Wearable Biosensors for Continuous Health Monitoring: Technologies, Applications, and Future Frontiers in Biomedical Research
This article provides a comprehensive analysis of the current state and future trajectory of wearable biosensors for continuous health monitoring, tailored for researchers, scientists, and drug development professionals.
Wearable Biosensors for Continuous Health Monitoring: Technologies, Applications, and Future Frontiers in Biomedical Research
Abstract
This article provides a comprehensive analysis of the current state and future trajectory of wearable biosensors for continuous health monitoring, tailored for researchers, scientists, and drug development professionals. It explores the foundational principles of biosensing technologies, including electrochemical, optical, and piezoelectric transducers, and their integration into flexible, miniaturized platforms. The scope extends to cutting-edge methodological applications, such as therapeutic drug monitoring (TDM) and the management of chronic diseases, leveraging non-invasive sampling of biofluids like sweat, saliva, and tears. The review critically addresses persistent challenges in sensor accuracy, power efficiency, and data standardization, while evaluating validation frameworks and performance metrics essential for clinical adoption. By synthesizing insights from recent academic literature and market analyses, this article aims to serve as a foundational resource for innovators shaping the next generation of personalized and predictive healthcare tools.
The Foundation of Modern Biosensing: Core Principles and Technological Evolution
Wearable biosensors are defined as wearable sensing devices that incorporate a biological recognition element and a physico-chemical transducer to provide continuous, real-time physiological information via dynamic, non-invasive measurements of biomarkers in biofluids such as sweat, tears, saliva, and interstitial fluid [1]. These devices have revolutionized contemporary medical healthcare monitoring systems by decentralizing the concept of regular clinical check-ups towards more versatile, remote, and personalized healthcare [2]. The fundamental operational principle involves the highly specific recognition of a target analyte by a bioreceptor, followed by the transduction of this biorecognition event into a quantifiable signal that can be processed, analyzed, and communicated [1] [2]. This architecture enables the continuous monitoring of dynamic biochemical processes, providing invaluable insights into a wearer's health status, enhancing chronic disease management, and alerting users or medical professionals to abnormal physiological situations [1].
Fundamental Components of Wearable Biosensors
Biorecognition Elements
The biorecognition element is responsible for the selective recognition of the target analyte and is the foundation of biosensor specificity [1] [2]. These elements can include enzymes, antibodies, whole cells, aptamers, and molecularly imprinted polymers [2]. Recent developments have favored aptamers due to their high specificity and sensitivity, along with superior stability compared to protein-based receptors [2]. The immobilization strategy for these biorecognition elements on the sensor surface is critical for maintaining their bioactivity and orientation, directly impacting sensor performance, stability, and shelf life [2]. Physical adsorption, covalent bonding, encapsulation, and affinity-based immobilization represent common approaches, each with distinct advantages for specific applications and operational environments [2].
Transduction Mechanisms
The physico-chemical transducer converts the biological recognition event into a measurable signal [1]. The primary transduction mechanisms in wearable biosensors include:
- Electrochemical Transduction: Measures electrical signals generated by biochemical reactions, including amperometric (current), potentiometric (potential), and conductometric (conductivity) measurements [2]. These sensors benefit from simple setup, cost efficiency, robust detection limits, and high specificity [2].
- Optical Transduction: Utilizes light-matter interactions for detection, including colorimetric, fluorescence, and surface plasmon resonance techniques [1] [3]. Recent advances include nanozyme-based colorimetric detection that offers high sensitivity, stability, and adjustable catalytic activities [3].
- Mechanical Transduction: Relies on physical changes such as mass, force, or pressure variations, often measured through piezoresistive, capacitive, or piezoelectric effects [2].
Table 1: Comparison of Primary Transduction Mechanisms in Wearable Biosensors
| Transduction Mechanism | Measured Parameter | Advantages | Common Applications |
|---|---|---|---|
| Electrochemical | Current, potential, or impedance | High specificity, low cost, miniaturization capability | Glucose monitoring (e.g., Freestyle Libre [1]), lactate, electrolytes |
| Optical | Light intensity, wavelength, or phase | Visual readouts, multiplexing capability | Colorimetric glucose patches [3], sweat pH monitoring |
| Mechanical | Mass, pressure, or force | Direct physical measurement, high sensitivity | Pulse monitoring, pressure-sensitive insoles |
Advanced Materials and Fabrication Strategies
The development of advanced materials has been instrumental in enhancing the wearability and performance of biosensors. Flexibility and stretchability are essential requirements for wearable biosensors to ensure comfort and maintain consistent skin contact during movement [2]. Material innovations include:
- Polymer-based composites with embedded nanostructures that maintain electrical conductivity under mechanical deformation [4]
- Skin-inspired patterned meshes that adapt to the human body's curvilinear surface [2]
- Hydrogels, textiles, and paper-based substrates that provide flexible, stretchable, and breathable platforms [2]
These advanced materials enable the development of epidermal wearable biosensors that conform to skin topography while maintaining biosensing functionality, facilitating real-time analysis of biomarkers in epidermal biofluids such as sweat and interstitial fluid [1]. Recent demonstrations include polymer-based sensors that withstand over 1,000 cycles of mechanical deformation with minimal resistance drift (<3%), enabling robust continuous monitoring during daily activities [4].
