g., buffer composition, pH, temperature).
- Solution: Systematically optimize the universal assay buffer by testing a range of pH and ionic strength conditions to find a compromise that maintains the activity of both recognition systems. Use a Design of Experiments (DoE) approach for efficient optimization.
- Prevention: During initial biosensor design, select modality pairs with compatible working requirements, such as CRISPR-Cas systems that can trigger both colorimetric and photothermal responses under the same conditions [34].
Problem: High background noise in one detection channel.
- Potential Cause: Non-specific adsorption of reagents or interference from complex sample matrices.
- Solution: Implement more stringent washing protocols and include blocking agents like BSA, casein, or specialized commercial blocking buffers. For sample analysis, incorporate purification steps or use sample dilution to reduce matrix effects.
- Verification: Test the biosensor with standard solutions in simple buffers versus spiked real samples to distinguish between assay and matrix-related issues [1].
Problem: One detection mode shows significantly lower sensitivity.
- Potential Cause: Improper ratio of shared recognition elements or incompatible signal amplification strategies.
- Solution: Titrate the concentration of common biorecognition elements (e.g., antibodies, CRISPR guide RNA) to find the optimal balance that supports both detection modalities. Consider adding a separate, non-interfering amplification step for the weaker signal.
- Example: In a CRISPR-dCas9 system, optimize the sgRNA concentration and the ratio of SYBR Green I to streptavidin-alkaline phosphatase to balance fluorescent and colorimetric signals [35].
Material and Fabrication Issues
Problem: Nanoparticle aggregation affecting both detection modalities.
- Potential Cause: Salt concentration in the assay buffer is too high, or improper functionalization of nanoparticle surfaces.
- Solution: When using gold nanoparticles (AuNPs), gradually introduce salt solutions or use buffers specifically designed to prevent aggregation. Ensure proper conjugation of probes to nanoparticles through characterization of conjugation efficiency via UV-Vis spectroscopy or gel electrophoresis.
- Prevention: Use surfactants or stabilizers in the nanoparticle storage solution, and characterize the hydrodynamic size and zeta potential of nanoparticles before assay implementation [34].
Problem: Poor reproducibility between different sensor batches.
- Potential Cause: Inconsistent fabrication procedures, particularly in manual modification steps.
- Solution: Standardize all fabrication steps with precise timing, temperature, and concentration controls. Implement rigorous quality control checks for each batch, including testing with positive and negative controls.
- Documentation: Maintain detailed Standard Operating Procedures (SOPs) for all fabrication and modification steps, including environmental conditions [2].
Data Interpretation Issues
Problem: Discrepant results between the two detection modes.
- Potential Cause: Different limits of detection or dynamic ranges for each modality, or cross-reactivity with interfering substances.
- Solution: Pre-establish decision rules for discrepant results, such as repeating the assay or using a confirmatory method. Characterize the dynamic range and limit of detection for each modality independently before integrating them.
- Analysis: If one signal is positive and the other negative, consider whether the analyte concentration falls within the detectable range of both modalities [2].
Problem: Calibration drift in one detection system over time.
- Potential Cause: Instability of reagents, evaporation of solutions, or fouling of sensor surfaces.
- Solution: Implement regular calibration checks using fresh standard solutions. For long-term assays, use sealed systems to prevent evaporation, and incorporate internal controls to monitor signal stability.
- Validation: Include calibration standards at the beginning and end of each assay run to detect and correct for drift [1].
Performance Data and Technical Specifications
Table 1: Performance Metrics of Representative Dual-Mode Biosensors
| Target Analyte | Detection Modes | Limit of Detection (LOD) | Dynamic Range | Assay Time | Reference |
|---|---|---|---|---|---|
| Salmonella spp. | Colorimetric & Photothermal | 1 CFU/mL | 1 - 108 CFU/mL | <60 min | [34] |
| S. typhimurium | Fluorescent & Colorimetric | 1 CFU/mL | 1 - 109 CFU/mL | ~90 min | [35] |
| BRCA-1 Protein | Electrochemical & Optical | 0.04 ng/mL | 0.05-20 ng/mL | ~30 min | [36] |
Table 2: Comparison of Biosensing Modalities for Dual-Mode Systems
| Transduction Method | Key Advantages | Common Limitations | Ideal Partner Modality |
|---|---|---|---|
| Colorimetric | Simple visualization, low cost, equipment-free readout | Lower sensitivity, subjective interpretation | Photothermal, Fluorescent |
| Photothermal | Quantitative, high sensitivity, uses portable reader | Requires thermal camera, potential background heating | Colorimetric, SERS |
| Fluorescent | High sensitivity, quantitative, multiplexing capability | Photobleaching, requires excitation source | Colorimetric, Electrochemical |
| Electrochemical | High sensitivity, miniaturization, low sample volume | Electroactive interferents, electrode fouling | Optical, SERS |
| SERS | Fingerprint capability, ultra-sensitive, multiplexing | Substrate reproducibility, complex data analysis | Electrochemical, Colorimetric |
Experimental Protocols for Dual-Mode Biosensing
CRISPR-Cas12a-Powered Dual-Mode Detection of Pathogenic Bacteria
This protocol adapts the methodology from Ma et al. for detecting pathogenic bacteria using a CRISPR-Cas12a system that generates both colorimetric and photothermal signals [34].
Principle: Target DNA (e.g., Salmonella-specific invA gene) activates the trans-cleavage activity of Cas12a, which indiscriminately degrades single-stranded DNA linkers that would otherwise connect gold nanoparticle (AuNP) probe pairs. This prevents AuNP aggregation, causing a color change from purple to red and altering the photothermal response under NIR irradiation.
Materials and Reagents:
- LbCas12a enzyme and specific crRNA
- AuNPs (20-30 nm)
- Single-stranded DNA linkers (complementary to AuNP probes)
- Loop-mediated isothermal amplification (LAMP) reagents
- NIR laser (808 nm) and thermal camera
- Centrifuge and portable colorimeter
Procedure:
- Sample Preparation and Amplification:
- Extract DNA from sample (bacterial culture, food homogenate, etc.)
- Amplify target sequence using LAMP with the following reaction mix:
- 1× LAMP reaction buffer
- 6 mM MgSO₄
- 1.4 mM dNTPs
- 0.8 µM FIP/BIP primers
- 0.2 µM F3/B3 primers
- 8 U Bst DNA polymerase
- Template DNA
- Incubate at 65°C for 45-60 minutes
CRISPR-Cas12a Reaction:
- Prepare Cas12a/crRNA complex by pre-incubating:
- 50 nM LbCas12a
- 60 nM crRNA (designed for invA target)
- 1× NEBuffer 2.1
- Incubate at 25°C for 10 minutes
- Add 5 µL of LAMP product to the Cas12a/crRNA complex
- Add 200 nM ssDNA reporter
- Incubate at 37°C for 30 minutes
- Prepare Cas12a/crRNA complex by pre-incubating:
Dual-Mode Detection:
- Colorimetric Mode:
- Add Cas12a reaction mixture to AuNP probe solution
- Observe color change visually or measure absorbance at 520/620 nm with portable colorimeter
- Photothermal Mode:
- Transfer mixture to a microcuvette
- Irradiate with 808 nm NIR laser (1.5 W/cm²) for 5 minutes
- Record temperature changes using thermal camera
- Calculate temperature change (ΔT) for quantification
- Colorimetric Mode:
Troubleshooting Notes:
- If no color change is observed: Verify Cas12a activity with synthetic DNA target and check AuNP functionalization.
- If photothermal signal is weak: Ensure proper NIR laser alignment and check for AuNP aggregation.
- High background in both modes: Increase washing steps or optimize Cas12a concentration to reduce non-specific trans-cleavage.
CRISPR-dCas9-Based Fluorescent and Colorimetric Detection
This protocol is based on the SCOUT-dCas9 system for S. typhimurium detection, which utilizes catalytically inactive Cas9 (dCas9) for target binding without cleavage [35].
Principle: Biotinylated LAMP amplicons of the target gene are specifically captured by dCas9-sgRNA complexes immobilized on a solid surface. The captured complexes are then detected using SYBR Green I (fluorescent signal) and streptavidin-modified alkaline phosphatase with BCIP/NBT substrate (colorimetric signal).
Materials and Reagents:
- dCas9 protein and specific sgRNA
- Streptavidin-modified magnetic beads
- SYBR Green I nucleic acid stain
- Streptavidin-modified alkaline phosphatase (SA-ALP)
- BCIP/NBT substrate
- LAMP reagents with biotinylated primer
- Microplate reader or portable spectrometer
Procedure:
- Ternary Complex Formation:
- Prepare dCas9-sgRNA complex by incubating 100 nM dCas9 with 120 nM sgRNA
- Immobilize the complex on streptavidin magnetic beads
- Add biotinylated LAMP amplicons and incubate for 20 minutes at 37°C
- Wash three times with PBS-Tween to remove unbound amplicons
- Dual-Signal Generation:
- Fluorescent Detection:
- Resuspend beads in SYBR Green I solution (1:100 dilution in TE buffer)
- Incubate for 5 minutes in the dark
- Measure fluorescence (excitation: 497 nm, emission: 520 nm)
- Colorimetric Detection:
- In parallel, add SA-ALP to the beads and incubate for 10 minutes
- Wash to remove unbound SA-ALP
- Add BCIP/NBT substrate and incubate for 15 minutes
- Measure absorbance at 405 nm or observe color development visually
- Fluorescent Detection:
Validation Steps:
- Include positive control (synthetic target DNA) and negative controls (non-target DNA, no template) in each run.
- For quantitative analysis, generate standard curves with known concentrations of target bacteria.
- Cross-validate results: both signals should correlate with target concentration.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Dual-Mode Biosensor Development
| Reagent/Category | Specific Examples | Function in Dual-Mode Biosensing |
|---|---|---|
| CRISPR Systems | Cas12a, Cas13a, dCas9 | Programmable recognition elements that can trigger multiple signal transduction pathways |
| Nanoparticles | Gold nanoparticles (AuNPs), Graphene-QDs, MoS₂ | Signal amplification, transducers for colorimetric, photothermal, and electrochemical detection |
| Enzymatic Reporters | Alkaline Phosphatase (ALP), Horseradish Peroxidase (HRP) | Generate both colorimetric and chemiluminescent signals with different substrates |
| Fluorescent Dyes | SYBR Green I, Ru(bpy)₃²⁺, Quantum Dots | Provide sensitive fluorescent signals that can be paired with other modalities |
| Signal Substrates | BCIP/NBT, TMB, Luminol | Convert enzymatic activity into detectable colorimetric, electrochemical, or luminescent signals |
| Transducer Materials | Screen-printed electrodes, Graphene FETs, SERS substrates | Convert biological recognition events into measurable electrical or optical signals |
Signaling Pathways and Experimental Workflows
CRISPR-Cas12a Dual-Mode Detection Workflow
Dual-Mode Result Interpretation Logic
Utilizing Nanomaterials and Surface Modifications to Minimize Non-Specific Adsorption
Core Concepts: Understanding Non-Specific Adsorption
What is non-specific adsorption (NSA) and why is it a critical issue in biosensor development?
Non-specific adsorption (NSA), also known as non-specific binding or biofouling, occurs when molecules other than your target analyte adhere to the biosensor's surface through physisorption rather than specific biorecognition [37]. This phenomenon presents a critical challenge because it generates background signals that are often indistinguishable from specific binding events, leading to:
- Increased false positives: Elevated background signals can be misinterpreted as positive detection [38] [39].
- Reduced sensitivity: NSA masks the detection of low-abundance analytes, raising the limit of detection [37] [39].
- Compromised accuracy and reproducibility: Fouling affects signal stability and reliability over time and across experiments [37] [39].
NSA is primarily driven by intermolecular forces, including hydrophobic interactions, ionic interactions, van der Waals forces, and hydrogen bonding between the sensor surface and non-target components in complex sample matrices like blood, serum, or milk [37] [39].
How can I quickly determine if my biosensor signal is affected by NSA?
A systematic workflow for evaluating potential NSA involves the following steps, which combine observational checks with controlled experiments [39]:
Key diagnostic experiments include:
- Blank sample analysis: Measure signal with sample matrix containing no target analyte.
- Surface comparison: Test both functionalized and non-functionalized surfaces with the same sample.
- Kinetic profiling: NSA often shows different binding kinetics compared to specific interactions.
- Negative controls: Use samples with known absence of target or non-target competing molecules.
Troubleshooting Guide: Solutions for NSA Reduction
What are the most effective surface modification strategies to prevent NSA?
Surface modification strategies can be broadly categorized into passive (preventive) and active (removal) methods. The table below summarizes the most effective approaches documented in recent literature:
Table: Comparison of NSA Reduction Methods
| Method Category | Specific Approach | Mechanism of Action | Reported Efficacy | Best For |
|---|---|---|---|---|
| Passive (Chemical) | Self-assembled monolayers (SAMs) | Creates dense, ordered molecular layer that sterically hinders approach | ~90% reduction in protein adsorption [40] | Glass, gold substrates |
| Passive (Chemical) | Polyethylene glycol (PEG) coatings | Forms hydrated barrier that resists protein adhesion | Up to 95% reduction in fouling [37] | Multiple substrates |
| Passive (Chemical) | Zwitterionic polymers | Creates superhydrophilic surface via strong hydration layer | >90% reduction in non-specific binding [39] | Complex biological samples |
| Passive (Chemical) | Negatively charged polymers (PSS, TSPP) | Electrostatic repulsion of negatively charged biomolecules | 300-400 fold reduction in QD adsorption [38] | Optical biosensors, glass substrates |
| Passive (Physical) | Blocking proteins (BSA, casein) | Occupies vacant surface sites before assay | Standard for ELISA; efficacy varies [37] | Immunoassays |
| Active Removal | Electromechanical transducers | Generates surface forces to shear away weakly adhered molecules | Effective for weakly bound molecules [37] | Microfluidic systems |
| Active Removal | Acoustic wave devices | Uses surface acoustic waves to remove non-specifically bound molecules | Improved signal-to-noise in complex samples [37] | Point-of-care devices |
My biosensor still shows high background after surface modification. What could be wrong?
Persistent NSA after surface modification often stems from these common pitfalls:
- Incomplete surface coverage: Even small uncovered areas can cause significant NSA.
- Sample matrix effects: Complex samples (serum, blood) require more robust antifouling strategies.
- Incorrect modification chemistry: The surface chemistry must be compatible with your substrate.
- Insufficient washing protocols: Inadequate removal of unbound molecules before detection.
Solutions:
- Characterize your modified surface using techniques like contact angle measurement, FTIR, or ellipsometry to verify complete modification [40] [41].
- Implement multi-layer protection, such as the TSPP/PSS system that demonstrated a 7.5-fold sensitivity improvement for CRP detection [38].
- Optimize blocking conditions including concentration, time, and temperature.
- Include detergent in wash buffers (e.g., 0.05% Tween-20) to reduce hydrophobic interactions.
Experimental Protocols: Detailed Methodologies
Protocol: Creating a Negatively Charged Polymer Coating on Glass Substrates
This protocol, adapted from Lv et al. [38], details the creation of a highly effective antifouling surface that reduced non-specific adsorption by 300-400 fold.
Principle: Sequential deposition of dense negatively charged films (SO₃²⁻) creates electrostatic repulsion against negatively charged biomolecules and nanoparticles.
Materials Needed:
- Clean glass substrates (soda-lime glass slides)
- Poly(styrene sulfonic acid) sodium salt (PSS)
- meso-tetra(4-sulfonatophenyl) porphine dihydrochloride (TSPP)
- Poly(diallyldimethylammoniumchloride) (PDDA)
- Piranha solution (3:1 H₂SO₄:H₂O₂) - EXTREME CAUTION
- Ultrapure water
Step-by-Step Procedure:
- Substrate Cleaning:
- Treat glass slides with piranha solution for 30 minutes at 80°C
- Rinse thoroughly with ultrapure water
- Dry under nitrogen stream
Surface Activation:
- Immerse cleaned slides in 2 mg/mL PDDA solution for 20 minutes
- Rinse with ultrapure water to remove excess PDDA
- Dry under nitrogen stream
Polymer Deposition - Option A (PSS only):
- Immerse PDDA-coated slides in 2 mg/mL PSS solution for 20 minutes
- Rinse thoroughly with ultrapure water
- Repeat for 4 layers total
- Dry under nitrogen stream
Polymer Deposition - Option B (TSPP/PSS hybrid):
- Immerse PDDA-coated slides in 0.05 mg/mL TSPP solution for 20 minutes
- Rinse with ultrapure water
- Repeat for 2 TSPP layers
- Continue with 4 PSS layers as in Option A
- Dry under nitrogen stream
Quality Control:
- Verify surface modification by measuring water contact angle (should decrease significantly)
- Confirm surface charge by zeta potential measurement (should be strongly negative)
- Test antifouling performance with fluorescently labeled BSA before proceeding with biosensor assembly
Applications: This coating is particularly effective for fluorescence-based immunosensors and quantum dot-based detection systems [38].
Protocol: Standardized Evaluation of Antifouling Performance
Purpose: Quantitatively assess the effectiveness of NSA reduction strategies to enable direct comparison between different approaches.
Materials:
- Your modified biosensor surface
- Appropriate negative control surface
- Fluorescently labeled BSA or other non-target protein
- Complex sample matrix (e.g., 10% serum, undiluted blood)
- Detection instrumentation (fluorescence reader, SPR, etc.)
Procedure:
- Sample Preparation:
- Prepare solution of fluorescently labeled BSA (0.1-1.0 mg/mL) in your typical assay buffer
- Prepare identical solution in complex matrix (e.g., 10% serum)
Incubation:
- Apply 100 μL of each solution to separate areas of your modified surface
- Incubate for 1 hour at room temperature
- Include appropriate positive and negative controls
Washing:
- Rinse surface 3 times with PBS containing 0.05% Tween-20
- Perform final rinse with pure PBS
Detection and Quantification:
- Measure signal from adsorbed fluorescent protein
- Calculate percentage reduction compared to unmodified surface
Calculation:
Interpretation:
- >90% reduction: Excellent antifouling performance
- 70-90% reduction: Good for most applications
- <70% reduction: May require optimization for complex samples
Research Reagent Solutions
Table: Essential Reagents for NSA Reduction Experiments
| Reagent/Chemical | Primary Function | Example Applications | Key Considerations |
|---|---|---|---|
| Poly(ethylene glycol) (PEG) | Forms hydrated anti-fouling barrier | Gold and silicon surface modification | Molecular weight affects layer density and performance |
| Poly(styrene sulfonic acid) sodium salt (PSS) | Creates negatively charged repulsive layer | Glass substrate modification [38] | Layer-by-layer assembly with cationic polymer required |
| Zwitterionic polymers | Superhydrophilic surface via strong hydration | SPR sensors, microfluidic chips [39] | Compatible with various transduction methods |
| Bovine Serum Albumin (BSA) | Blocking agent for vacant surface sites | ELISA, immunoassays [37] | Can denature on some surfaces, potentially increasing NSA |
| Casein | Protein-based blocking agent | Western blotting, lateral flow assays [37] | Effective for preventing NSA of various biomolecules |
| Aminosilanes | Surface functionalization for silica | Nanoparticle and glass substrate modification [40] | Provides amine groups for subsequent bioconjugation |
| Thiol-based linkers | Surface attachment to noble metals | Gold nanoparticle functionalization [40] [41] | Form strong Au-S bonds for stable monolayers |
Advanced Applications & Emerging Strategies
How can I integrate nanomaterials to enhance NSA reduction?
Nanomaterials offer unique advantages for NSA reduction due to their tunable surface chemistry and physical properties:
Nanoparticle Surface Functionalization [40] [41]:
- Core-shell structures: Create inert shells (SiO₂, PEG) around functional nanoparticles
- Mixed monolayer approaches: Combine different functional groups to optimize surface properties
- Biomimetic coatings: Use cell membrane derivatives to create "self" surfaces
Recent Advancements:
- Stimuli-responsive polymers: Switchable surfaces that can be "turned on" for sensing and "off" for cleaning
- Hybrid organic-inorganic coatings: Combine mechanical stability of inorganic materials with antifouling properties of organic polymers
- Machine learning-assisted design: Computational prediction of optimal surface chemistries for specific applications [39]
What are the future directions for NSA reduction in biosensing?
Emerging strategies focus on dynamic, adaptive, and intelligence-driven approaches [39]:
- Active removal integration: Combining passive prevention with real-time removal mechanisms
- Multi-modal protection: Simultaneously addressing multiple NSA mechanisms (electrostatic, hydrophobic, etc.)
- AI-optimized materials: Machine learning algorithms to design and predict antifouling performance
- Biomimetic innovations: Learning from natural antifouling systems (marine organisms, cell membranes)
The field is shifting from simple blocking strategies to sophisticated surface engineering approaches that maintain biosensor functionality while providing robust protection against NSA in complex real-world samples.
Implementing Microfluidic Systems for Automated and Controlled Assay Conditions
Technical Support Center
Frequently Asked Questions (FAQs)
FAQ 1: What are the common sources of false positives in microfluidic biosensors? False positives can arise from multiple sources, including nonspecific binding of biorecognition elements (like antibodies or aptamers) to non-target molecules or the chip surface, cross-reactivity in multiplexed assays, and signal interference from sample matrix components [1] [42]. Inadequate washing steps that fail to remove unbound substances can also lead to false signals.
FAQ 2: How does the choice of microfluidic chip material influence assay performance? The chip material significantly impacts performance due to its optical properties, biocompatibility, and potential for nonspecific adsorption. Materials like PDMS are popular due to their optical transparency and flexibility but are prone to nonspecific protein adsorption, which can increase background noise or false positives [43]. Alternative materials like PMMA or glass offer different advantages and limitations, as detailed in the table below [43].
FAQ 3: What role do nanomaterials play in reducing false signals? Nanomaterials such as gold nanoparticles (AuNPs), carbon nanotubes (CNTs), and graphene can enhance biosensor sensitivity and selectivity [44]. Their high surface-to-volume ratio allows for more efficient immobilization of biorecognition elements, which can reduce nonspecific binding. Furthermore, they can improve electron transfer in electrochemical sensors and enhance optical signals, contributing to a higher signal-to-noise ratio [44].
FAQ 4: How can I validate a negative result in my microfluidic assay? It is crucial to incorporate appropriate controls. Always run a positive control (a sample known to contain the target analyte) to confirm the assay is functioning correctly. A negative control (a sample known to be devoid of the target) should be used to establish the baseline signal and identify any contamination or nonspecific binding contributing to false positives [1]. For CRISPR-based systems, a crRNA known to not target any sequence in the sample can serve as a negative control [45].
FAQ 5: Can fluid flow dynamics within the microchip cause inaccurate results? Yes, improper fluidic control can lead to inconsistent mixing of samples and reagents, formation of air bubbles, or uneven washing. These issues can cause variations in reaction times and signal intensities, leading to both false positives and false negatives [46]. Ensuring a well-designed microchannel structure and optimized flow rates is essential for reproducible results.
Troubleshooting Guides
Issue 1: High Background Signal or Frequent False Positives
| Probable Cause | Recommended Action | Underlying Principle |
|---|---|---|
| Nonspecific Adsorption | Use surface passivation agents (e.g., bovine serum albumin (BSA) or casein) to block active sites on the chip surface [43]. | Blocking agents occupy nonspecific binding sites, preventing biomolecules from adhering to the chip surface and causing background noise [43]. |
| Contaminated Reagents | Prepare fresh reagents, use nuclease-free water, and aliquot reagents to minimize freeze-thaw cycles. | Contaminants can act as unintended substrates for enzymatic reactions or bind to detection elements, generating a false signal. |
| Insufficient Washing | Optimize wash buffer composition (e.g., include mild detergents like Tween-20) and increase washing cycle volume or duration. | Effective washing removes unbound reagents and loosely adsorbed molecules that contribute to background signal [42]. |
| Cross-reactivity | Re-validate the specificity of biorecognition elements (e.g., antibodies, aptamers). For multiplex assays, ensure primer and crRNA sequences are highly specific to their targets [45]. | Biorecognition elements with low specificity can bind to similar, non-target analytes, producing a false positive signal [1] [45]. |
Issue 2: Low Signal or False Negatives
| Probable Cause | Recommended Action | Underlying Principle |
|---|---|---|
| Bioreceptor Inactivity | Check storage conditions of antibodies/aptamers/enzymes. Avoid repeated freezing and thawing. Use fresh aliquots. | Bioreceptors can denature or lose activity over time, preventing successful recognition and binding of the target analyte. |
| Clogged Microchannels | Inspect channels under a microscope. Filter all samples and buffers before loading. Increase channel diameter if design allows. | Blockages impede the flow of the sample to the detection zone, preventing the target analyte from reaching the bioreceptor. |
| Sub-optimal Assay Conditions | Re-optimize incubation times, temperature, and pH. Refer to the manufacturer's data sheet for bioreceptors. | Each bioreceptor and assay chemistry has an optimal operating window. Deviations can reduce the efficiency of the binding reaction [46]. |
| Signal Transducer Failure | Calibrate detection equipment (e.g., photodetector, potentiostat). Ensure the transducer surface is clean and functional. | A malfunctioning transducer cannot properly convert the biological binding event into a quantifiable electrical or optical signal. |
Issue 3: Inconsistent Results Between Replicates
| Probable Cause | Recommended Action | Underlying Principle |
|---|---|---|
| Inconsistent Flow Rates | Calibrate syringe or peristaltic pumps. Use integrated pressure controllers for more stable flow. Check for and remove air bubbles. | Fluctuations in flow rate cause variations in incubation and reaction times, leading to poor reproducibility [46]. |
| Bubble Formation | Degas buffers before use. Incorporate bubble traps into the microfluidic design. | Air bubbles can block microchannels, create flow resistance, and act as optical barriers in detection systems. |
| Non-uniform Surface Chemistry | Standardize the surface modification and bioreceptor immobilization protocol across all chips. | Inconsistent coating of the chip surface or immobilization of bioreceptors leads to varying amounts of active capture sites, affecting assay uniformity [43]. |
Experimental Protocols for Key Investigations
Protocol 1: Systematic Evaluation of Chip Material Impact on Nonspecific Binding
Objective: To quantitatively compare different microfluidic chip materials for their propensity to cause nonspecific binding, a common source of false positives.
Materials:
- Chip materials: PDMS, PMMA, glass, and paper-based devices (μPADs).
- Blocking solutions: 1% BSA, 1% casein in PBS.
- Sample: A solution containing a non-target protein (e.g., 100 µg/mL BSA in buffer).
- Detection: Fluorescence scanner or microscope.
Methodology:
- Fabrication: Fabricate identical microchannel designs using PDMS (via soft lithography), PMMA (via laser cutting), glass (via etching), and paper (via wax printing) [43].
- Blocking: Divide the chips into two groups. Treat one group with a blocking agent and leave the other unblocked. Incubate for 1 hour at room temperature.
- Exposure: Flush all chips with the non-target protein solution and incubate for 30 minutes.
- Washing: Rinse the channels with PBS-Tween 20 wash buffer.
- Detection & Analysis: Measure the signal from each channel. The signal in the unblocked chips represents the maximum nonspecific binding. The reduction in signal in the blocked chips indicates the efficacy of the blocking agent for each material.
Protocol 2: crRNA Specificity Validation for CRISPR-Cas12a-based Detection
Objective: To confirm that crRNAs used in a multiplexed microfluidic assay (like MiCaR) only activate Cas12a collateral activity upon binding to their correct DNA target, minimizing false positives [45].
Materials:
- Purified DNA samples for all target subtypes (e.g., HPV-16, HPV-18, etc.) and non-target but similar subtypes.
- Cas12a enzyme.
- Designed crRNA for each target.
- Fluorescent ssDNA reporter (e.g., FAM-TTATT-BHQ1).
- Microfluidic chip designed for multiplexing (e.g., a hub-and-spoke SS-Chip) [45].
- Fluorescence imager.
Methodology:
- Pre-loading: Load different Cas12a/crRNA complexes into separate reaction wells on the microfluidic chip.
- Assay Setup: Introduce a single DNA target into the central hub, which will be distributed to all wells [45].
- Incubation: Allow the CRISPR reaction to proceed for 30-60 minutes at 37°C.
- Imaging: Capture fluorescence images of the chip.
- Analysis: A positive fluorescence signal should only appear in the wells containing the crRNA that is a perfect match to the introduced DNA target. Any signal in wells with non-matching crRNAs indicates off-target activity and a potential source of false positives.
Table 1: Comparison of Common Microfluidic Chip Materials [43]
| Material | Optical Transparency | Cost | Ease of Fabrication | Nonspecific Binding | Key Characteristics |
|---|---|---|---|---|---|
| Polydimethylsiloxane (PDMS) | High | Low | Moderate | High (requires blocking) | Gas-permeable, flexible, widely used in prototyping. |
| Polymethylmethacrylate (PMMA) | High | Low | Moderate | Low | Good mechanical strength, biocompatible. |
| Glass | Very High | High | Difficult | Very Low | Excellent chemical resistance, low autofluorescence. |
| Silicon | Opaque | High | Difficult | Low | High thermal stability, primarily used for electronics. |
| Paper (μPADs) | Low | Very Low | Easy | Moderate | Power-free capillary flow, disposable, high plasticity. |
Table 2: Performance Metrics of Advanced Microfluidic Biosensing Platforms
| Platform / Technology | Detection Limit | Multiplexing Capacity | Assay Time | Key Application | Reference |
|---|---|---|---|---|---|
| MiCaR (CRISPR-Cas12a) | 0.26 attomole | 30 targets (with one probe) | ~40 minutes | HPV subtyping, respiratory viruses | [45] |
| Color-based MF-AST | N/A (phenotypic) | Multiple antibiotics | Faster than traditional AST | Antimicrobial Susceptibility Testing | [46] |
| Electrochemical Biosensors | High (varies) | Moderate | Minutes to Hours | Cancer biomarkers (e.g., ctDNA) | [44] |
Research Reagent Solutions
Table 3: Essential Materials for Microfluidic Biosensor Development and Troubleshooting
| Item | Function | Example in Context |
|---|---|---|
| Blocking Agents (BSA, Casein) | Reduces nonspecific binding by occupying reactive sites on the chip surface. | Used to passivate PDMS chips to prevent false positives from protein adsorption [43]. |
| crRNAs / Primers | Provides target specificity in CRISPR-based and amplification-based assays. | Designed to uniquely identify HPV subtypes in the MiCaR platform; specificity is key to avoiding cross-reactivity [45]. |
| Fluorescent Reporters | Generates a measurable signal upon target recognition (e.g., cleavage by activated Cas12a). | A fluorophore-quencher-labeled ssDNA reporter is used to detect Cas12a collateral activity [45]. |
| Nanomaterials (AuNPs, Graphene) | Enhances signal transduction and immobilization of biorecognition elements. | Gold nanoparticles (AuNPs) can enhance electrochemical signals, lowering detection limits for cancer biomarkers [44]. |
| Surface Modification Reagents | Chemically alters the chip surface to enable stable bioreceptor immobilization. | Used to create functional groups on PMMA or glass for covalent attachment of antibodies [43]. |
Workflow and System Diagrams
Assay Workflow
False Positive Diagnosis
Designing Aptamer-Based Assays for Improved Stability and Target Selectivity
Core Concepts and Frequent Challenges
Why is my aptamer-based biosensor producing false positive signals?
False positives in aptamer-based assays often arise from the aptamer's interaction with non-target components in the sample matrix, its inherent structural instability, or suboptimal assay conditions. The table below summarizes common causes and their underlying reasons.
Table 1: Common Causes of False Positive Results in Aptamer-Based Assays
| Cause of False Positive | Underlying Reason | Impact on Assay |
|---|---|---|
| Non-Specific Binding [47] | Aptamer interacts with assay matrix components (e.g., proteins, lipids) or surfaces. | Skewed experimental results, reduced signal-to-noise ratio, inaccurate quantification. |
| Aptamer Instability/Degradation [48] | Nucleases in the sample degrade the aptamer, leading to fragments that bind unpredictably. | Loss of specific signal, generation of deceptive signals from fragment binding, poor reproducibility. |
| Inappropriate Assay Stringency [47] | Buffer conditions (ionic strength, pH, cations) do not favor highly specific target binding. | Increased off-target interactions, failure to discriminate between closely related targets. |
| Cross-Reactivity [47] | The aptamer binds to molecules structurally similar to the intended target. | False identification of analyte presence, incorrect diagnostic or research conclusions. |
How can I improve the stability of my aptamer for in vitro assays?
Aptamer stability is critical for reliable assay performance. Stability can be compromised by nuclease degradation, chemical degradation, and conformational instability. The following strategies can significantly enhance aptamer robustness [49] [48] [50].
Table 2: Strategies for Enhancing Aptamer Stability
| Strategy | Method | Function |
|---|---|---|
| Backbone Modification | Replacing phosphate oxygen with sulfur (thiophosphate or dithiophosphate) [50]. | Reduces degradation by nucleases and can increase relative affinity to target proteins. |
| Sugar Group Modification | Incorporating 2'-fluoro (2'-F) or 2'-O-methyl ribose analogues into RNA aptamers [50]. | Protects against nuclease cleavage and enhances serum stability. |
| Terminal Capping | Adding an inverted thymidine or other molecule to the 3' end [49]. | Blocks exonuclease activity, a primary pathway for aptamer degradation. |
| Conversion to DNA Analogue | Converting a native RNA aptamer sequence into a modified DNA aptamer [50]. | Leverages the innate higher stability of DNA while maintaining binding function. |
| Conjugation | Covalently linking a polymer like Polyethylene Glycol (PEG) to the 5' end [50]. | Improves pharmacokinetics by reducing renal clearance and nuclease hydrolysis. |
The following diagram illustrates the key decision points for selecting an appropriate stability optimization strategy.