Experimental Protocols for Wearable Biosensor Development
Protocol: Fabrication of Flexible Electrochemical Biosensor
This protocol outlines the fabrication of a flexible electrochemical biosensor for metabolite monitoring (e.g., glucose, lactate) in sweat [2] [4].
Materials Required:
- Flexible polymer substrate (e.g., PET, PI, or elastomeric material)
- Conductive inks (e.g., carbon, Ag/AgCl, or graphene-based)
- Biorecognition elements (e.g., glucose oxidase, lactate oxidase)
- Cross-linking agents (e.g., glutaraldehyde, BS³)
- Encapsulation material (e.g., silicone, polyurethane)
- Screen-printing or inkjet printing equipment
Procedure:
- Substrate Preparation: Clean the flexible substrate with sequential washes of ethanol and deionized water, then dry under nitrogen stream.
- Electrode Fabrication: Deposit working, reference, and counter electrodes using screen-printing or inkjet printing techniques.
- Thermal Curing: Cure the printed electrodes at appropriate temperature (typically 60-90°C) for 1-2 hours to ensure adhesion and stability.
- Bioreceptor Immobilization: Apply biorecognition element solution to working electrode, followed by cross-linking agent to covalently bind the biological element.
- Membrane Application: Apply protective membrane (e.g., Nafion) to minimize biofouling and interference.
- Encapsulation: Apply encapsulation material to all non-sensing areas to ensure mechanical stability and electrical insulation.
- Quality Control: Verify electrode functionality through cyclic voltammetry in standard solutions (e.g., potassium ferricyanide).
Validation: Perform calibration with standard solutions of target analyte across physiological range. Assess sensor-to-sensor reproducibility (target CV <5%), sensitivity, and limit of detection.
Protocol: Integration with Wireless Data Transmission
This protocol describes the integration of biosensing elements with wireless communication modules for real-time data transmission [4].
Materials Required:
- Fabricated biosensor platform
- Microcontroller unit (e.g., ARM Cortex-M series)
- Bluetooth Low Energy (BLE) module
- Power source (e.g., flexible battery or energy harvesting system)
- Mobile device or custom receiver for data collection
Procedure:
- Signal Conditioning Circuit Design: Design and implement front-end electronics for signal amplification and filtering appropriate to the transducer type.
- Microcontroller Programming: Program microcontroller to coordinate sensor sampling, signal processing, and data transmission.
- BLE Integration: Interface BLE module with microcontroller for wireless communication.
- Power Management: Implement power-saving strategies (e.g., duty cycling) to extend operational lifetime.
- Data Logging Firmware: Develop firmware for temporary data storage and transmission protocols.
- Mobile Application: Develop companion mobile application for data visualization, storage, and remote transmission.
- System Validation: Test end-to-end system functionality, including packet loss (target <1% [4]), latency, and power consumption under realistic use conditions.