Troubleshooting Guides
Guide 1: Troubleshooting High Background and Non-Specific Binding
Problem: The assay shows a high signal even in the absence of the target analyte.
Investigation and Resolution Steps:
Verify Assay Matrix Compatibility:
- Action: Run a negative control (blank) containing only the sample matrix (e.g., serum, buffer) without the target.
- Solution: If the background is high, incorporate non-specific competitors like carrier DNA/RNA (e.g., yeast tRNA, salmon sperm DNA) or inert proteins (e.g., BSA) into the assay buffer to block non-specific sites [47].
Optimize Buffer Conditions for Stringency:
Check Aptamer Purity and Integrity:
Guide 2: Troubleshooting Low Signal and Poor Target Selectivity
Problem: The signal is weak, or the aptamer fails to distinguish between the target and closely related molecules.
Investigation and Resolution Steps:
Confirm Aptamer Affinity and Conformation:
- Action: Use Surface Plasmon Resonance (SPR) or Isothermal Titration Calorimetry (ITC) to measure binding affinity (KD) and kinetics.
- Solution: If affinity is low, consider re-selecting the aptamer under more stringent conditions or performing post-SELEX optimization through truncation to identify the minimal functional sequence [51].
Validate Target Engagement Site:
- Action: If the goal is inhibition (e.g., of an enzyme), ensure the selection process directed aptamers to the active site.
- Solution: For inhibitory functions, the discovery process must be modified to direct aptamers to the functionally critical site on the target protein [47].
Assess Conformational Change:
- Action: For signaling aptamers (signaling probes), ensure the binding event induces a sufficient conformational change.
- Solution: Re-design the aptamer probe architecture or select a different aptamer sequence with a more robust structural switch upon target binding.
Experimental Protocols for Validation
Protocol 1: Analyzing Aptamer Stability in Biological Matrices
Objective: To evaluate the stability and half-life of an aptamer in a complex biological fluid like serum.
Materials:
- Aptamer (unmodified and chemically modified versions)
- Fetal Bovine Serum (FBS)
- Incubator or water bath set to 37°C
- Proteinase K
- Phenol-chloroform or commercial cleanup kit
- Denaturing Polyacrylamide Gel Electrophoresis (PAGE) system
Methodology:
- Incubation: Mix the aptamer with FBS (e.g., 95% serum) and incubate at 37°C.
- Sampling: Withdraw aliquots at defined time points (e.g., 0, 1, 2, 4, 8, 24 hours).
- Reaction Termination: Add Proteinase K to digest proteins, then extract the aptamer using phenol-chloroform or a cleanup kit.
- Analysis: Resolve the extracted aptamers on denaturing PAGE. The intensity of the full-length band over time indicates stability. Compare degradation rates between modified and unmodified aptamers [48].
Protocol 2: Assessing Target Selectivity and Cross-Reactivity
Objective: To confirm that the aptamer binds specifically to the intended target and not to related interferents.
Materials:
- Purified target protein
- Purified related proteins (e.g., family members, proteins with similar domains)
- Assay buffer
- Method for detecting binding (e.g., SPR, ELISA-type plate reader, fluorescence anisotropy)
Methodology:
- Immobilization: Immobilize the aptamer on a sensor chip (for SPR) or a microplate well.
- Binding Test: Expose the immobilized aptamer to a solution containing the target protein and record the binding signal.
- Cross-Reactivity Test: In separate experiments, expose the aptamer to the same concentration of non-target, closely related proteins.
- Data Interpretation: High signal with the target and negligible signal with non-targets confirm high selectivity. Significant binding to non-targets indicates cross-reactivity, necessitating counter-selection or further optimization [47].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Aptamer Assay Development and Troubleshooting
| Reagent / Material | Function in Assay Development |
|---|---|
| 2'-Fluoro Pyrimidine NTPs | Raw materials for in vitro transcription of nuclease-resistant RNA aptamers [50]. |
| Thiophosphate Nucleotides | Building blocks for synthesizing aptamers with backbone modifications to enhance stability and affinity [50]. |
| Polyethylene Glycol (PEG) | Polymer for 5'-end conjugation to reduce renal clearance and improve in vivo half-life [50]. |
| Magnetic Beads (Streptavidin) | Solid support for immobilizing biotinylated targets during SELEX or for developing capture assays [51]. |
| Carrier DNA/RNA (e.g., yeast tRNA) | Used as a non-specific competitor in assay buffers to reduce background from non-specific binding [47]. |
| Surface Plasmon Resonance (SPR) Chip | Sensor surface for real-time, label-free analysis of aptamer-target binding affinity and kinetics [48]. |
The workflow for developing a robust and selective aptamer-based assay, from selection to validation, is summarized below.
Frequently Asked Questions (FAQs)
What is the single most critical factor in minimizing false positives from the start?
Incorporating counter-targets during the SELEX process is paramount. By including non-target molecules (e.g., related proteins, sample matrix components) in the selection buffer, you actively drive the evolution of aptamers that can distinguish the target from potential interferents, building selectivity directly into the aptamer sequence [47] [51].
Can I convert an existing RNA aptamer into a more stable DNA version?
Yes, this is a validated strategy. Research has demonstrated the successful conversion of an RNA aptamer targeting phospho-AXL into a modified DNA aptamer. The process involves synthesizing the DNA sequence with strategic modifications, such as 2'-fluoro pyrimidines and dithiophosphate groups, which resulted in improved stability and robust anti-tumor effects in models [50].
How does aptamer truncation help, and when should I do it?
Truncation identifies the minimal sequence essential for target binding, removing redundant nucleotides. This reduces production costs and can improve binding affinity and specificity by eliminating parts of the sequence that may contribute to non-specific interactions. It is a key post-SELEX optimization step performed after initial aptamer selection [51].
Are aptamers less stable than antibodies?
Unmodified DNA aptamers are generally more stable than antibodies, especially against heat denaturation, and can be renatured easily. Unmodified RNA aptamers are less stable due to RNase degradation. However, with chemical modifications, both DNA and RNA aptamers can achieve high stability, often surpassing that of antibodies in diagnostic applications [49].
A Systematic Workflow for Diagnosing and Correcting False Positives
FAQs on Root Cause Analysis for Biosensor Research
What is Root Cause Analysis (RCA) and why is it important for biosensor research?
Root Cause Analysis (RCA) is a structured process for identifying the underlying, fundamental reason a problem occurred, rather than just addressing surface-level symptoms [52]. In biosensor research, effective RCA helps to [52]:
- Prevent repeat problems by eliminating the true source of error.
- Improve systems and processes surrounding assay development and validation.
- Reduce downtime and rework by implementing long-lasting solutions.
- Boost reliability and accuracy of diagnostic results, which is critical in medical and drug development settings.
When should I use the 5 Whys versus a Fishbone Diagram for troubleshooting my assay?
The choice depends on the nature and complexity of the problem you are facing. The table below summarizes the key differences:
| Criteria | 5 Whys | Fishbone Diagram |
|---|---|---|
| Approach | Linear, follows a single cause-and-effect chain [52] | Visual, multi-dimensional, and structured [52] |
| Problem Complexity | Best for simple or moderately difficult issues with a suspected linear causality [52] [53] | Ideal for complex, multifaceted problems with many potential causes [52] |
| Collaboration | Works well with small teams or individuals with direct process knowledge [52] | Highly collaborative; excellent for cross-functional teams to gain diverse perspectives [52] [54] |
| Best Use Case | When the problem is well-defined and you need a quick, straightforward analysis [53] | When the root cause is unclear and you need to brainstorm all possible contributing factors from different categories (e.g., Materials, Methods, Equipment) [52] [54] |
How do I perform a 5 Whys analysis on a false positive result?
The 5 Whys method involves iteratively asking "Why?" to peel back the layers of a problem. The following workflow outlines the process, using a hypothetical biosensor false positive scenario.
Step-by-Step Application:
- Define the Problem: Clearly state the issue. Example: "The biosensor assay is producing false positive results for negative control samples." [53] [55]
- Ask the First "Why?": Why are there false positives? Answer: The detection antibody is exhibiting non-specific binding.
- Ask the Second "Why?": Why is the detection antibody exhibiting non-specific binding? Answer: The assay wash steps are insufficient to remove unbound antibody.
- Ask the Third "Why?": Why are the wash steps insufficient? Answer: The ionic strength of the wash buffer is too low to disrupt weak, non-specific interactions.
- Ask the Fourth "Why?": Why is the ionic strength of the wash buffer too low? Answer: The buffer was prepared according to an outdated protocol that does not account for the new antibody's isoelectric point.
- Identify the Root Cause: The root cause is an incorrect buffer preparation protocol.
- Develop and Implement a Solution: Update the standard operating procedure (SOP) for buffer preparation, specifying the correct ionic strength, and validate the new protocol [53] [55].
How do I create and use a Fishbone Diagram to investigate inconsistent biosensor performance?
A Fishbone Diagram (also known as an Ishikawa or Cause-and-Effect Diagram) helps you visually brainstorm all potential causes of a problem. For biosensor research, you can adapt standard categories to fit a laboratory context. The diagram below illustrates the structure and application of this method.
Process for a Fishbone Analysis Session:
- Define the Problem Statement: Be specific and place it in the "head" of the fish. Example: "High inter-assay coefficient of variation (CV) for positive control samples." [54] [56]
- Select Cause Categories: Use standard or customized categories. For biosensors, common categories are People, Methods, Materials, Equipment, Environment, and Measurement [52] [54].
- Brainstorm Potential Causes: Gather a cross-functional team (e.g., researchers, lab technicians) and brainstorm all possible causes for each category [52] [54].
- Methods: Unoptimized incubation times, unclear SOP.
- Materials: Lot-to-lot reagent variability, contaminated buffers.
- Equipment: Sensor surface fouling, fluctuation in detector voltage.
- People: Insufficient training, variation in pipetting technique.
- Environment: Temperature fluctuations in the lab, high ambient dust.
- Measurement: Improper calibration, high background noise.
- Prioritize and Investigate: After brainstorming, the team should discuss and prioritize the most likely causes. Use data and experiments to validate or rule out each hypothesis [54].
What are common pitfalls to avoid when using these RCA methods?
For the 5 Whys:
- Stopping too soon: The number five is a guideline; continue until you find a fundamental process or system failure [53].
- Assigning blame: The goal is to find a faulty process, not a person. Avoid answers that end with "...because Technician X made a mistake." [53]
- Lack of validation: The final root cause is a hypothesis. You must test it by implementing a fix and monitoring if the problem recurs [53] [55].
For the Fishbone Diagram:
- Poor problem definition: A vague problem statement leads to an unfocused and ineffective diagram [54].
- Unbalanced team: Failing to include people with hands-on experience can lead to theoretical rather than practical causes being identified [52] [54].
- Analysis paralysis: The diagram can become overwhelming. The goal is not to list every conceivable cause, but to identify the most likely ones for further investigation [52].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key materials used in biosensor research, the management of which is often a source of problems uncovered by Root Cause Analysis.
| Item | Function in Biosensor Assays | Common RCA-Related Considerations |
|---|---|---|
| Bioreceptors (e.g., antibodies, aptamers, enzymes) [1] | The biological element that specifically interacts with the target analyte (e.g., a protein biomarker). | Stability, binding affinity, specificity, and lot-to-lot consistency are frequent root causes of false positives/negatives. |
| Detection Antibodies (if used) | Used in sandwich assays to generate a signal after the primary bioreceptor has captured the analyte. | Non-specific binding or cross-reactivity can lead to false signals. Validation is critical. |
| Sensor Chip / Solid Support | The surface on which the bioreceptor is immobilized. | Surface chemistry, fouling, and non-specific protein adsorption can severely impact assay performance. |
| Assay Buffers (e.g., running, wash, regeneration buffers) | Maintain optimal pH and ionic strength for molecular interactions; wash away unbound material. | Composition, pH, and ionic strength are common root causes for issues with non-specific binding and signal strength. |
| Analyte Standard / Calibrator | A known quantity of the substance being measured, used to create a calibration curve. | Purity, stability, and accurate preparation are essential for reliable quantitative results. |
| Blocking Agents (e.g., BSA, casein) | Used to coat unused binding sites on the sensor surface to prevent non-specific binding. | The choice and concentration of blocking agent are vital for minimizing background noise. |
| Signal Generation Reagents (e.g., fluorescent dyes, enzyme substrates) | Produce a measurable signal (optical, electrochemical) proportional to the amount of analyte bound. | Stability and reaction efficiency can be a source of signal drift or inconsistency. |
Step-by-Step Experimental Troubleshooting for Label-Free Biosensors
Core Concepts: Understanding Your Biosensor and False Positives
Label-free biosensors are analytical devices that detect the interaction between a target analyte and a biological recognition element without the need for fluorescent or radioactive labels. They translate this binding event into a measurable signal using transducers that detect changes in mass, refractive index, or electrical properties at the sensor surface [1] [57]. While offering the advantage of studying biomolecules in their native state, these systems are susceptible to false positives—signals that mimic a specific binding event but are caused by non-specific interactions, matrix effects, or instrument artifacts [1]. This guide is designed to help you systematically identify and resolve the root causes of these false positives.
FAQ: Fundamental Questions on False Positives
Q1: What is the most common source of false positives in label-free biosensing? A: Non-specific binding (NSB) is the most frequent culprit. This occurs when non-target molecules in your sample matrix (e.g., proteins, lipids, or contaminants) adhere to the sensor surface or the capture ligand, generating a signal indistinguishable from specific binding [1] [18]. The sensor cannot intrinsically differentiate between the mass of your target and the mass of a contaminant.
Q2: My positive control works, but my sample gives a high background. What should I check? A: This strongly points to sample matrix effects. Complex biological samples like serum, saliva, or lysates contain many components that can interact with the sensor surface. Begin by ensuring your running buffer and sample matrix are perfectly matched and that you have implemented a rigorous surface blocking step after immobilizing your capture ligand [18] [58].
Q3: Can a faulty sensor surface cause false positives? A: Absolutely. An improperly functionalized or contaminated sensor surface is a major source of error. Inconsistent coating of the capture ligand, unstable immobilization, or leftover contaminants from manufacturing can all lead to high background noise and drift, which may be misinterpreted as a positive signal [59] [58]. Always inspect the baseline stability before sample injection.
Troubleshooting Guide: Diagnosing and Solving Common Issues
Use the following flowcharts and tables to diagnose your experimental issues.
Diagnosis Workflow
The following diagram outlines a logical pathway to diagnose the source of false positives in your label-free biosensor experiments.
Experimental Protocol: Surface Preparation and Blocking
A robust surface functionalization protocol is your first defense against false positives. The following workflow is adapted from a validated protocol for an electrochemical impedance biosensor [59].
Title: Step-by-Step Protocol for Sensor Surface Functionalization and Blocking Objective: To immobilize a capture ligand (e.g., antibody) on a biosensor surface while minimizing non-specific binding. Materials: ZnO/Au electrode (or other suitable sensor surface), DTSSP crosslinker, monoclonal antibody, SuperBlock Blocking Buffer, 1x PBS, deionized water [59].
Quantitative Performance Metrics
Familiarity with key performance parameters allows you to benchmark your sensor and identify deviations that could lead to false interpretations. The table below summarizes the expected performance of a well-functioning label-free biosensor, based on a real-world example for pathogen detection [59].
Table 1: Key Analytical Performance Metrics for a Validated Label-Free Biosensor
| Performance Parameter | Target Value | Description & Troubleshooting Implication |
|---|---|---|
| Limit of Detection (LOD) | 9 CFU/mL [59] | The lowest analyte concentration that can be reliably detected. A shift to a higher LOD suggests loss of sensitivity, potentially due to ligand degradation. |
| Assay Time | 5 minutes [59] | Time from sample injection to result. Drift or instability over this period can cause false readings. |
| Coefficient of Variation (%CV) | <20% [59] | Measure of reproducibility (both inter- and intra-assay). A high %CV indicates poor surface consistency or pipetting errors. |
| Positive Predictive Value (PPV) | >85% [59] | The probability that a positive result is a true positive. A low PPV is a direct indicator of a high false positive rate. |
The Scientist's Toolkit: Essential Reagents and Materials
The following reagents are critical for developing robust and reliable label-free biosensor assays.
Table 2: Key Research Reagent Solutions for Label-Free Biosensing
| Reagent/Material | Function & Role in Troubleshooting |
|---|---|
| High-Purity Capture Ligands (e.g., antibodies, aptamers) | The specificity of the assay originates here. Use affinity-purified ligands with documented specificity to minimize cross-reactivity. Ligand batch variability is a common source of inconsistency [57]. |
| Chemical Crosslinkers (e.g., DTSSP, sulfo-HSAB) | Provides a stable covalent bond between the sensor surface and the capture ligand, preventing ligand leakage which can cause signal drift and false positives [59]. |
| Commercial Blocking Buffers (e.g., SuperBlock, BSA, casein) | Critical for passivating the sensor surface after ligand immobilization. They adsorb to remaining bare surfaces, preventing non-specific binding of sample components [59] [18]. |
| Nanomaterial-Enhanced Surfaces (e.g., ZnO/Au, AuNPs, graphene) | Used to modify the transducer surface to increase the active surface area and improve signal transduction. This enhances sensitivity and can lower the LOD. Inconsistent nanomaterial synthesis can lead to variable performance [59] [57]. |
| Validated Positive & Negative Controls | Essential for every experiment. A positive control confirms the system is working. A negative control (e.g., a sample without the analyte or with a scrambled aptamer) directly measures the level of non-specific binding and is key to quantifying false positives [1] [60]. |
Advanced Troubleshooting: Sensor Technology-Specific Issues
Different biosensor transduction principles have unique failure modes. The table below outlines common issues based on the sensing technology.
Table 3: Technology-Specific Challenges and Solutions
| Biosensor Type | Common False Positive Triggers | Mitigation Strategies |
|---|---|---|
| Electrochemical (e.g., EIS) | Redox-active impurities in sample or buffer [18]; electrode fouling [58]. | Use ultra-pure reagents; employ non-Faradaic EIS to avoid redox probes [59]; implement electrode cleaning protocols. |
| Optical (e.g., SPR) | Bulk refractive index shift from buffer mismatch [61] [18]; air bubbles in microfluidics [58]. | Precisely match buffer composition between sample and running buffer; degas buffers; use reference channel for subtraction. |
| Piezoelectric (e.g., QCM) | Viscosity changes in the sample [58]; non-rigid mass binding [58]. | Ensure sample and standard matrices are identical; use models that account for viscoelastic effects. |
Optimizing Bioreceptor Immobilization and Surface Blocking Protocols
Troubleshooting Guide & FAQs for Researchers
This technical support center addresses common challenges in biosensor development, specifically focusing on mitigating false positives and enhancing assay reliability through optimized bioreceptor immobilization and surface blocking. The guidance is framed within the context of advanced research for troubleshooting biosensor assays.
Frequently Asked Questions (FAQs)
1. What is the primary cause of non-specific binding in label-free biosensors, and how can it be mitigated? Non-specific binding occurs when molecules interact with the sensor surface in an undesired, non-target manner. This acts as background noise, interfering with the accurate detection of the specific target signal and leading to false positives [62]. Mitigation is achieved through an optimized blocking step, where a blocking buffer occupies all non-specific binding sites on the assay surface before the introduction of the sample [62].
2. How does the choice of blocking buffer impact my assay's performance? The choice of blocking buffer directly influences the signal-to-noise ratio. An ineffective buffer results in high background noise, potentially drowning out the true signal. Different blockers have unique advantages and drawbacks; for instance, while Bovine Serum Albumin (BSA) is widely used, it can interfere with assays involving bovine antibodies. Selecting the right buffer is crucial for assay clarity and data reliability [62].
3. My biosensor results are inconsistent between runs. Could the immobilization method be a factor? Yes, the functionalization method significantly impacts both the signal strength and replicability of biosensors. Research shows that changing the immobilization chemistry and patterning approach can alter the detection signal by more than 8-fold and is critical for achieving a reliable inter-assay coefficient of variability (CV) [63]. Ensuring a consistent and optimized immobilization protocol is key to reproducible results.
4. Are there alternatives to traditional protein-based blocking buffers? Yes, several alternatives exist:
- Protein-based classics: BSA, Casein, Non-fat Dry Milk, and Fish Gelatin (which offers lower cross-reactivity with mammalian antibodies) [62].
- Synthetic blocking agents: These are engineered molecules that provide a defined composition and minimize the risk of interference common with biological mixtures [62].
- Proprietary buffers: Pre-optimized commercial solutions offer convenience and consistency, though they can be more costly [62].
Troubleshooting Common Experimental Issues
Problem: High background noise or false positive signals.
- Potential Cause: Inadequate blocking of the biosensor surface.
- Solution:
- Optimize your blocking buffer: Test different types (e.g., BSA vs. casein vs. synthetic) for your specific assay [62].
- Fine-tune blocking conditions: Systematically optimize the blocking time, concentration, pH, and ionic strength of the blocking solution. Under-blocking leaves sites open, while over-blocking can mask the target [62].
Problem: Low signal strength, even when the target is present.
- Potential Cause: The bioreceptors are not properly immobilized or are immobilized in an orientation that reduces binding efficiency.
- Solution:
- Evaluate immobilization chemistries: Compare different methods. For example, one study found that a simple polydopamine-mediated spotting method improved the detection signal for a spike protein by over 8 times compared to a flow-based method using the same chemistry [63].
- Verify bioreceptor activity: Ensure that the immobilization process does not denature the bioreceptors (e.g., antibodies, aptamers) and that their binding sites remain accessible.
Problem: Inconsistent results (high assay variability).
- Potential Cause: Inconsistent surface functionalization or the presence of bubbles in microfluidics-integrated systems.
- Solution:
- Standardize the functionalization protocol: Adopt a method that demonstrates low variability. The aforementioned polydopamine-spotting approach achieved an inter-assay CV below the 20% threshold for immunoassay validation [63].
- Mitigate bubbles in microfluidics: Implement strategies such as device degassing, plasma treatment, and pre-wetting microchannels with a surfactant solution to improve assay stability and yield [63].
Experimental Protocols & Data
Detailed Methodology: Comparing Bioreceptor Immobilization Approaches
A 2025 study provides a clear protocol for comparing functionalization methods to optimize performance [63]:
Biosensor Functionalization:
- Chemistry 1 (Polydopamine-mediated): Prepare a polydopamine solution in Tris-HCl buffer (pH 8.5). Introduce the solution to the biosensor surface and incubate to allow a thin film to form. Subsequently, spot or flow the bioreceptor (e.g., antibody, protein A) onto the activated surface.
- Chemistry 2 (Protein A-mediated): Immobilize Protein A on the sensor surface using a standard coupling chemistry like EDC/NHS. Then, flow the antibody over the Protein A surface, which facilitates a consistent, oriented binding.
Patterning Approach:
- Spotting-based: Use a non-contact dispenser to directly spot the bioreceptor solution onto defined locations on the biosensor chip.
- Flow-based: Use a microfluidic system to flow the bioreceptor solution over the entire functionalized channel.
Assay and Measurement:
- After functionalization, block the surface with an optimized blocking buffer.
- Introduce the target analyte (e.g., spike protein at 1 μg mL⁻¹).
- Measure the detection signal (e.g., wavelength shift for optical biosensors) and calculate the inter-assay coefficient of variability (CV) across multiple sensor chips.
Summary of Quantitative Performance Data [63]
Table 1: Impact of Functionalization Method on Biosensor Performance
| Immobilization Chemistry | Patterning Approach | Relative Signal Improvement | Inter-assay Variability (CV) |
|---|---|---|---|
| Polydopamine | Spotting | 8.2x (vs. Polydopamine/Flow) | < 20% |
| Polydopamine | Flow | Baseline (1x) | Not specified |
| Protein A | Flow | 1.4x (vs. Polydopamine/Flow) | Not specified |
Optimization of Blocking Buffer Conditions [62]
Table 2: Key Factors for Optimizing Blocking Buffer Performance
| Factor | Effect of Poor Optimization | Recommended Action |
|---|---|---|
| pH | Can alter charge and shape of proteins/blockers, reducing effectiveness. | Verify that the pH is optimal for your specific blocking agent and assay. |
| Ionic Strength | Too much or too little salt can disrupt charge-based blocking. | Find the "sweet spot" to prevent unwanted interactions without disrupting specific binding. |
| Blocking Time | Under-blocking leaves sites open; over-blocking can mask the target. | Run a time-course experiment to find the optimal duration. |
| Blocking Concentration | Too low is ineffective; too high can prevent target binding. | Create a titration curve to determine the ideal concentration. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Bioreceptor Immobilization and Blocking
| Reagent / Material | Function / Explanation |
|---|---|
| Bovine Serum Albumin (BSA) | A widely used, cost-effective protein for blocking non-specific binding sites. |
| Casein | A milk-derived protein offering a lower-cost alternative to BSA for blocking. |
| Fish Gelatin | A blocking agent that minimizes cross-reactivity with mammalian antibodies. |
| Synthetic Blocking Agents | Engineered molecules with a defined composition for highly controlled and reproducible blocking. |
| Polydopamine | A versatile polymer used for surface coating that facilitates strong bioreceptor immobilization. |
| Protein A | A bacterial protein that binds the Fc region of antibodies, promoting oriented immobilization. |
| Silver Nanoparticles (AgNPs) | Used in electrode modification to enhance conductivity and signal transduction [64]. |
| Poly(4-hydroxybenzoic acid) | A conductive polymer for electrode modification, providing a platform for biomolecule immobilization [64]. |
Experimental Workflow and Signaling Pathways
The following diagram illustrates the strategic decision-making pathway for selecting an optimization strategy, based on the primary assay problem encountered.
The following diagram outlines a general workflow for the initial setup and optimization of a biosensor surface, incorporating key steps from the referenced protocols.
Refining Sample Preparation Techniques to Mitigate Matrix Interferences
Troubleshooting Guide: Resolving Matrix Effects in Biosensor Assays
Matrix effects are a common source of false positives and false negatives in biosensor assays, caused by interfering components within complex biological samples. This guide provides targeted solutions for these critical issues.
Why does my biosensor show high background or false positives in clinical samples?
Problem: Non-specific binding or autofluorescence in complex matrices like serum or plasma increases background signal, leading to false positives [65] [66].
Solutions:
- Use Blocking Agents: Incorporate buffers containing proteins like Bovine Serum Albumin (BSA) or surfactants to minimize non-specific binding [66].
- Employ Sample Dilution: Diluting the sample with an assay-compatible buffer reduces the concentration of interfering substances [66].
- Implement Buffer Exchange: Use desalting columns to remove interfering components and place the sample into a compatible buffer [66].
- Apply Antifouling Coatings: For physical biosensors, use surface coatings designed to resist the adhesion of nonspecific biomolecules [67].
Why is my signal suppressed, leading to false negatives?
Problem: Enzymatic inhibitors or signal quenchers in the sample can suppress the assay signal [68] [65].
Solutions:
- Add Specific Enzyme Inhibitors: For cell-free biosensors, the addition of RNase inhibitors has been shown to mitigate degradation of nucleic acid components, though commercial glycerol-based buffers should be avoided [68] [69].
- Use Matrix-Matched Calibration: Prepare standard curves using the same biological matrix as the unknown samples to correct for suppression or enhancement effects [66].
- Optimize Sample Preparation: For sputum, a mild enzymatic liquefaction step can disrupt the matrix with fewer interferences than harsh chemicals [22].
How can I reduce high inter-patient variability in my results?
Problem: Differences in sample composition between individuals cause inconsistent biosensor performance [68].
Solutions:
- Standardize Sample Processing: Uniform collection and preparation methods are crucial. For blood, ensure consistent centrifugation protocols for serum and plasma separation [68] [69].
- Internal Standardization: Where possible, use a spiked internal standard to correct for recovery variations in each sample.
- Engineer Robust Biological Components: Utilizing engineered strains, such as E. coli producing endogenous RNase inhibitor, can temper interpatient variability by making the biosensor core more resilient [68].
Frequently Asked Questions (FAQs)
The common sources vary by sample type [68] [65] [66]:
- Serum/Plasma: Proteins, lipids, and bilirubin.
- Sputum: Highly cross-linked mucins creating a viscous, semi-solid matrix.
- Urine: Variable pH, salts, and metabolites.
- General: Endogenous enzymes like RNases or proteases, and sample contaminants.
What are the fundamental strategies for mitigating matrix effects?
The core strategies involve sample treatment, assay design, and validation [66]:
- Sample Preparation: Dilution, filtration, centrifugation, and buffer exchange.
- Assay Optimization: Using blocking agents, optimizing antibody specificity, and modifying incubation protocols.
- System Design: Employing dual-modality biosensors that use two detection methods for cross-validation [2].
- Validation: Performing spike-recovery experiments and parallel analysis to quantify and account for matrix effects.
How can I validate that my sample prep has successfully mitigated interference?
Robust validation is key to reliable results [65] [66]:
- Spike-Recovery Experiments: Spike a known amount of analyte into the sample matrix and measure the recovery percentage. Acceptable recovery (e.g., 80-120%) indicates minimal interference.
- Parallel Analysis: Compare results from a gold-standard reference method (like LC-MS or ELISA) with your biosensor results for a set of real samples.
- Standard Addition: For complex matrices, use the method of standard addition to quantify the analyte without a pre-defined matrix-matched standard.
Experimental Protocols & Data
Detailed Protocol: Mitigating RNase Interference in Cell-Free Biosensors
This protocol is adapted from systematic evaluations of cell-free systems in clinical samples [68] [69].
Principle: Clinical samples contain RNases that degrade RNA components in cell-free transcription-translation (TX-TL) systems, inhibiting reporter protein production. This protocol uses an engineered RNase inhibitor to protect the system.
Workflow:
Procedure:
- Sample Preparation: Collect clinical samples (serum, plasma, urine, saliva) using standard venipuncture or collection kits. For serum and plasma, perform basic centrifugation according to established protocols to remove cells or debris. Do not use additional processing unless experimentally required [68] [69].
- Reaction Setup:
- Use a cell-free TX-TL extract prepared from a specialized E. coli strain engineered to produce murine RNase inhibitor (mRI) [68]. This avoids the glycerol interference found in commercial inhibitors.
- In a reaction tube, mix the cell-free extract, an optimized energy buffer, salts, and a plasmid DNA constitutively expressing a reporter gene (e.g., sfGFP or luciferase).
- Add the clinical sample to a final concentration of 10% (v/v) of the total reaction volume [68] [69].
- Incubation and Detection:
- Incubate the reaction at a constant temperature (e.g., 37°C) for a set period (e.g., several hours).
- Measure reporter output fluorometrically (for sfGFP) or luminometrically (for luciferase).
Expected Outcome: The use of the mRI-producing extract should yield higher reporter protein levels and reduced inter-patient variability compared to using a standard extract or one supplemented with commercial RNase inhibitor [68].
Quantitative Data: Matrix Effects and Mitigation
The table below summarizes the inhibitory effects of different clinical samples on cell-free biosensors and the recovery achieved with mitigation strategies, based on published research [68] [69].
Table 1: Inhibition and Recovery in Cell-Free Biosensors
| Clinical Sample | Reporter | Inhibition (%) | Mitigation Strategy | Recovery Achieved |
|---|---|---|---|---|
| Serum | sfGFP | >98% | RNase Inhibitor | ~20% improvement |
| Luciferase | >98% | RNase Inhibitor | Up to 50% of no-sample signal | |
| Plasma | sfGFP | >98% | RNase Inhibitor | ~40% improvement |
| Luciferase | >98% | RNase Inhibitor | Up to 50% of no-sample signal | |
| Urine | sfGFP | >90% | RNase Inhibitor | ~70% improvement |
| Luciferase | >90% | RNase Inhibitor | Less effective than in other samples | |
| Saliva | sfGFP | ~40% | (None measured) | (Baseline) |
| Luciferase | ~70% | RNase Inhibitor | Up to 50% of no-sample signal |
The Scientist's Toolkit: Key Reagents for Mitigation
Table 2: Essential Reagents for Overcoming Matrix Interference
| Reagent / Material | Function in Mitigation | Example Application |
|---|---|---|
| RNase Inhibitor | Protects RNA from degradation in biological samples. | Critical for cell-free biosensor function in serum, plasma, and urine [68] [69]. |
| Bovine Serum Albumin (BSA) | Blocking agent that reduces non-specific binding by saturating surface sites. | Used in immunoassays and on sensor surfaces to lower background signal [66]. |
| Murine RNase Inhibitor (mRI) producing E. coli extract | Provides RNase inhibition without the glycerol found in commercial buffers, which itself can inhibit cell-free reactions [68]. | Engineered cell-free system for more robust performance in clinical samples [68]. |
| Poly(sodium 4-styrenesulfonate) (PSS) | Polymer used to functionalize paper for creating stable biosensor reservoirs. | Manufacturing of paper-based biosensors for pathogen detection [22]. |
| Gold Nanoparticles (AuNPs) | Serve as a colorimetric label or signal amplifier in optical biosensors. | Conjugated with antibodies for detection in competitive immunoassays on paper platforms [22]. |
Calibration and Signal Processing Adjustments to Enhance Signal-to-Noise Ratio
How do I calculate the Signal-to-Noise Ratio (SNR) for my biosensor, and what is considered a good value?
The Signal-to-Noise Ratio (SNR) is a quantitative measure critical for evaluating biosensor performance. A higher SNR indicates a greater ability to distinguish the target signal from background noise, leading to more accurate results and a lower likelihood of false positives or negatives [27].
For a straightforward DC (direct current) optical signal, SNR can be calculated using the ratio of the average signal amplitude to the standard deviation of the noise [27]. The formulas are:
- Linear Scale:
SNR = μ / σ- Where
μis the mean (average) of the signal, andσis the standard deviation of the noise.