Signaling Pathways and System Architecture
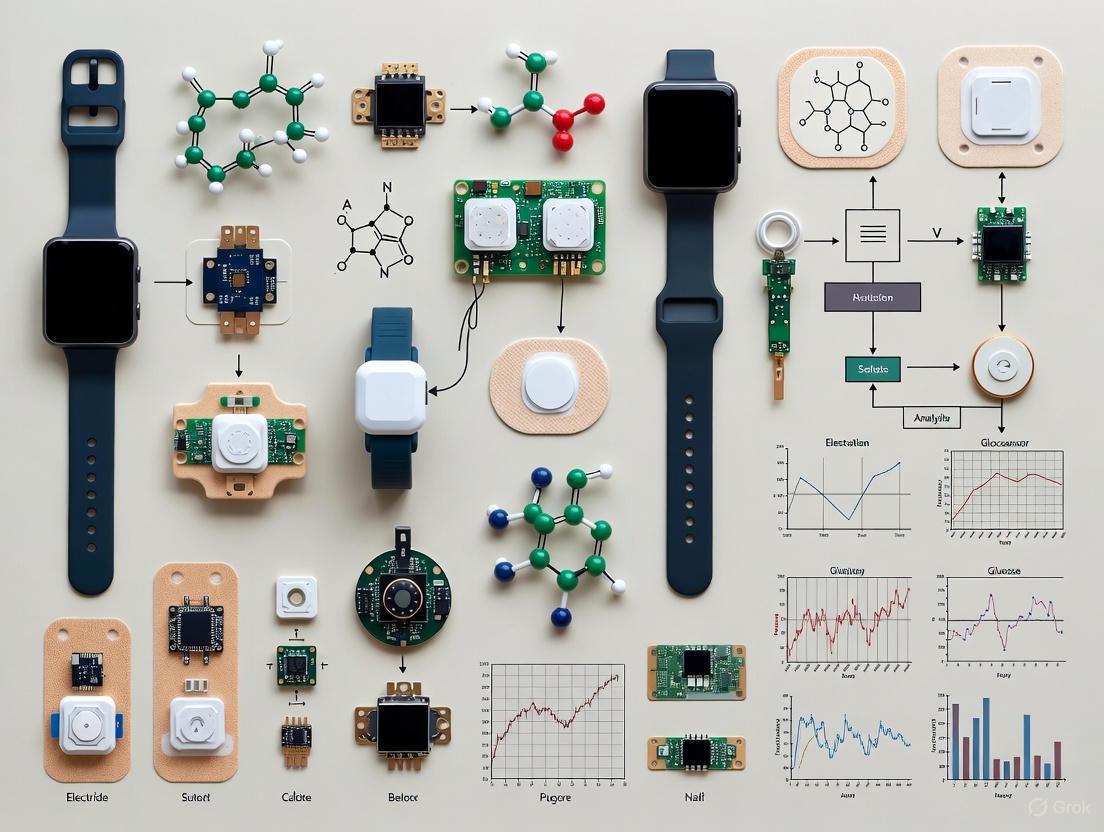
The following diagrams illustrate the fundamental architecture of wearable biosensors and the signal transduction pathways.
Diagram 1: Fundamental biosensor system architecture showing the pathway from analyte recognition to signal output.
Diagram 2: Classification of transduction mechanisms used in wearable biosensors.
Performance Metrics and Validation
Rigorous performance validation is essential for assessing wearable biosensor functionality and reliability. Key metrics include:
Table 2: Key Performance Metrics for Wearable Biosensor Evaluation
| Performance Parameter | Target Specification | Testing Methodology |
|---|---|---|
| Sensitivity | Sufficient to detect physiological analyte ranges | Calibration curve from standard solutions |
| Selectivity | >90% response to target vs. interferents | Interference testing with common biomarkers |
| Response Time | <60 seconds for real-time monitoring | Dynamic response measurement after analyte introduction |
| Operational Stability | <5% signal drift over 24 hours | Continuous operation in simulated biofluid |
| Mechanical Durability | <5% signal change after deformation | Performance testing during/after bending cycles |
| On-body Accuracy | MARD <10% vs. reference method | Clinical comparison study with gold standard |
Validation should progress from in-vitro testing in controlled laboratory conditions to in-vivo testing in realistic use environments [1] [2]. This includes assessing sensor performance during physical activity, environmental changes, and over extended wear periods. Additionally, correlation between analyte concentrations in non-invasive biofluids (e.g., sweat, tears) and blood levels must be established for clinical relevance [1] [3].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Wearable Biosensor Development
| Reagent/Material | Function | Example Applications |
|---|---|---|
| Graphene & CNTs | Conductive nanomaterial with high surface area | Electrode modification for enhanced sensitivity [2] [4] |
| Molecularly Imprinted Polymers | Synthetic biorecognition elements | Stable alternative to biological receptors [2] |
| Nanozymes | Enzyme-mimicking nanomaterials | Colorimetric detection with enhanced stability [3] |
| Ionophores | Ion-selective recognition elements | Potentiometric sensing of electrolytes (Na+, K+) [2] |
| Cross-linking Agents | Bioreceptor immobilization | Covalent attachment to transducer surfaces [2] |
| Blocking Agents | Minimize non-specific binding | Improve selectivity in complex biofluids [2] |
| Hydrogel Matrix | Biofluid sampling and transport | Controlled analyte delivery to sensing interface [1] |
Emerging Trends and Future Perspectives
The field of wearable biosensors is rapidly evolving with several emerging trends shaping future developments:
Artificial Intelligence Integration: Machine learning and deep learning algorithms enhance real-time data processing, artifact rejection, and predictive analytics [5] [4] [6]. Recent demonstrations include hybrid CNN-LSTM architectures achieving 98.3% classification accuracy for physiological events [4].
Multimodal Sensing Systems: Integration of multiple sensing modalities within a single platform for comprehensive health assessment [7] [6]. These systems simultaneously monitor chemical biomarkers (e.g., glucose, lactate) and physical parameters (e.g., heart rate, activity).
Advanced Material Innovations: Development of self-healing materials, biodegradable substrates, and nanocomposites that enhance sensor longevity, sustainability, and biocompatibility [6].
Closed-Loop Therapeutic Systems: Integration of biosensing with feedback-controlled therapeutic intervention, such as closed-loop insulin delivery systems [7].
Despite significant progress, challenges remain in sensor calibration, long-term stability, and large-scale validation [1]. Future research directions include expanding the repertoire of measurable biomarkers, improving understanding of correlations between non-invasive biofluid concentrations and blood chemistry, and enhancing the commercial translation of research prototypes into clinically validated devices [1] [2].
The field of medical technology has undergone a profound transformation, evolving from single-function therapeutic devices to sophisticated, continuous health monitoring platforms. This evolution began with the first implantable pacemakers and has now reached its current state with wearable biosensors capable of tracking a vast array of biochemical and biophysical parameters. For researchers and drug development professionals, understanding this progression is not merely an academic exercise; it provides a critical framework for innovating next-generation diagnostic tools and personalized therapeutic strategies. These platforms are foundational to the shift from reactive, hospital-centered healthcare to a proactive, individual-centered model, enabling real-time biomarker quantification that informs clinical decisions and pharmaceutical research [8].
Historical Milestones: From Therapeutic to Diagnostic & Monitoring Tools
The journey of biomedical devices is marked by key innovations that progressively increased their functionality, miniaturization, and intelligence. The following table summarizes this evolution, highlighting the transition from simple life-sustaining devices to complex monitoring systems.
Table 1: Historical Evolution of Key Biomedical Device Technologies
| Era | Dominant Technology | Key Parameters Measured | Limitations & Challenges |
|---|---|---|---|
| Mid-20th Century | Early Implantable Pacemakers (e.g., VVI, AAI modes) [9] | Chamber sensing and pacing (Atrial/Ventricular) [9] | Large size, single-function, no sensor feedback, limited programmability [8] [9] |
| Late 20th Century | Advanced Pacemakers & Early Wearables (e.g., DDD mode, GlucoWatch) [8] [9] | A-V sequential pacing, non-invasive glucose [8] [9] | Invasive for implants, skin irritation for wearables, single analyte focus, limited battery life [8] |
| Early 21st Century | Consumer Fitness Trackers & CGM | Heart rate, step count, continuous glucose | Lack of clinical validation, focus on biophysical/one biochemical parameter, reliance on batteries [8] [10] |
| Present Day (2025) | All-in-One, Self-Powered Multi-Parameter Platforms [10] [11] | Metabolites (e.g., vitamins, amino acids), nutrients, hormones, drugs, ECG, activity [10] [12] [11] | Material stability, data security, miniaturization-information trade-offs, biocompatibility [10] |
This progression shows a clear trend: from therapeutic to diagnostic, from single-parameter to multi-parameter, from invasive to non-invasive, and from power-hungry to self-powered [8] [10].
Modern Multi-Parameter Sensing Platforms: Core Technologies
Contemporary platforms integrate several advanced technologies to achieve continuous, multi-analyte monitoring.
Sensing Modalities and Material Innovations
Modern wearable biosensors are classified based on their sensing principles and the type of data they collect:
- Biophysical Sensors: Measure parameters like heart rate, blood pressure, and temperature. These are widely marketized and used in consumer devices like smartwatches [8].
- Biochemical Sensors: Detect analytes in biological fluids like sweat, saliva, and tears. These represent the cutting edge of research, focusing on metabolites (glucose, lactate), nutrients (amino acids, vitamins), hormones, and pharmaceuticals [8] [12] [11]. A key advancement is the use of electrochemical biosensors, which offer high sensitivity, quick response, and low power consumption [8] [12]. Material science plays a critical role, with innovations in graphene electrodes, hybrid and metallic nanoparticles, and nanocomposites significantly improving sensor performance [8] [11].
The Paradigm of Self-Powered Systems
A critical challenge for continuous wearables is power. The latest research focuses on all-in-one, self-powered systems that harvest energy from the user's body or environment, eliminating the need for bulky batteries [10]. These systems integrate six essential modules:
- Energy Harvesting: Capturing energy from motion (Triboelectric/Piezoelectric Nanogenerators - TENGs/PENGs), heat (Thermoelectric Generators - TEGs), biofluids (Enzyme-Based Biofuel Cells - E-BFCs), or light (Solar Cells - SCs) [10].