- Where
- Logarithmic Scale (decibels):
SNR (dB) = 20 * log10( μ / σ )
For more complex signals, such as a photoplethysmography (PPG) signal which contains both AC and DC components, a different approach is needed. In this case, signal processing in the frequency domain is recommended. The signal is filtered to separate the biologically relevant frequencies (e.g., below 20 Hz for PPG) from the higher-frequency noise, allowing for a more accurate SNR calculation [27].
What constitutes a "good" SNR is highly dependent on the specific biosensor platform, its intended application, and the required detection limit. The primary goal is to have an SNR high enough to ensure your target analyte's signal is unmistakably distinguishable from system noise. The table below summarizes the calculation methods.
Table: Methods for Calculating Signal-to-Noise Ratio
| Signal Type | Calculation Method | Key Consideration |
|---|---|---|
| DC / Simple Optical | SNR = μ / σ [27] |
Requires a stable baseline and consistent signal. |
| AC + DC Composite (e.g., PPG) | Frequency-domain filtering to separate signal and noise bands [27] | Prevents false noise results from the signal's natural variation. |
What are the most effective strategies to improve the SNR in my biosensor assays?
Enhancing SNR is a two-pronged approach: amplifying the specific signal and suppressing the background noise. The following diagram illustrates the logical workflow for tackling SNR improvement.
A. Signal Enhancement Strategies
- Optimize the Biorecognition Event: The efficiency of the interaction between your bioreceptor (e.g., antibody, aptamer) and the target analyte is fundamental. You can enhance this by regulating binding kinetics and increasing the probability of reaction through careful design of the surface chemistry and fluidics [70].
- Employ Signal Amplification Techniques: These are designed to make the detection event more pronounced.
- Assembly-based amplification: Using structures like gold nanoparticles that can form larger aggregates, creating a stronger signal per binding event [70].
- Metal-Enhanced Fluorescence (MEF): Utilizing metallic nanostructures to amplify the fluorescence signal of nearby labels, significantly boosting intensity [70].
- Utilize Advanced Detection Modalities: Switching from a standard continuous-wave excitation to a time-gated detection method (e.g., using lanthanide probes) can effectively separate the long-lived signal from short-lived background fluorescence [70].
B. Background Noise Reduction Strategies
- Suppress Optical Background:
- Time-gated noise suppression: As mentioned above, this technique temporally separates the signal from the noise [70].
- Wavelength-selective noise reduction: Using optical filters to block scattered excitation light and only collect the emission light from the label [70].
- Low-excitation background strategies: Employing detection modes like chemiluminescence that do not require an external light source, thereby eliminating noise from source scattering and ambient light [70].
- Improve Surface Chemistry and Materials:
- Anti-fouling Coatings: Apply coatings like polyethylene glycol (PEG) or bovine serum albumin (BSA)-based composites to the sensor surface to prevent non-specific adsorption of proteins or other molecules from complex samples (e.g., blood, saliva). This directly reduces biological noise [71].
- Novel Carbon Nanomaterials: Materials like graphene and other advanced carbon allotropes offer high conductivity (reducing electronic noise) and can have innate anti-fouling properties, tackling both electronic and biological noise sources simultaneously [71].
- Optimize Electronic Systems: Ensure proper electromagnetic shielding of the instrument and use a stable power supply to minimize noise from external sources like power lines or radio frequencies [71].
My biosensor data is unstable and drifts over time. How can calibration and processing fix this?
Baseline drift and signal instability are often related to environmental factors, sensor degradation, or nonspecific binding. Calibration and signal processing are essential to correct these issues.
- Implement Robust Calibration Protocols:
- Frequent Recalibration: Regularly calibrate your sensor using standard solutions with known analyte concentrations to establish a fresh calibration curve. This accounts for the degradation of biological components over time [67].
- Use Reference Standards: Incorporate internal references or control samples in each run. For example, using a sensor channel with an inert bioreceptor can provide a baseline to subtract for drift and nonspecific binding [72].
- Apply Signal Processing Algorithms:
- Baseline Correction: Algorithms can be used to model and subtract a drifting baseline from the raw signal, leaving behind the analyte-specific response.
- Digital Filtering: Use high-pass filters to remove low-frequency drift or low-pass filters to remove high-frequency noise. For signals like PPG, band-pass filters are used to isolate the physiologically relevant frequency components [27].
- Multivariate Calibration: For complex data, techniques like Principal Component Analysis (PCA) or Partial Least Squares (PLS) regression can be employed to resolve overlapping signals and compensate for drift and matrix effects [67].
Can you provide a detailed protocol for optimizing an SPR biosensor to minimize false positives?
False positives in Surface Plasmon Resonance (SPR) often stem from nonspecific binding and inadequate surface preparation. The following workflow provides a step-by-step guide for optimization.
Protocol: Minimizing False Positives in SPR Biosensing [72] [73]
Objective: To establish a robust SPR assay with high specificity and minimal false positive signals.
Materials:
- SPR instrument (e.g., Biacore series)
- Appropriate sensor chips (e.g., CM5, NTA, SA)
- Purified ligand and analyte samples
- Running buffer (e.g., HBS-EP: 10 mM HEPES, 150 mM NaCl, 3 mM EDTA, 0.05% v/v Surfactant P20, pH 7.4)
- Regeneration solution (e.g., 10 mM Glycine-HCl, pH 2.0-3.0)
- Blocking agent (e.g., 1 M Ethanolamine, pH 8.5, or 1% BSA)
Procedure:
Pre-Experimental Setup:
- Chip Selection: Choose a sensor chip with chemistry compatible with your ligand. For antibodies, CM5 (carboxymethylated dextran) is common. For his-tagged proteins, NTA chips are ideal [72].
- Buffer Optimization: Prepare a running buffer containing a surfactant like Tween-20 or the included P20 to reduce nonspecific binding. Ensure the buffer's pH and ionic strength maintain the stability of your interactions [72].
- Sample Quality Control: Purify your ligand and analyte samples to remove aggregates and contaminants. Characterization via methods like SDS-PAGE or HPLC is recommended to ensure homogeneity [72].
Surface Preparation and Immobilization:
- Ligand Immobilization: Immobilize your ligand using standard amine-coupling (EDC/NHS) or capture methods. Crucially, optimize the immobilization level. A density that is too high can cause steric hindrance and rebinding effects, while too low a density yields a weak signal. Aim for an Rmax that fits your kinetic model [72].
- Surface Blocking: After immobilization, deactivate any remaining active esters on the surface with an injection of ethanolamine. Furthermore, inject a blocking agent like BSA or casein to passivate any nonspecific sites on the chip surface [72].
- Reference Surface: Create a reference flow cell by subjecting a blank channel to the same immobilization and blocking procedure but without the ligand. This channel will be used for automatic subtraction of bulk refractive index changes and nonspecific binding.
Assay Execution and Validation:
- Control Analytes: Always run control experiments with analytes known not to bind your ligand. This confirms that your blocking and buffer conditions are effective and provides a direct measure of nonspecific binding [72].
- Optimize Flow Rate: Use a moderate to high flow rate (e.g., 30-50 µL/min) to minimize mass transport limitations and reduce the time for nonspecific interactions to occur [72].
- Secondary Validation: For primary screening, consider developing a secondary, orthogonal assay to validate hits. For example, a sequential competition assay can efficiently reveal false positives by probing the remaining binding sites with a high-molecular-weight reporter ligand [73].
Research Reagent Solutions for SNR Enhancement
The table below lists key materials and reagents commonly used to implement the SNR enhancement strategies discussed.
Table: Essential Research Reagents for Biosensor Optimization
| Reagent / Material | Function in SNR Enhancement | Key References / Examples |
|---|---|---|
| CM5 Sensor Chip | A carboxymethylated dextran chip for covalent immobilization of proteins (e.g., antibodies) via amine coupling. | [72] |
| NTA Sensor Chip | For capturing His-tagged proteins, allowing for controlled orientation and reversible binding. | [72] |
| Surfactant P20 (Tween-20) | A non-ionic detergent added to running buffers to reduce nonspecific binding to the sensor surface. | [72] |
| BSA or Ethanolamine | Used as blocking agents to passivate unused active sites on the sensor surface after ligand immobilization. | [72] |
| Gold Nanoparticles (AuNPs) | Used in signal amplification strategies, such as assembly-based amplification, to enhance optical or electrochemical signals. | [70] [74] |
| Polyethylene Glycol (PEG) | A polymer used to create anti-fouling coatings on sensor surfaces, reducing noise from nonspecific adsorption. | [71] |
| Novel Carbon Nanomaterials | Materials like graphene or Gii provide high conductivity (low electronic noise) and innate anti-fouling properties. | [71] |
| Time-gated Lanthanide Probes | Fluorescent probes with long lifetimes, enabling time-gated detection to suppress short-lived background fluorescence. | [70] |
Frequently Asked Questions (FAQs)
Q: What is the trade-off between SNR and power consumption in optical biosensors? A: In optical systems like wearable biosensors, increasing LED current or duty cycle boosts light output and SNR but also significantly increases power consumption, which shortens battery life. The optimal configuration balances sufficient SNR for accurate readings with acceptable power drain for the application [27].
Q: How can artificial intelligence (AI) improve the SNR and reduce false results? A: AI and machine learning (ML) algorithms can process complex biosensor data to intelligently distinguish true signals from noise patterns. They can enhance sensitivity and specificity through advanced signal processing, pattern recognition, and automated decision-making, thereby helping to mitigate false positives and negatives [1] [75].
Q: My lateral flow immunoassay (LFIA) lacks sensitivity. What are the best SNR strategies for this platform? A: LFIA can be enhanced through multiple approaches. For signal amplification, consider using gold nanostructures or fluorescent labels with metal-enhanced fluorescence (MEF). For noise reduction, strategies like time-gated luminescence (to eliminate background from the strip material) or switching to a chemiluminescence-based detection (which has a low-excitation background) are highly effective [70].
Evaluating Assay Performance and Comparative Efficacy of Solutions
Core Concepts FAQ
What are sensitivity and specificity, and why are they critical for diagnosing biosensor performance?
Sensitivity and specificity are fundamental, prevalence-independent metrics that describe the accuracy of a diagnostic test, such as a biosensor assay [76] [77].
- Sensitivity (True Positive Rate): This measures the test's ability to correctly identify individuals who have the condition. It is the proportion of actual positives that are correctly identified [76] [77]. A high-sensitivity test is crucial for "ruling out" a disease because it misses very few true positives [77].
- Specificity (True Negative Rate): This measures the test's ability to correctly identify individuals who do not have the condition. It is the proportion of actual negatives that are correctly identified [76] [77]. A high-specificity test is essential for "ruling in" a disease because it minimizes false alarms [77].
Table 1: The Confusion Matrix - Defining Test Outcomes
| Condition Present (Truth) | Condition Absent (Truth) | |
|---|---|---|
| Test Positive | True Positive (TP) | False Positive (FP) |
| Test Negative | False Negative (FN) | True Negative (TN) |
The formulas for calculating these metrics are [76] [77]:
- Sensitivity = TP / (TP + FN)
- Specificity = TN / (TN + FP)
How do Precision, Recall, and the F1-Score relate to Sensitivity and Specificity?
Precision and Recall are another pair of metrics, particularly useful when evaluating classification tools on imbalanced datasets, which are common in bioinformatics [78].
- Precision (Positive Predictive Value): Answers the question: "Of all the positive results my biosensor reported, how many were actually positive?" It is calculated as TP / (TP + FP) [78]. A high precision indicates low false positive rates.
- Recall: This is mathematically identical to Sensitivity (TP / (TP + FN)) [78]. It answers: "Of all the actual positive samples, how many did my biosensor successfully find?"
The F1-Score is the harmonic mean of Precision and Recall, providing a single metric that balances the concern for both false positives and false negatives. It is especially valuable when you need to find an optimal balance between the two [78].
What is the inherent trade-off between sensitivity and specificity in biosensor assays?
There is a fundamental trade-off: as sensitivity increases, specificity tends to decrease, and vice versa [76] [79]. This occurs because a biosensor's performance is ultimately limited by the accuracy of the underlying biological affinity interaction (e.g., an antibody binding to its target) [79]. This trade-off is often managed by adjusting the test's cut-off point or decision threshold. A lower threshold might catch more true positives (increasing sensitivity) but also admit more false positives (decreasing specificity) [77].
Troubleshooting Guide: Diagnosing False Positives
Table 2: Troubleshooting Common Causes of False Positives in Biosensor Assays
| Symptom | Potential Cause | Investigation & Resolution |
|---|---|---|
| High false positive rate, negative controls also show positive signal. | Sample or reagent contamination during assay setup [80]. | Physically separate pre-PCR and post-PCR areas. Decontaminate work surfaces and pipettes with a 10% bleach solution. Always use fresh pipette tips and thoroughly mix all reagents [80]. |
| Increasing baseline fluorescence or baseline drift over time. | Probe degradation due to DNase contamination or reducing agents (e.g., DTT) in the reaction mix [80]. | Use fresh, high-quality reagents. Avoid carrying over DTT from reverse transcription steps, as it can degrade common quencher dyes like BHQ [80]. |
| False positives occur at high concentrations of variant (non-target) analyte. | Limited inherent specificity of the biorecognition element; the probe binds to non-targets at high concentrations [79]. | Consider advanced probe technologies like Tentacle Probes (TPs), which use cooperative binding to provide concentration-independent specificity and can eliminate false positives even at high variant concentrations [79]. |
| Jagged amplification signals and elevated background noise. | Poor probe signaling, potentially from inefficient quenching, low probe Tm, or suboptimal fluorophore selection [80]. | Check probe concentration and design. Ensure the melting temperature (Tm) is appropriate and that the distance between the fluorophore and quencher is not too great. Verify instrument calibration for the chosen dye [80]. |
| Positive results in a well-characterized negative sample. | Incorrect threshold setting in qPCR data analysis, placing the threshold within the background noise [80]. | Manually set the threshold above the background baseline and within the exponential phase of amplification. Do not rely solely on software-automated settings [80]. |
Experimental Protocols for Benchmarking
Protocol: Determining Sensitivity and Specificity Using a Truth Set
This protocol allows you to empirically determine the key accuracy metrics for your biosensor assay [78].
- Establish a Truth Set: Obtain or create a collection of samples where the true status (positive or negative for the analyte) is definitively known. This serves as your gold standard for comparison [78].
- Run the Assay: Process all samples from the truth set using your biosensor under standardized conditions.
- Tally Results: Compare your biosensor's results against the known truth and populate a confusion matrix (as shown in Table 1). Count the True Positives (TP), False Positives (FP), True Negatives (TN), and False Negatives (FN).
- Calculate Metrics:
- Calculate Sensitivity: TP / (TP + FN)
- Calculate Specificity: TN / (TN + FP)
- Calculate Precision: TP / (TP + FP)
- Calculate F1-Score: 2 * ((Precision * Recall) / (Precision + Recall))
Protocol: Evaluating Tentacle Probes for Enhanced Specificity
This methodology, based on published research, describes how to test a probe system designed to overcome the sensitivity-specificity trade-off [79].
- Probe and Target Synthesis: Synthesize Tentacle Probes (TPs) and traditional Molecular Beacons (MBs) with identical detection sequences and varying stem lengths. Synthesize target sequences, including the perfect match (wild-type), and variants with single nucleotide polymorphisms (SNPs) in different regions [79].
- Kinetic Measurements:
- Prepare solutions of each probe (e.g., 100 nM).
- Rapidly add an excess of the target analyte (e.g., 1 μM for TPs, 10 μM for MBs) to initiate the reaction.
- Immediately monitor fluorescence intensity over time (e.g., 10 minutes for TPs, 1 hour for MBs) using a plate reader [79].
- Plot fluorescence against time and fit the data to determine the reaction rate constants.
- Specificity Assessment:
- Test each probe against all target types (wild-type and SNP variants) across a wide concentration range (e.g., up to 1 mM).
- Record the fluorescence signal for each combination. Tentacle Probes are characterized by maintaining a high signal with the wild-type target and showing no false positive signal (similar to background) even at very high concentrations of SNP variants, whereas Molecular Beacons may show significant false positives at lower variant concentrations [79].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Their Functions in Biosensor Development
| Reagent / Material | Function in Biosensor Development & Troubleshooting |
|---|---|
| Tentacle Probes (TPs) | A class of reagents that use cooperative binding to enhance specificity and kinetics simultaneously, reducing false positives without sacrificing sensitivity [79]. |
| Molecular Beacons (MBs) | Hairpin-shaped nucleic acid probes with a fluorophore and quencher. The stem-loop structure provides inherent specificity, but they can suffer from false positives at high concentrations of non-target analytes [79]. |
| Carrier Nucleic Acids (e.g., yeast tRNA, PolyA) | Added to dilute DNA solutions to prevent adsorption of low-concentration target molecules to tube walls, thereby avoiding "drop-out" effects and false negatives [80]. |
| Black Hole Quencher (BHQ) Dyes | Common dark quenchers used in fluorescent probes. They contain an azo bond that can be reduced by agents like DTT, leading to loss of quenching and baseline drift [80]. |
| Fluorophore-Quencher Pairs | The core signaling system of many optical biosensors. The choice of pair (e.g., FAM-BHQ) affects signal strength, background noise, and instrument detection efficiency [80]. |
Diagnostic Logic and Experimental Workflow Visualization
The following diagrams outline the logical process for diagnosing false positives and the experimental workflow for benchmarking a biosensor.