- Energy Management: Converting and stabilizing the harvested energy using circuits and supercapacitors [10].
- Energy Storage: Storing excess energy for continuous operation [10].
- Signal Acquisition: Detecting the biochemical or biophysical signals via the sensors [10].
- Signal Processing: Analyzing and digitizing the collected data [10].
- Signal Transmission: Wirelessly sending information to external devices like smartphones [10].
Machine learning is increasingly used to optimize these systems by predicting energy availability and dynamically adjusting sensor operation to conserve power [10].
Mass Production through Advanced Manufacturing
Transitioning from lab prototypes to widespread use requires scalable manufacturing. A groundbreaking approach developed in 2025 involves inkjet printing arrays of core-shell cubic nanoparticles [11]. This technique allows for the mass production of inexpensive, long-lasting sweat sensors. The nanoparticles consist of a molecularly imprinted polymer (MIP) shell that acts as an artificial antibody, selectively capturing target molecules (e.g., vitamins, drugs), and a nickel hexacyanoferrate (NiHCF) core that generates an electrical signal. The presence of the target molecule alters this signal, enabling precise quantification [11].
Application Notes & Experimental Protocols
Protocol 1: Monitoring Metabolites and Nutrients via a Wearable Sweat Sensor
This protocol is adapted from a 2022 study for a fully integrated, wearable electrochemical biosensor capable of continuous, multiplexed analysis of trace-level metabolites and nutrients in sweat [12].
1. Principle: The sensor uses graphene electrodes functionalized with antibody-like Molecularly Imprinted Polymers (MIPs) and redox-active reporter nanoparticles. Each MIP is specific to a target analyte (e.g., an essential amino acid or vitamin). The binding of the analyte to the MIP induces a measurable change in the electrochemical signal [12].
2. Workflow:
3. Key Steps:
- Sensor Fabrication: Construct the flexible sensor patch. Pattern graphene-based working, reference, and counter electrodes on a flexible substrate. Functionalize each working electrode with a specific MIP "ink" designed for a target analyte (e.g., tryptophan, vitamin C) [12] [11].
- System Integration: Integrate the sensor with a microfluidic channel for sweat sampling and transport, an iontophoresis module for controlled sweat induction, and the necessary electronics for potentiostatic control, signal processing, and wireless data transmission (e.g., Bluetooth Low Energy) [12].
- Calibration: Calibrate the sensor in vitro using artificial sweat solutions with known concentrations of the target analytes to establish a standard curve for signal-to-concentration conversion [12].
- Human Subject Testing: Apply the sensor to the volunteer's skin (e.g., forearm). Activate the iontophoresis module to induce sweat. Initiate continuous monitoring of the electrochemical signal (e.g., via chronoamperometry or square wave voltammetry) throughout the study period, which can include periods of rest and controlled physical exercise [12].
- Data Correlation & Validation: Periodically collect sweat and blood samples from the volunteer for parallel analysis using gold-standard methods (e.g., mass spectrometry). Correlate the sensor's real-time readings with the lab-based results to validate accuracy and assess serum-sweat correlations for specific biomarkers [12].
4. Applications:
- Real-time monitoring of amino acid intake and utilization during exercise [12].
- Assessment of metabolic syndrome risk by correlating amino acid levels in serum and sweat [12].
- Precision nutrition studies [12].
Protocol 2: Evaluating a Self-Powered, Printed Nanoparticle Sensor for Therapeutic Drug Monitoring (TDM)
This protocol is based on a 2025 study demonstrating the use of printed, molecule-selective nanoparticles for monitoring anti-tumor drug levels in cancer patients, pointing the way to personalized dosing [11].
1. Principle: Core-shell nanoparticles with a NiHCF core and a MIP shell are printed onto a substrate to form a sensor array. When a target drug molecule (e.g., a chemotherapeutic agent) binds to the shape-specific cavities in the MIP shell, it blocks the analyte fluid from reaching the NiHCF core, causing a measurable change in the electrical signal proportional to the drug concentration [11].
2. Workflow:
3. Key Steps:
- Nanoparticle Synthesis: Synthesize core-shell nanoparticles for each target drug. For a given chemotherapeutic drug, form the NiHCF core. Then, assemble the MIP shell in the presence of the drug molecules, which act as templates. Use a solvent to remove the template molecules, leaving behind cavities complementary in shape and size to the drug [11].