Biosensor False Positive Diagnosis
Biosensor Benchmarking Workflow
Comparative Analysis of Single-Mode vs. Dual-Mode Biosensing Platforms
Biosensors are analytical devices that combine a biological recognition element with a physicochemical transducer to detect a specific analyte. They are vital tools in clinical diagnostics, food safety, and environmental monitoring, converting biochemical reactions into measurable signals [1]. The core components of any biosensor include the analyte (substance to be detected), bioreceptor (molecule that specifically recognizes the analyte), transducer (converts recognition event into measurable signal), electronics (processes the signal), and display (presents the results) [1].
Single-mode biosensors utilize one transduction mechanism (e.g., optical or electrochemical) for detection, while dual-mode biosensors integrate two complementary detection techniques in a single platform to enhance reliability and accuracy [2]. This technical resource center provides troubleshooting guidance for researchers investigating false positives in biosensor assays, with particular focus on the comparative advantages of dual-mode systems for error reduction.
Technical Comparison: Single-Mode vs. Dual-Mode Biosensors
Performance Characteristics
Table 1: Comparative performance metrics of single-mode and dual-mode biosensing platforms
| Parameter | Single-Mode Biosensors | Dual-Mode Biosensors | Experimental Validation |
|---|---|---|---|
| False Positive/Negative Rates | Higher susceptibility due to single signal pathway [2] | Significantly reduced through cross-validation [2] [81] | Internal cross-validation between two independent signals [2] |
| Detection Limit | Varies with modality: Optical: ~1.1 particles/μL [82] | Enhanced sensitivity: Electrochemical: 9 CFU/mL for live bacteria [83] | Serial dilution studies with spiked samples [83] |
| Dynamic Range | Constrained by single detection mechanism [2] | Broader due to complementary detection ranges [81] | Analysis across concentration gradients (e.g., 10-10⁶ particles/μL) [82] |
| Matrix Effect Resistance | Susceptible to interference in complex samples [2] | Improved resilience through signal cross-correlation [2] | Testing in clinical samples (serum, blood) [82] |
| Reliability & Accuracy | Limited by environmental variability and signal noise [2] | Enhanced through self-correction capabilities [2] [81] | Statistical comparison with reference methods (e.g., PCR, ELISA) [83] |
Operational Characteristics
Table 2: Operational comparison between biosensing platforms
| Characteristic | Single-Mode Biosensors | Dual-Mode Biosensors | Troubleshooting Implications |
|---|---|---|---|
| Signal Transduction Pathways | Single pathway (optical, electrochemical, or mechanical) [2] | Two independent pathways (e.g., optical-electrochemical) [2] | Failure in one pathway doesn't compromise entire assay |
| System Complexity | Simplified design and fabrication [2] | Increased complexity due to integrated systems [2] | Requires expertise in multiple detection methodologies |
| Calibration Requirements | Standard single-point calibration | Multi-parameter calibration needed [81] | More comprehensive but time-consuming calibration protocol |
| Data Interpretation | Straightforward single-signal analysis | Complex multivariate analysis [81] | Discrepancies between signals require investigation |
| Cost Considerations | Generally lower per-device cost | Higher initial development cost [2] | Balanced by reduced repeat testing needs |
Fundamental Principles and Signaling Pathways
Single-Mode Biosensing Mechanisms
Single-mode biosensors operate through one primary transduction mechanism. The major categories include:
Optical Biosensors: Measure changes in light properties (absorbance, fluorescence, scattering) resulting from analyte-bioreceptor interactions [2]. These include colorimetric, fluorometric, surface plasmon resonance (SPR), and surface-enhanced Raman scattering (SERS) systems.
Electrochemical Biosensors: Convert biochemical reactions into measurable electrical signals (current, potential, impedance) [2]. These include amperometric, potentiometric, and impedance-based systems.
Mechanical Biosensors: Detect changes in mass, density, or viscoelastic properties, often using cantilever or acoustic wave technologies.
Single-Mode Biosensor Signal Pathway: This diagram illustrates the linear signal pathway in single-mode biosensors, highlighting vulnerability points to environmental interference that can lead to false results.
Dual-Mode Biosensing Mechanisms
Dual-mode biosensors integrate two independent transduction mechanisms to provide complementary detection capabilities:
Cross-Validation Capability: Dual-mode systems enable real-time validation of results through two independent signal pathways, significantly reducing false positives and negatives [2].
Complementary Detection Ranges: Different modalities often cover various concentration ranges, expanding the dynamic detection range [81].
Redundancy: If one detection method experiences interference, the secondary method can still provide reliable data [2].
Common dual-mode combinations include:
- Optical-electrochemical (e.g., fluorescence-amperometric)
- Electrochemical-photothermal
- Colorimetric-fluorescence [82]
- Bioluminescence-fluorescence [83]
Dual-Mode Biosensor Signal Pathway: This diagram shows the parallel signal pathways in dual-mode biosensors, demonstrating how cross-validation and signal compensation reduce susceptibility to interference.
Experimental Protocols for False Positive Investigation
Protocol: Dual-Mode Biosensor Assembly and Validation
Objective: Construct and validate a dual-mode biosensor with cross-validation capability to minimize false positives in complex samples.
Materials:
- Functionalized transducer substrates (e.g., Au electrodes, glass chips)
- Biorecognition elements (antibodies, aptamers, enzymes)
- Signal probes (enzyme conjugates, fluorescent dyes, nanoparticles)
- Target analytes and interfering substances
- Buffer solutions and blocking agents
Methodology:
- Substrate Functionalization:
- Clean transducer surfaces according to manufacturer protocols
- Immobilize biorecognition elements using appropriate chemistry (e.g., EDC-NHS for antibodies, thiolation for aptamers)
- Block non-specific binding sites with BSA or casein
- Validate surface functionalization using surface characterization techniques (e.g., SPR, EIS)
Dual-Signal System Integration:
- Incorporate two independent detection systems (e.g., electrochemical and optical)
- Optimize assay conditions to ensure both systems function simultaneously without interference
- Establish signal calibration curves for both detection modalities
Cross-Validation Protocol:
- Test samples with known concentrations to establish correlation between signals
- Implement statistical algorithms for signal discrepancy analysis
- Set tolerance thresholds for acceptable signal variation
Troubleshooting Tips:
- If signal discrepancy exceeds thresholds, check bioreceptor integrity and storage conditions
- If both signals show consistent deviation, investigate sample matrix effects
- If one signal is consistently unreliable, optimize detection conditions for that modality
Protocol: Specificity Testing for False Positive Reduction
Objective: Systematically evaluate and minimize cross-reactivity in biosensor assays.
Materials:
- Primary target analyte
- Structurally similar interferents
- Biological matrices (serum, urine, saliva)
- Negative control samples
Methodology:
- Cross-Reactivity Assessment:
- Test biosensor response against structurally similar compounds
- Evaluate response against common biological matrix components
- Assess potential interferents at physiologically relevant concentrations
Matrix Effect Evaluation:
- Compare calibration curves in buffer vs. biological matrices
- Perform standard addition experiments to quantify matrix effects
- Implement matrix-matched standards when significant effects are observed
Dual-Mode Specificity Enhancement:
- Utilize the two detection modalities to confirm analyte identity
- Establish modality-specific response patterns for target vs. interferents
- Implement pattern recognition algorithms for enhanced specificity
Troubleshooting Tips:
- If cross-reactivity is observed, consider alternative biorecognition elements with higher specificity
- If matrix effects are significant, implement additional sample cleanup or dilution protocols
- If specificity patterns differ between modalities, optimize assay conditions for consistency
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Why does my biosensor produce false positives in complex biological samples?
A: False positives in complex matrices typically result from:
- Non-specific binding: Interfering substances in the sample bind to the biorecognition element or transducer surface [1]
- Matrix effects: Sample components alter the physicochemical environment, affecting assay performance [18]
- Cross-reactivity: Structurally similar compounds are recognized by the bioreceptor [1]
- Signal interference: Autofluorescence or electrochemical activity in the sample contributes to the signal [2]
Mitigation strategies:
- Incorporate more specific biorecognition elements (e.g., aptamers instead of antibodies)
- Implement additional blocking steps and wash protocols
- Use dual-mode detection to cross-validate results [2]
- Employ sample pretreatment to remove interferents
Q2: How can I determine whether a false positive is due to biorecognition or transducer issues?
A: Systematic troubleshooting:
- Test the biosensor with the target analyte in simple buffer - if false positives persist, the issue is likely transducer-related
- Perform competitive inhibition assays - if known interferents don't compete with the target, the issue is likely transducer-based
- Compare signals from both modalities in a dual-mode system - discrepant signals suggest modality-specific interference [2]
- Characterize the sensor surface after assay completion to detect non-specific adsorption
Q3: What are the key advantages of dual-mode over single-mode biosensors for false positive reduction?
A: Dual-mode biosensors provide:
- Internal validation: Two independent signals must agree for a positive result [2]
- Complementary information: Different modalities can distinguish between specific and non-specific binding [81]
- Error detection: Discrepancies between signals alert to potential interference [2]
- Wider dynamic range: Different modalities often cover complementary concentration ranges [81]
- Robustness: Failure or interference in one modality doesn't necessarily compromise the entire assay [2]
Q4: How can I optimize my dual-mode biosensor when the two signals show poor correlation?
A: Signal discrepancy indicates need for optimization:
- Temporal factors: Ensure both detection methods interrogate the same binding events simultaneously
- Spatial factors: Verify that both modalities probe the same region of the sensor
- Bioreceptor orientation: Optimize immobilization to ensure equal accessibility for both detection systems
- Signal-to-noise ratios: Independently optimize each detection modality before integration
- Calibration consistency: Use the same standard samples for both calibration curves
Troubleshooting Common Experimental Issues
Table 3: Troubleshooting guide for common biosensor false positive issues
| Problem | Possible Causes | Solutions | Preventive Measures |
|---|---|---|---|
| Consistent false positives across samples | Non-specific binding, bioreceptor degradation, insufficient blocking | Implement additional blocking steps, use fresh bioreceptors, increase wash stringency | Regular quality control of bioreceptors, optimize blocking protocol |
| Matrix-dependent false positives | Interfering substances in complex samples, pH/ionic strength effects | Dilute samples, implement cleanup steps, use matrix-matched standards | Characterize matrix effects during assay development |
| Inconsistent false positives | Variable environmental conditions, unstable signal transduction | Control temperature/humidity, implement internal reference standards | Environmental monitoring, signal normalization protocols |
| Modality-specific false positives (dual-mode) | Interference with specific detection method, optimization imbalance | Re-optimize affected modality, implement interference-resistant detection | Comprehensive interference testing during development |
| Concentration-dependent false positives | Sensor saturation, hook effect, non-linear response | Test wider concentration range, implement dilution protocols | Establish dynamic range during validation |
Research Reagent Solutions
Table 4: Essential research reagents for biosensor false positive investigations
| Reagent Category | Specific Examples | Function in False Positive Reduction | Application Notes |
|---|---|---|---|
| Blocking Agents | BSA, casein, salmon sperm DNA, commercial blocking buffers | Reduce non-specific binding to sensor surface | Must be compatible with detection modalities; test multiple agents |
| Surface Chemistry Reagents | EDC/NHS, MPA, APTES, glutaraldehyde | Controlled immobilization of biorecognition elements | Optimization required for each sensor surface type |
| Biorecognition Elements | Monoclonal antibodies, aptamers, molecularly imprinted polymers | Specific target recognition with minimal cross-reactivity | Aptamers offer advantages for stability and modification |
| Signal Probes | Enzyme conjugates, fluorescent dyes, quantum dots, electroactive tags | Generate detectable signal from binding events | Must be stable and produce minimal background signal |
| Wash Buffers | PBS with Tween-20, stringent wash buffers | Remove unbound material and weakly adsorbed interferents | Stringency must be optimized to preserve specific binding |
| Reference Materials | Certified reference materials, internal standards | Quality control and signal normalization | Essential for method validation and troubleshooting |
Advanced Methodologies: Triple-Mode Biosensing
Emerging research demonstrates that triple-mode biosensors further enhance reliability by integrating three distinct detection mechanisms. These systems provide even greater accuracy through additional cross-validation channels and can overcome limitations of dual-mode systems in ultra-trace detection and complex matrices [81].
Common triple-mode combinations include:
- Colorimetric-fluorescence-photothermal [81]
- Electrochemical-SERS-photothermal [81]
- Electrochemical-fluorescence-colorimetric [81]
The integration of artificial intelligence with multi-modal biosensing enables sophisticated error correction, pattern recognition, and predictive analytics, representing the future direction for reliable biosensing platforms [1] [81].
Dual-mode biosensing platforms offer significant advantages over single-mode systems for reducing false positives in complex analytical environments. Through cross-validation, complementary detection capabilities, and built-in redundancy, these systems provide the reliability required for critical applications in clinical diagnostics, food safety, and environmental monitoring. The troubleshooting guidelines and experimental protocols presented here provide researchers with practical strategies for investigating and resolving false positive issues in biosensor assays, with dual-mode systems representing a powerful approach for enhancing assay reliability.
FAQs on Biosensor Clinical Validation
What are the most critical factors to control when transitioning from spiked buffers to real patient samples? The most critical factors are matrix effects and nonspecific binding. Real patient samples like sputum, serum, or whole blood contain highly cross-linked mucins, thousands of proteins, and other components that can interfere with detection by increasing background noise or sequestering the target analyte [84] [85]. To control this, implement sample pre-processing steps (like enzymatic liquefaction for sputum) [84] and use sensor surfaces engineered for low nonspecific binding, such as linear polycarboxylate hydrogels [86].
Why does my assay show good sensitivity in buffer but high false positives in clinical samples? High false positives in clinical samples are frequently caused by nonspecific interactions between matrix components and the sensor surface [1] [86]. Complex samples can cause cross-reactivity with assay components. Using a competitive immunoassay format can sometimes circumvent these issues, as demonstrated in a paper biosensor for sputum pyocyanin detection, which showed clearer differentiation between spiked and non-spiked samples compared to traditional ELISA [84].
How can I validate the activity and quality of my immobilized ligand or bioreceptor? Ligand activity can be checked by injecting a high concentration of analyte (approximately 10-times the estimated KD value) and observing the binding response at saturation. The ratio of the molecular weight to the bound response units provides a good indication of ligand activity [86]. Ensure immobilization buffers are free of impurities and have the correct pH and salt concentrations to maintain ligand function [86].
Can very weak interactions be reliably measured in complex matrices? Yes, even weak interactions can be measured by combining highly sensitive instrumentation with high ligand-capacity surfaces. This powerful combination allows for the measurement of binding events with fast on- and off-rates, even in complex mixtures [86].
What are the benefits of a modular biosensor system for method development? A modular system provides significant flexibility. It allows for easy upgrades and maintenance, and the use of standardised components (like HPLC vials and FPLC fittings) reduces reliance on proprietary consumables, saving time and money [86].
Experimental Protocols for Validation
Protocol 1: Paper-Based Biosensor for Complex Sputum Samples
This protocol details a method to overcome matrix effects in sputum for detecting Pseudomonas aeruginosa via the biomarker pyocyanin (PYO) [84].
1. Sample Preparation (Liquefaction):
- Add hydrogen peroxide to the sputum sample for 1 minute. The production of bubbles mechanically disrupts the highly cross-linked mucin matrix, liquefying the sample without harsh chemicals or instrumentation [84].
2. Biosensor Assembly and Detection:
- The biosensor consists of two main parts: a paper substrate modified with an albumin-antigen conjugate (competing element) and a reservoir containing antibody-coated gold nanoparticles (Ab-AuNPs) [84].
- Add the liquefied sample to the paper substrate.
- Press the Ab-AuNPs reservoir against the substrate and incubate for 5 minutes. During this step, PYO from the sample and the paper-bound antigen compete for binding sites on the Ab-AuNPs.
- Wash the substrate. The intensity of the remaining colored spot is inversely proportional to the PYO concentration in the sample [84].
3. Analysis:
- Quantify the pixel intensity of the colorimetric signal. This paper biosensor demonstrated a lower relative standard deviation in sputum samples compared to ELISA [84].
Protocol 2: Assessing Ligand Immobilization Quality in SPR Biosensors
This protocol outlines key checks for successful ligand immobilization, a common failure point in biosensor experiments [86].
1. Ligand Purity and Buffer Check:
- Prior to immobilization, ensure the ligand is pure and active.
- Verify that the immobilization buffer is free of impurities and does not contain interfering substances like free amines. Confirm that pH and salt concentrations are optimal for your specific ligand [86].
2. Ligand Activity Test:
- Once immobilized, inject a known analyte at a high concentration (around 10 times the estimated KD).
- Allow binding to reach saturation. The ratio of the analyte's molecular weight to the immobilized response units (µRIU) provides an overview of ligand activity on the surface [86].