- Sensor Fabrication via Printing: Prepare an ink solution containing the synthesized nanoparticles. Use a commercial inkjet printer to deposit the ink onto a flexible, wearable substrate (e.g., a sweat patch) or an implantable substrate, creating a multiplexed array for different drugs [11].
- In-Vitro Characterization: Test the printed sensors in a simulated biological fluid (PBS or artificial sweat) containing known concentrations of the target drug. Perform calibration curves, selectivity tests against common interferents, and stability assessments over time [11].
- Pre-Clinical/Clinical Testing: For wearable application, deploy the patch on consenting cancer patients undergoing chemotherapy. For implantable application, conduct studies in animal models, subcutaneously implanting the sensor. Continuously monitor the electrical signal from the sensor. In parallel, take periodic blood draws from the patient/animal to measure drug concentration using the standard method (e.g., Liquid Chromatography with tandem mass spectrometry - LC-MS/MS) [11].
- Data Analysis: Correlate the continuous sensor readouts with the discrete LC-MS/MS measurements from blood plasma. Analyze the pharmacokinetic profile of the drug and assess the feasibility of real-time, remote TDM [11].
4. Applications:
- Personalized dosing for chemotherapy and other conditions with narrow therapeutic windows [11].
- Remote monitoring of drug pharmacokinetics in clinical trials and routine care [11].
The Scientist's Toolkit: Key Research Reagent Solutions
The development and implementation of advanced wearable biosensors rely on a suite of specialized materials and reagents. The following table details key components for constructing these platforms.
Table 2: Essential Research Reagents and Materials for Wearable Biosensor Development
| Reagent/Material | Function/Application | Specific Example |
|---|---|---|
| Molecularly Imprinted Polymer (MIP) "Inks" | Serve as synthetic, stable recognition elements on sensor electrodes; selectively bind target analytes (vitamins, drugs, hormones) [12] [11]. | Core-shell nanoparticles with NiHCF core and MIP shell for vitamin C or tryptophan [11]. |
| Graphene & Carbon-based Inks | Form the base of flexible, high-surface-area working electrodes; provide excellent electrical conductivity for electrochemical sensing [8] [12]. | Graphene electrodes functionalized with MIPs and redox-active reporters [12]. |
| Nickel Hexacyanoferrate (NiHCF) | Acts as a stable, redox-active core in nanoparticles; generates an electrical signal when in contact with biofluids, which is modulated by analyte binding [11]. | Core material in printable, molecule-selective nanoparticles [11]. |
| Flexible Substrate Materials | Provide a conformal, skin-compatible base for mounting sensors and electronics; enable comfort and reliable skin contact for long-term monitoring [8] [10]. | Flexible polymers used in skin patches, smart textiles, and implantable devices [8] [10]. |
| Triboelectric/Piezoelectric Materials | Harvest biomechanical energy from body movement (walking, breathing) to power devices; enable self-powered systems [10]. | Materials in TENGs/PENGs for powering pacemakers or pulse monitors [10]. |
| Enzyme-Based Biofuel Cell (E-BFC) Components | Utilize biological fuels (glucose, lactate) in biofluids to generate electrical power; can also function as the sensing element itself [10]. | E-BFCs in sweat patches or contact lenses for simultaneous power generation and metabolite sensing [10]. |
The performance of modern multi-parameter platforms can be quantified against key metrics, as summarized in the table below. This data provides a benchmark for researchers evaluating system capabilities.
Table 3: Performance Metrics of Modern Multi-Parameter Sensing Platforms
| Performance Parameter | Representative Value/State-of-the-Art | Context & Application |
|---|---|---|
| Number of Simultaneously Measured Analytes | 3+ (e.g., Vitamin C, Tryptophan, Creatinine) [11] | Multiplexed panel for Long COVID monitoring via a single printed sensor array [11]. |
| Power Source Efficiency | >30% power conversion efficiency (Flexible Perovskite Solar Cells) [10] | Powers sweat sensors or implants; hybrid systems (TENG + SC + E-BFC) improve stability [10]. |
| Data Transmission Method | Wireless (e.g., Bluetooth) [10] [12] | Standard for commercial wearables and research prototypes for real-time data relay [10] [12]. |
| Sensor Lifetime & Stability | "Long-lasting," "highly stable... in biological fluids" [11] | Critical for long-term measurement of biomarkers; enabled by stable materials like NiHCF [11]. |
| Key Analytical Performance Metrics | Continuous, real-time monitoring of "trace levels" of metabolites and nutrients [12] | Enabled by in-situ calibration and advanced signal processing in integrated systems [12]. |
The advancement of wearable biosensors for continuous health monitoring is intrinsically linked to the development of robust, sensitive, and specific sensing modalities. Among the most prominent are electrochemical, optical, and piezoelectric biosensors. These transducers convert a biological recognition event into a quantifiable electrical, optical, or mechanical signal, respectively. The selection of an appropriate sensing modality is paramount for the development of effective wearable monitoring platforms, as it directly influences key performance parameters such as sensitivity, selectivity, power consumption, and integration potential. This document provides detailed application notes and experimental protocols for these three core sensing modalities, framed within the context of their application in continuous, real-time health monitoring for research and drug development.