The table below summarizes performance characteristics from cited research, highlighting the transition from ideal to complex matrices.
Table 1: Comparison of Biosensor Performance in Validation Studies
| Biosensor Type / Target | Sample Matrix | Limit of Detection (LOD) | Key Validation Finding |
|---|---|---|---|
| Paper Immunosensor / Pyocyanin [84] | Buffer & Sputum | 4.7·10⁻³ µM | Qualitative differentiation in sputum superior to ELISA; reduced matrix effects. |
| SERS Platform / α-Fetoprotein (AFP) [5] | Aqueous solution | 16.73 ng/mL | Detected AFP across 500–0 ng/mL range; method avoids dependence on Raman reporters. |
| THz SPR Biosensor (Theoretical) [5] | Liquid & Gas | N/A | Achieved high phase sensitivity up to 3.1x10⁵ deg/RIU in simulation. |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Biosensor Development and Validation
| Reagent / Material | Function in Experiment | Example Use Case |
|---|---|---|
| Gold Nanoparticles (AuNPs) | Signal generation or transducer element; can be conjugated to antibodies [84]. | Used as colored labels in a paper-based competitive immunoassay [84]. |
| Poly(sodium 4-styrenesulfonate) (PSS) | Polymer used to create a charged reservoir for nanoparticle storage in paper biosensors [84]. | Prepares the Ab-AuNPs reservoir in the paper biosensor platform [84]. |
| PC1-BSA Bioconjugate | A competing antigen immobilized on the sensor surface in a competitive immunoassay [84]. | Serves as the competing recognition element for pyocyanin detection [84]. |
| Hydrogen Peroxide | A reagent used for the rapid, enzymatic liquefaction of complex, viscous samples [84]. | Disrupts sputum matrix through bubble production in a one-step, instrument-free process [84]. |
| Linear Polycarboxylate Hydrogels | Sensor chip coating material designed to minimize nonspecific binding and improve signal-to-noise ratio [86]. | Used in SPR biosensors to reduce false positives from complex samples like serum [86]. |
Experimental Workflow Diagrams
Diagram 1: Clinical validation workflow.
Diagram 2: Paper biosensor assay flow.
Assessing the Impact of Machine Learning Integration on Diagnostic Accuracy
Troubleshooting Guides & FAQs
This technical support center provides targeted guidance for researchers troubleshooting false positives in machine learning (ML)-enhanced biosensor assays.
Frequently Asked Questions (FAQs)
Q1: My ML-powered biosensor shows high overall accuracy but is missing critical positive cases (e.g., cancer biomarkers). What is wrong? This is a classic example of the Accuracy Paradox [87]. It often occurs when your dataset is imbalanced, meaning one class (e.g., "healthy" samples) significantly outnumbers the other (e.g., "diseased" samples). A model can achieve high accuracy by simply always predicting the majority class, while failing on the critical minority class. To diagnose this, do not rely on accuracy alone; use a confusion matrix and metrics like precision and recall.
Q2: What are the primary sources of false positives in nucleic acid-based biosensors like LAMP assays? The main sources are carry-over contamination from amplicons and nonspecific amplification due to primer-dimer formation [28]. Using a large number of primers (4-6) increases the risk of these interactions, leading to amplification even when the target analyte is absent.
Q3: How can I make my electrochemical immunosensor more reliable against false signals? Implement a built-in error-checking mechanism. One effective approach is to design a sensor with dual- or triple-mode detection (e.g., electrochemical and colorimetric) [88]. This provides a self-validation system, where a signal must be confirmed by two independent transduction methods, minimizing the chance of a false positive from a single, potentially erroneous reading.
Q4: Can the design of the biosensor itself, not just the ML model, contribute to false results? Yes, fundamentally. The sensitivity and specificity start at the biosensor level [1] [89]. Issues such as non-specific binding of antibodies, cross-talk in enzyme-based sensors, or insufficiently optimized plasmonic surfaces can generate erroneous initial data. A poorly performing biosensor will generate noisy or inaccurate data, which no ML model can reliably correct.
Q5: My SERS biosensor data is complex and high-dimensional. How can ML help reduce false interpretations? ML algorithms excel at processing complex, high-dimensional data from techniques like Surface-Enhanced Raman Scattering (SERS) [30] [89]. They can be trained to identify subtle, multi-analyte patterns that are specific to a disease, effectively filtering out random noise or non-specific binding signals that could lead to a false positive.
Troubleshooting Guides
Guide 1: Addressing Data-Related Issues in ML-Biosensor Systems
Problem: High false positive rate traced to data quality and model metrics.
Solution:
- Step 1: Audit Dataset Balance: Calculate the ratio of positive to negative samples in your training and validation sets. If the ratio is highly skewed (e.g., 1:20), the dataset is imbalanced.
- Step 2: Employ Robust Metrics: Stop using accuracy as your primary metric. Instead, use the following to get a true picture of performance [87]:
| Metric | Formula | Use Case When Prioritizing... |
|---|---|---|
| Precision | True Positives / (True Positives + False Positives) | ...the cost of false alarms (False Positives). |
| Recall (Sensitivity) | True Positives / (True Positives + False Negatives) | ...the cost of missing a real positive (False Negative). |
| F1-Score | 2 × (Precision × Recall) / (Precision + Recall) | ...a balanced measure between Precision and Recall. |
| Matthew's Correlation Coefficient (MCC) | (TP×TN - FP×FN) / √((TP+FP)(TP+FN)(TN+FP)(TN+FN)) | ...a reliable score for imbalanced datasets. |
- Step 3: Utilize a Confusion Matrix: Visually inspect where misclassifications are occurring to pinpoint if false positives are a systematic issue.
- Step 4: Apply Data & Algorithm Techniques: For imbalanced data, use techniques like oversampling the minority class (SMOTE), undersampling the majority class, or using ML algorithms that are robust to class imbalance.
The following diagram illustrates the core workflow for diagnosing and addressing data-related false positives:
Guide 2: Mitigating False Positives in Nucleic Acid Amplification Assays (e.g., LAMP)
Problem: Nonspecific amplification and carry-over contamination in isothermal amplification assays.
Solution:
- Step 1: Pre-Amplification Prevention:
- Organic Additives: Include additives like DMSO (5-10%) or betaine in the reaction mix to reduce nonspecific primer binding and improve specificity [28].
- Enzymatic Control: Use Uracil-DNA-Glycosylase (UDG) in the reaction. Incorporate dUTP instead of dTTP in previous amplicons. UDG will degrade any contaminating amplicons before the amplification reaction begins, preventing carry-over contamination [28].
- Hot-Start Effect: Use gold nanoparticles (AuNPs) or other hot-start polymerases to inhibit polymerase activity at low temperatures, preventing primer-dimer formation during reaction setup [28].
- Step 2: Post-Amplification Verification:
- CRISPR/Cas Systems: Use Cas proteins (e.g., Cas12, Cas13) with specific guide RNAs that only cleave a reporter molecule upon binding to the correct amplicon. This confirms that amplification was specific to the target sequence [28].
- Lateral Flow Immunoassay (LFA): Use hybridized probes that are specifically designed to recognize the target amplicon. The LFA strip will only show a positive line if the correct sequence is present, differentiating it from nonspecific products [28].
The table below summarizes key methods for mitigating false positives in LAMP assays:
| Method | Phase | Mechanism | Key Benefit |
|---|---|---|---|
| DMSO/Betaine [28] | Pre-Amplification | Disrupts secondary structures, inhibits nonspecific annealing. | Improves amplification specificity. |
| UDG Treatment [28] | Pre-Amplification | Enzymatically degrades contaminating dUTP-containing amplicons. | Prevents carry-over contamination. |
| Hot-Start AuNPs [28] | Pre-Amplification | Suppresses polymerase activity during setup. | Reduces primer-dimer formation. |
| CRISPR/Cas [28] | Post-Amplification | Specific gRNA recognizes target amplicon, activating reporter cleavage. | Confirms target-specific amplification. |
| Lateral Flow (LFA) [28] | Post-Amplification | Hybridization probe specifically binds target amplicon on strip. | Visually distinguishes true target. |
Guide 3: Optimizing Biosensor Hardware and Assay Design for Specificity
Problem: Physical or chemical limitations of the biosensor cause nonspecific binding and signal interference.
Solution:
- Step 1: Improve Biorecognition Element Orientation: For immunosensors, use oriented immobilization strategies. Employ Protein A, biosynthesized quantum dots (BQDs) with Fc-binding proteins, or other methods to align antibodies via their Fc region. This presents the antigen-binding sites optimally, maximizing binding efficiency and reducing non-specific interactions [88].
- Step 2: Employ Multiplexed & Multi-Modal Sensing: Instead of relying on a single biomarker, use a sensor array to detect multiple biomarkers simultaneously [30] [89]. A true positive is indicated by a specific combination of signals, which is harder to replicate by random noise or interference. Combining multiple detection modes (e.g., electrochemical and colorimetric) in a single platform provides built-in error-checking [88].
- Step 3: Leverage Advanced Nanomaterials: Use nanomaterials with high specificity and conductivity. For example:
- Graphene and MXene can enhance electrical conductivity and provide a large surface area for efficient bioreceptor immobilization [90] [88].
- Au-Ag Nanostars in SERS biosensors create "hot spots" for intense signal enhancement, allowing for sensitive detection of specific biomarkers like α-fetoprotein at low concentrations [5].
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Troubleshooting False Positives |
|---|---|
| Uracil-DNA-Glycosylase (UDG) [28] | Enzyme used to degrade carry-over contamination in nucleic acid assays by breaking down uracil-containing DNA. |
| Dimethyl Sulfoxide (DMSO) [28] | Organic additive that improves amplification specificity in LAMP and PCR by reducing secondary structures. |
| Gold Nanoparticles (AuNPs) [28] | Used for hot-start nucleic acid amplification and as a platform for immobilizing biomolecules in electrochemical sensors. |
| CRISPR/Cas System with gRNA [28] | Provides highly specific post-amplification verification of nucleic acid targets, distinguishing true amplicons. |
| Biosynthesized Quantum Dots (BQDs) [88] | Enable oriented antibody immobilization on sensor surfaces via Fc-binding proteins, enhancing binding efficiency. |
| MXene (e.g., NH2-MXene@AuNPs) [88] | 2D nanomaterial used in electrochemical sensors for its excellent conductivity and large surface area for bioreceptor loading. |
| Au-Ag Nanostars [5] | Plasmonic nanoparticles for SERS biosensors; their sharp tips create intense electromagnetic fields for sensitive, multiplexed detection. |
| Anti-Fc Region Binding Proteins (Protein A/G) [88] | Used for oriented antibody immobilization on biosensor surfaces, ensuring antigen-binding sites are available. |
The following workflow integrates physical biosensor optimization with machine learning data processing to create a robust diagnostic system:
Cost-Benefit Analysis of Different Troubleshooting and Optimization Approaches
False positives in biosensor assays present a significant challenge in diagnostic research and drug development, potentially leading to inaccurate data, misguided clinical decisions, and wasted resources. A false positive occurs when a biosensor incorrectly indicates the presence of a target analyte that is not actually present in the sample. The sources of these inaccuracies are diverse, stemming from issues such as nonspecific binding, carry-over contamination, suboptimal surface chemistry, and interference from complex sample matrices [1] [28]. This technical support guide provides a structured, evidence-based framework for researchers to troubleshoot, optimize, and validate their biosensor assays, thereby enhancing diagnostic reliability.
Troubleshooting Guides and FAQs
General Biosensor Optimization
FAQ: What are the primary strategies to reduce false positives before an assay is run? Proactive optimization of the assay conditions and components is the most effective way to prevent false positives. This includes careful selection of biorecognition elements, optimizing immobilization strategies, and using chemical additives to suppress nonspecific reactions.
Experimental Protocol: Using Organic Additives to Suppress Nonspecific Amplification
- Objective: To reduce primer-dimer formation and nonspecific amplification in nucleic acid-based biosensors like LAMP.
- Methodology:
- Prepare your standard LAMP master mix.
- Introduce organic additives such as Dimethyl sulfoxide (DMSO) (typically 1-10% v/v), betaine (0.5-1.2 M), or pullulan.
- Run the amplification reaction and compare the results with a control reaction without additives.
- DMSO disrupts secondary structures in primers and DNA templates, while betaine destabilizes GC-rich regions and minimizes nonspecific binding, thereby reducing false-positive rates [28].
Experimental Protocol: Employing Uracil-DNA-glycosylase (UDG) to Prevent Carry-over Contamination
- Objective: To eliminate false positives caused by contamination from previous amplification products.
- Methodology:
- Incorporate dUTP instead of dTTP during the nucleic acid amplification step in previous assays.
- In new assays, add the enzyme UDG to the reaction mix prior to the main amplification.
- UDG will enzymatically cleave any uracil-containing contaminating DNA amplicons, preventing their amplification.
- Inactivate UDG by heating before starting the new amplification cycle, ensuring only the target DNA is amplified [28].
FAQ: My biosensor shows a high background signal or drift. What could be the cause? A drifting baseline or high background is often related to the sensor surface or buffer conditions.
- Troubleshooting Steps:
- Check Surface Regeneration: Inefficient regeneration of the sensor surface between runs can cause a buildup of residual material, leading to baseline drift. Ensure you are using an appropriate regeneration buffer and protocol that removes bound analyte without damaging the immobilized ligand [72].
- Verify Buffer Compatibility: Certain buffer components can destabilize the sensor surface. Check for compatibility between your buffer (e.g., salt concentration, detergents) and the sensor chip. Switching to a more compatible buffer can resolve drift issues [72].
- Assess Sample Quality: Impurities, aggregates, or denatured proteins in your sample can non-specifically bind to the surface. Always use high-quality, purified samples to minimize nonspecific binding and baseline instability [72].
SPR Biosensor Specifics
FAQ: How can I minimize non-specific binding in my SPR experiments? Non-specific binding (NSB) is a major contributor to false positives in SPR biosensors.
- Troubleshooting and Optimization Steps:
- Surface Blocking: After immobilizing your ligand, use blocking agents like ethanolamine, casein, or BSA to occupy any remaining active sites on the sensor chip [72].
- Optimize Surface Chemistry: Select a sensor chip tailored to your analyte. For example, CM5 chips with carboxymethylated dextran are versatile, while C1 chips with a flat surface may reduce NSB for larger analytes [72].
- Tune Flow Conditions: A moderate flow rate ensures efficient analyte delivery without causing turbulence that can promote nonspecific adsorption [72].
- Buffer Optimization: Include additives like surfactants (e.g., Tween-20) in your running buffer to prevent unwanted adsorption of proteins or other molecules to the surface [72].
FAQ: The signal from my SPR biosensor is too weak. How can I improve it? Low signal intensity can result from insufficient ligand density or weak interactions.
- Troubleshooting and Optimization Steps:
- Optimize Ligand Immobilization Density: A density that is too low yields a weak signal, while one that is too high can cause steric hindrance. Perform ligand titrations to find the optimal density [72].
- Use High-Sensitivity Chips: For weak interactions or low-abundance analytes, consider using sensor chips with enhanced sensitivity, such as those with a higher surface area or specialized coatings [72].
- Signal Amplification: Integrate signal enhancement strategies. For instance, gold nanoparticle amplification can be used post-capture to significantly boost the signal. Captured gold nanoparticle-antibody complexes act as seeds for in situ metal growth, increasing the optical signal without altering the core assay chemistry [91].
Nucleic Acid Biosensor Specifics
FAQ: How can I confirm if my positive LAMP amplification result is a true positive? Due to its high sensitivity, LAMP is prone to false positives, but post-amplification confirmation methods can validate results.
Experimental Protocol: Using CRISPR/Cas Systems for Specific Amplicon Detection
- Objective: To distinguish specific LAMP amplicons from nonspecific amplification products.
- Methodology:
- Design a guide RNA (gRNA) that is complementary to a specific sequence within the target LAMP amplicon.
- After the LAMP reaction, mix the amplicon with the Cas enzyme (e.g., Cas12a) and the specific gRNA.
- If the target sequence is present, the Cas/gRNA complex will bind and become activated.
- The activated Cas enzyme will non-specifically cleave a reporter molecule (e.g., a fluorescent quenched probe), generating a detectable signal. This double layer of specificity (LAMP + CRISPR) drastically reduces false-positive reports [28].
Experimental Protocol: Using DNAzyme for Colorimetric Confirmation
- Objective: To visually confirm true positive LAMP results.
- Methodology:
- Design LAMP primers to include a G-quadruplex sequence in the amplicon.
- After amplification, add hemin to the reaction product.
- If the G-quadruplex sequence is present (i.e., specific amplification occurred), it will form a complex with hemin to create a DNAzyme with peroxidase-like activity.
- Upon adding a colorless peroxidase substrate (e.g., TMB), the DNAzyme will catalyze a color change to blue, providing visual confirmation of a true positive [28].