Core Principles and Comparative Analysis
Biosensors are analytical devices that integrate a biological recognition element (bioreceptor) with a physico-chemical transducer [1]. The bioreceptor—such as an enzyme, antibody, nucleic acid, or whole cell—is responsible for the selective interaction with the target analyte. The transducer then converts this biorecognition event into a measurable signal that is proportionate to the analyte concentration [13].
The table below summarizes the fundamental characteristics, advantages, and challenges of the three primary biosensing modalities in the context of wearable health monitoring.
Table 1: Comparative Analysis of Core Biosensing Modalities for Wearable Applications
| Feature | Electrochemical Biosensors | Optical Biosensors | Piezoelectric Biosensors |
|---|---|---|---|
| Transduction Principle | Measures electrical changes (current, potential, impedance) from biochemical reactions [14]. | Measures changes in light properties (intensity, wavelength, polarization) [15]. | Measures change in mass via mechanical stress-induced electrical signals (e.g., frequency shift) [16]. |
| Common Sub-types | Voltammetric/Amperometric, Impedimetric, Potentiometric, FET-based [14]. | Surface Plasmon Resonance (SPR), Localized SPR, Fluorescence, Interferometric, Colorimetric [15] [13]. | Quartz Crystal Microbalance (QCM), Piezoelectric Cantilevers [16]. |
| Key Advantages | High sensitivity, portability, low cost, low power requirements, suitability for miniaturization [17] [14]. | High sensitivity and specificity, label-free detection, potential for multiplexing [15] [13]. | Label-free, real-time detection, high sensitivity to mass changes, simplicity [16] [18]. |
| Key Challenges for Wearables | Sensor drift, biofouling, calibration in complex matrices [17]. | Integration of optical components, miniaturization, potential for external light interference [15]. | Sensitivity to environmental vibrations, interference from liquid viscosity, integration challenges [16]. |
| Example Wearable Application | Real-time glucose monitoring in interstitial fluid [1]. | Monitoring of biomarkers via colorimetric sweat patches [17]. | Detection of pathogens or biomarkers in liquid samples [18]. |
Experimental Protocols for Wearable Integration
Protocol: Development of a Wearable Electrochemical Biosensor for Lactate Monitoring
Objective: To fabricate and characterize a flexible, amperometric biosensor for continuous lactate monitoring in sweat.
Principle: The enzyme lactate oxidase (LOx) is immobilized on a working electrode. LOx catalyzes the oxidation of lactate, producing hydrogen peroxide (H₂O₂). An applied potential at the working electrode oxidizes H₂O₂, generating a current proportional to the lactate concentration [1] [14].
Materials:
- Substrate: Flexible polyimide or polyethylene terephthalate (PET) sheet.
- Electrodes: Screen-printed carbon (working, counter) and Ag/AgCl (reference) electrodes.
- Bioreceptor: Lactate oxidase (LOx) enzyme.
- Immobilization Matrix: Chitosan or Nafion solution.
- Equipment: Potentiostat, electrochemical cell, data acquisition system.
Procedure:
- Electrode Functionalization: Prepare a solution containing 5 mg/mL LOx in a 1% chitosan solution. Deposit 5 µL of this solution onto the working electrode area and allow it to dry at 4°C for 1 hour.
- Sensor Assembly: Integrate the functionalized electrode into a flexible, microfluidic sweat collection patch designed for epidermal attachment.
- Calibration: Connect the sensor to a portable potentiostat. Perform amperometric measurements (e.g., at +0.6 V vs. Ag/AgCl) in standard lactate solutions (e.g., 0.1 - 20 mM) in 0.1 M PBS, pH 7.4. Record the steady-state current.
- Data Analysis: Plot the calibration curve of current vs. lactate concentration. Determine the sensor's linear range, sensitivity (slope of the linear region), and limit of detection (LOD).
- In-Vitro Validation: Validate sensor performance using artificial sweat matrix to assess interference.
Protocol: Fabrication of an Optical SPR Biosensor for Biomarker Detection
Objective: To implement a Surface Plasmon Resonance (SPR) assay for the label-free, real-time detection of a specific protein biomarker (e.g., cortisol) in a buffer.