Cost-Benefit Analysis of Troubleshooting Approaches
The table below compares the relative cost, time investment, and effectiveness of various optimization methods to help guide your research strategy.
| Optimization Approach | Relative Cost | Time Investment | Key Benefit / Effectiveness | Primary Use Case |
|---|---|---|---|---|
| Organic Additives (DMSO/Betaine) [28] | Low | Low (Simple addition to master mix) | Reduces primer-dimer formation & nonspecific amplification | Nucleic acid amplification assays (e.g., LAMP) |
| UDG Treatment [28] | Low | Low (Pre-incubation step) | Effectively eliminates carry-over contamination | All nucleic acid-based assays; high-throughput labs |
| Buffer Optimization [72] | Low | Medium (Requires testing of different formulations) | Reduces non-specific binding & stabilizes baseline | All biosensor types, especially SPR and electrochemical |
| Surface Chemistry Optimization [72] | Medium | High (Testing different chips/immobilization strategies) | Increases specificity & ligand activity; foundational | SPR and other surface-based biosensors |
| Design of Experiments (DoE) [92] | Medium (software) | High (initial setup) | Systematically optimizes multiple interacting variables | Complex assay development; maximizing performance |
| Dual Modality Biosensors [2] | High | High (Complex fabrication & data integration) | Cross-validation reduces false positives/negatives | Applications requiring high reliability (e.g., clinical Dx) |
| CRISPR-based Confirmation [28] | Medium | Medium (Additional post-assay step) | Very high specificity for amplicon verification | Confirmatory testing after rapid nucleic acid assays |
| Gold Nanoparticle Amplification [91] | Medium | Low-Medium (One-step integration) | Boosts sensitivity & can lower limit of detection | Optical biosensors (Colorimetric, SPR, LFA) |
The Scientist's Toolkit: Key Research Reagent Solutions
This table details essential materials used in the featured optimization protocols and their specific functions.
| Reagent / Material | Function / Explanation |
|---|---|
| DMSO (Dimethyl Sulfoxide) [28] | Organic additive that disrupts secondary structures in DNA/RNA, improving primer specificity and reducing false amplification in LAMP and PCR. |
| Betaine [28] | Reduces base composition bias and destabilizes secondary structures during nucleic acid amplification, leading to more specific target detection. |
| Uracil-DNA-glycosylase (UDG) [28] | Enzyme that degrades uracil-containing DNA from previous amplifications, preventing carry-over contamination and subsequent false positives. |
| Gold Nanoparticles (AuNPs) [91] | Used for signal amplification; captured AuNPs can catalyze a reduction reaction to deposit more metal, enhancing the optical or electrochemical signal. |
| CRISPR/Cas System & gRNA [28] | Provides a highly specific secondary verification; the gRNA guides the Cas enzyme to a specific amplicon sequence, activating a reporter only for true positives. |
| MES Buffer [91] | A buffering agent identified as optimal (e.g., at pH 5 and 150 mM) for certain signal amplification reactions, such as gold nanoparticle growth. |
| Blocking Agents (BSA, Casein) [72] | Proteins used to cover unused binding sites on a sensor surface after ligand immobilization, thereby minimizing non-specific binding of analytes. |
| Surfactants (e.g., Tween-20) [72] | Added to running buffers to reduce hydrophobic interactions between proteins and the sensor surface, minimizing nonspecific binding. |
Detailed Experimental Protocols
Protocol 1: Systematic Optimization Using Design of Experiments (DoE)
Objective: To efficiently optimize multiple interacting variables in biosensor fabrication (e.g., immobilization pH, ligand density, incubation time) using a fraction of the experiments required by the traditional one-variable-at-a-time approach [92].
Methodology:
- Factor Identification: Select the variables (e.g., pH, ionic strength, temperature) you believe affect your biosensor's response.
- Define Experimental Domain: Set the high (+1) and low (-1) levels for each variable.
- Create Experimental Matrix: Use a statistical design, such as a 2^k factorial design. For 3 variables, this requires 8 experiments. The matrix defines the specific conditions for each run.
- Run Experiments: Perform all experiments in a randomized order to avoid systematic bias.
- Model Building & Analysis: Use the response data (e.g., signal intensity, signal-to-noise) to build a linear model (e.g.,
Y = b0 + b1X1 + b2X2 + b12X1X2). The coefficients reveal the influence of each variable and their interactions. - Validation: Run a confirmation experiment at the predicted optimal conditions to validate the model.
This approach is highly cost-effective as it reveals interactions between variables that would be missed otherwise, leading to a more robust and optimized assay [92].
Protocol 2: Implementing a Dual Modality Biosensor for Cross-Validation
Objective: To develop a biosensor that combines two detection methods (e.g., electrochemical and optical) to cross-validate results, thereby significantly reducing the risk of false positives and negatives [2].
Methodology:
- Platform Design: Fabricate a biosensor platform that integrates both transduction mechanisms. A common example is an electrode decorated with plasmonic nanoparticles.
- Assay Execution: Upon introduction of the analyte, both signals are measured simultaneously or sequentially.
- Electrochemical Signal: e.g., a change in current or impedance due to a binding event.
- Optical Signal: e.g., a color change or shift in local surface plasmon resonance (LSPR) from the same nanoparticles.
- Data Analysis: The signals are analyzed independently and then compared. A true positive is confirmed only if both modalities show a positive response for the same sample. This internal cross-validation makes the biosensor exceptionally reliable for complex samples [2].
Workflow Visualization
Systematic Biosensor Optimization Workflow
The diagram below outlines a logical pathway for diagnosing and addressing false positives in biosensor assays, incorporating both established and advanced strategies.
Conclusion
Effectively troubleshooting false positives in biosensor assays requires a holistic approach that spans from fundamental design to advanced data analysis. The integration of systematic troubleshooting frameworks, such as those demonstrated to double assay success rates, is as critical as technological innovations like machine learning and dual-mode sensing. Future efforts must focus on the clinical translation of these robust assays, emphasizing the development of standardized validation protocols and scalable fabrication techniques. By addressing the root causes of inaccuracy through interdisciplinary strategies, biosensor technology can fully realize its potential to deliver reliable, point-of-care diagnostics that significantly impact biomedical research and patient care.
References
- 1. Biosensors, Artificial Intelligence Biosensors, False Results ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025796/]
- 2. Recent advancements in dual modality biosensors for ... [https://www.sciencedirect.com/science/article/abs/pii/S016599362500322X]
- 3. Nano-scale biosensor lets scientists monitor molecules in real ... [https://news.stanford.edu/stories/2025/05/nano-scale-biosensor-monitor-molecules-real-time]
- 4. Grand Challenges in Biosensors and Biomolecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8377753/]
- 5. Biosensors, Volume 15, Issue 9 (September 2025) [https://www.mdpi.com/2079-6374/15/9]
- 6. The Example of Blood Glucose Meters [https://www.mdpi.com/2227-9040/13/8/300]
- 7. New method developed to dramatically enhance bioelectronic ... [https://news.rice.edu/news/2025/new-method-developed-dramatically-enhance-bioelectronic-sensors]
- 8. Frontiers | Advanced biosensor technology for mycotoxin detection [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1596690/full]
- 9. Label-free biosensor decodes the... | Nature Communications assay [https://www.nature.com/articles/s41467-024-53770-9?error=cookies_not_supported&code=b11c9c72-d265-4e8b-8172-6a7a728fa835]
- 10. Machine learning for detecting DNA attachment on SPR ... [https://www.nature.com/articles/s41598-023-29395-1]
- 11. Improving biosensor accuracy and speed using dynamic ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566323007716]
- 12. Biosensors at the crossroads of food safety and ... [https://link.springer.com/article/10.1007/s44373-025-00061-7]
- 13. Bioreceptor modified electrochemical biosensors for the ... [https://pubs.rsc.org/en/content/articlehtml/2024/ra/d4ra04038d]
- 14. Antibody-receptor bioengineering and its implications in ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813022015410]
- 15. Investigation of Limitations in the Detection of Antibody ... [https://www.mdpi.com/1424-8220/23/17/7490]
- 16. Sensitivity and dynamics of bioreceptor-based biosensors [https://pubmed.ncbi.nlm.nih.gov/2829685/]
- 17. Transformative biomedical devices to overcome biomatrix ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566325002477]
- 18. Advances and challenges in biosensor-based diagnosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4104499/]
- 19. An Introduction To Immunoassay Interference | Blog [https://www.biosynth.com/blog/immunoassay-interference]
- 20. Matrix-insensitive protein assays push the limits of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4165514/]
- 21. Troubleshooting [https://www.sprpages.nl/troubleshooting]
- 22. A paper biosensor for overcoming matrix effects interfering ... [https://link.springer.com/article/10.1007/s00604-023-06017-1]
- 23. Biolayer interferometry and its applications in drug ... [https://www.sciencedirect.com/science/article/pii/S0165993624002243]
- 24. Discrimination of specific and non-specific bindings by ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566308006337]
- 25. 14 Valuable Ways To Troubleshoot Current Transducer ... [https://www.hangzhiprecision.com/blog/14-valuable-ways-to-troubleshoot-current-transducer-problems/]
- 26. Pressure Transducer Troubleshooting Extreme Environments [https://sucoesi.com/pressure-transducer-troubleshooting-extreme-environments/]
- 27. Signal-to-Noise Ratio as a Quantitative Measure for Optical ... [https://www.analog.com/en/resources/design-notes/signaltonoise-ratio-as-a-quantitative-measure-for-optical-biosensors.html]
- 28. Diverse methods of reducing and confirming false-positive ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267023009145]
- 29. Machine learning in point-of-care testing: innovations, ... [https://www.nature.com/articles/s41467-025-58527-6]
- 30. Advancement of machine learning algorithms in biosensors [https://www.sciencedirect.com/science/article/abs/pii/S000989812500556X]
- 31. Machine learning for biosensor signal processing [https://www.sciencedirect.com/science/article/abs/pii/B9780443364341000380]
- 32. A high content assay for biosensor validation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4324324/]
- 33. Challenges and Opportunities in Smart Biosensing for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12455640/]
- 34. CRISPR-Cas12a-Powered Dual - Mode for Ultrasensitive... Biosensor [https://pubmed.ncbi.nlm.nih.gov/34281340/]
- 35. A Portable, Visual, and Dual - Mode for... | SpringerLink Biosensor [https://link.springer.com/protocol/10.1007/978-1-0716-4358-7_16]
- 36. Biosensors, Volume 15, Issue 5 (May 2025) – 69 articles [https://www.mdpi.com/2079-6374/15/5]
- 37. Non-Specific Adsorption Reduction Methods in Biosensing [https://pmc.ncbi.nlm.nih.gov/articles/PMC6603772/]
- 38. Self-assembly strategy to reduce non-specific adsorption ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267022009382]
- 39. Promising Solutions to Address the Non-Specific ... [https://www.mdpi.com/2227-9040/13/3/92]
- 40. Nanomaterial surface modification toolkit: Principles, ... [https://www.sciencedirect.com/science/article/pii/S0001868623002026]
- 41. Nanoparticle Surface Functionalization: How to Improve ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2020.587012/full]
- 42. Recent advancements in microfluidic-based biosensors for ... [https://www.sciencedirect.com/science/article/pii/S2590137024000530]
- 43. a promising analytical tool for on-site detection of mycotoxins [https://www.nature.com/articles/s41538-025-00444-5]
- 44. for biomarker detection in body fluids: a key... Microfluidic biosensors [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-024-00697-4]
- 45. Microfluidic space coding for multiplexed nucleic acid ... [https://www.nature.com/articles/s41467-022-34086-y]
- 46. Microfluidic chip systems for color-based antimicrobial ... [https://www.sciencedirect.com/science/article/abs/pii/S095656632500034X]
- 47. Protein-binding Aptamers: The What And The How [https://aptamergroup.com/protein-binding-aptamers/]
- 48. Aptamer Stability Analysis - Creative Biolabs [https://www.creative-biolabs.com/complement-therapeutics/aptamer-stability-analysis.htm]
- 49. Aptamers: Design, Theory, and Applications to Diagnosis and Therapy for Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12086380/]
- 50. Conversion of RNA aptamer into modified DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12486140/]
- 51. Recent Advances in the Optimization of Nucleic Acid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564743/]
- 52. 5 Whys vs Fishbone Diagram [https://aigproexcellence.com/blog/5-whys-vs-fishbone-diagram/]
- 53. How to Conduct a 5 Whys Root Cause Analysis? [https://easyrca.com/blog/how-to-conduct-5-whys-root-cause-analysis/]
- 54. 🎣 Solving Problems with the Fishbone Diagram: A Practical ... [https://www.linkedin.com/pulse/solving-problems-fishbone-diagram-practical-guide-gim2c]
- 55. Using the 5 Whys Method to Identify and Solve Problems [https://oncpracticemanagement.com/issues/2021/april-2021-vol-11-no-4/using-the-5-whys-method-to-identify-and-solve-problems]
- 56. How to Create a Fishbone - Edraw Diagram [https://edraw.wondershare.com/make-fishbone-diagram.html]
- 57. Point-of-care biosensors for infectious disease diagnosis [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03897a?page=search]
- 58. The Challenges of Developing Biosensors for Clinical ... [https://www.mdpi.com/2227-9040/9/11/299]
- 59. Label-Free Electrochemical Biosensor for Real-Time ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566325008371]
- 60. Label-free biosensor assay decodes the dynamics of Toll- ... [https://www.nature.com/articles/s41467-024-53770-9]
- 61. Experimental design (Chapter 2) - Label-Free Biosensors [https://www.cambridge.org/core/books/labelfree-biosensors/experimental-design/52225A62F2947448E81638FC937D85FB]
- 62. Buffers: Blocking Sensitivity & Assay Biosensors [https://justanswers.blog/blocking-buffers-assay-biosensors/]
- 63. Resonating with replicability: factors shaping assay yield and variability... [https://pubs.rsc.org/en/content/articlelanding/2025/lc/d5lc00575b]
- 64. Development and Optimization of a Cost-Effective ... [https://www.mdpi.com/2079-6374/15/2/67]
- 65. Interference and Artifacts in High-content Screening - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK615088/]
- 66. What is Matrix Interference and How Does It Affect Testing? [https://www.arborassays.com/what-is-matrix-interference/?srsltid=AfmBOorWf8MgS7eDSnUgJoWwXnprLlEZzeHxvW8Nm61u2bkH8hF0Vd9k]
- 67. A Closer Look at Biosensors: A Practical Tutorial for ... [https://www.spectroscopyonline.com/view/a-closer-look-at-biosensors-a-practical-tutorial-for-spectroscopists]
- 68. Evaluating and mitigating clinical samples matrix effects on ... [https://www.nature.com/articles/s41598-022-17583-4]
- 69. Evaluating and mitigating clinical samples matrix effects on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9374283/]
- 70. Strategies for Enhancing the Signal-to-Noise Ratio in ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993625003620]
- 71. A guide to reducing noise and increasing sensitivity in ... [https://blog.igii.uk/a-guide-to-reducing-noise-and-increasing-sensitivity-in-biosensors]
- 72. Troubleshooting and Optimization Tips for SPR Experiments [https://www.creative-proteomics.com/resource/troubleshooting-optimization-tips-for-spr-experiments.htm]
- 73. Development of surface plasmon resonance biosensor for... assays [https://research.vu.nl/en/publications/development-of-surface-plasmon-resonance-biosensor-assays-for-pri/]
- 74. Point-of-care biosensors for infectious disease diagnosis: recent... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03897a]
- 75. Emerging trends in AI-integrated optical biosensors for point ... [https://pubs.rsc.org/en/content/articlehtml/2025/cc/d5cc04899k]
- 76. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 77. Sensitivity and specificity [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]
- 78. Benchmarking performance with sensitivity, specificity, ... [https://epi2me.nanoporetech.com/benchmarking-performance/]
- 79. Tentacle probes: eliminating false positives without ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1904288/]
- 80. 8 qPCR amplification plot questions answered - LGC [https://blog.biosearchtech.com/8-qpcr-amplification-plot-questions-answered]
- 81. Triple-mode biosensing strategies: A critical review of ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25023550]
- 82. Visual and fluorescence dual mode platform for sensitive ... [https://pubmed.ncbi.nlm.nih.gov/39705784]
- 83. Dual-Mode Biosensor for Simultaneous and Rapid ... [https://www.mdpi.com/2079-6374/13/3/401]
- 84. A paper biosensor for overcoming matrix effects interfering ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10579119/]
- 85. Biosensors Designed for Clinical Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8301448/]
- 86. Products | SPR Biosensors | FAQ [https://www.xantec.com/products/spr_biosensors/faq.php]
- 87. How to Check the Accuracy of Your Machine Model in Learning 2025 [https://www.deepchecks.com/how-to-check-the-accuracy-of-your-machine-learning-model/]
- 88. An oriented self-assembly biosensor with built-in error ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566324009126]
- 89. Recent advances in SERS assays for detection of multiple extracellular... [https://pubs.rsc.org/en/content/articlehtml/2025/nr/d4nr04014g]
- 90. Enhancement and optimization of a graphene-based ... [https://www.nature.com/articles/s41598-025-20570-0]
- 91. Simulation-Guided Optimization of One-Step Gold ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566325010838]
- 92. Perspectives on systematic optimization of ultrasensitive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11403992/]