Principle: A laser beam is directed onto a gold-coated glass sensor chip, exciting surface plasmons at a specific resonance angle. The immobilization of a capture antibody and subsequent binding of the target analyte to the surface causes a change in the refractive index, leading to a shift in the resonance angle that is monitored in real-time [13].
Materials:
- SPR Instrument: Commercial SPR instrument (e.g., Biacore) or lab-built setup.
- Sensor Chip: Gold-coated glass chip with carboxymethylated dextran matrix.
- Bioreceptors: Monoclonal antibody specific to the target biomarker.
- Reagents: N-hydroxysuccinimide (NHS), N-(3-Dimethylaminopropyl)-N′-ethylcarbodiimide hydrochloride (EDC), ethanolamine hydrochloride.
- Buffers: HBS-EP running buffer (10 mM HEPES, 150 mM NaCl, 3 mM EDTA, 0.005% surfactant P20, pH 7.4).
Procedure:
- Surface Activation: Dock the sensor chip and prime the system with HBS-EP buffer. Inject a 1:1 mixture of 0.4 M EDC and 0.1 M NHS for 7 minutes to activate the carboxyl groups on the dextran matrix.
- Ligand Immobilization: Dilute the capture antibody to 20 µg/mL in 10 mM sodium acetate buffer (pH 5.0). Inject over the activated surface for 10 minutes to achieve covalent immobilization.
- Surface Blocking: Inject 1 M ethanolamine-HCl (pH 8.5) for 7 minutes to deactivate remaining activated esters.
- Binding Assay: Set a continuous flow of HBS-EP buffer. Inject a series of analyte (cortisol) solutions at varying concentrations (e.g., 0, 10, 50, 100 nM) for 3 minutes (association phase), followed by buffer flow for 5 minutes (dissociation phase).
- Data Analysis: Use the instrument's software to subtract signals from a reference flow cell. Fit the resulting sensorgrams to a 1:1 Langmuir binding model to determine the association ((k{on})) and dissociation ((k{off})) rate constants, and the equilibrium dissociation constant ((KD = k{off}/k_{on})).
Protocol: Quartz Crystal Microbalance (QCM) Assay for Pathogen Detection
Objective: To detect a bacterial pathogen (e.g., E. coli) using a QCM piezoelectric biosensor.
Principle: An antibody is immobilized on the gold surface of a quartz crystal. Binding of the bacterial cells to the antibodies increases the mass on the crystal surface, leading to a decrease in its resonant frequency, as described by the Sauerbrey equation [16].
Materials:
- QCM System: QCM instrument with flow cell and frequency oscillator.
- Sensor: AT-cut quartz crystal with gold electrodes.
- Bioreceptor: Anti-E. coli antibody.
- Reagents: 11-Mercaptoundecanoic acid (11-MUA), EDC, NHS.
- Buffers: Phosphate Buffered Saline (PBS), pH 7.4.
Procedure:
- Sensor Surface Functionalization: Incubate the QCM crystal in a 1 mM ethanolic solution of 11-MUA for 24 hours to form a self-assembled monolayer (SAM). Rinse with ethanol and dry under nitrogen.
- Antibody Immobilization: Place the crystal in the QCM flow cell. Flow PBS to establish a stable baseline frequency. Inject a solution of 0.4 M EDC and 0.1 M NHS for 15 minutes to activate the carboxyl groups of the SAM. Inject a solution of anti-E. coli antibody (50 µg/mL in PBS) for 30 minutes, allowing covalent amide bond formation.
- Baseline Stabilization: Flow PBS until a stable frequency is achieved. Record this frequency as the baseline, (F_0).
- Sample Measurement: Inject a series of E. coli suspensions in PBS of known concentrations (e.g., 10³ to 10⁶ CFU/mL) over the sensor surface. Monitor the frequency shift ((\Delta F)) in real-time for each concentration.
- Data Analysis: Use the Sauerbrey equation, (\Delta m = -C \cdot \Delta F / n), where (C) is the sensitivity constant of the crystal and (n) is the overtone number, to calculate the mass bound. Plot (\Delta F) versus E. coli concentration to establish a calibration curve.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Biosensor Development
| Item | Function | Example Use Case |
|---|---|---|
| Enzymes (e.g., Glucose Oxidase, Lactate Oxidase) | Biocatalytic element that reacts specifically with the target analyte to produce a measurable product [1]. | Core recognition element in amperometric biosensors for metabolites. |
| Monoclonal Antibodies | High-specificity biorecognition elements for antigens and protein biomarkers [13]. | Immobilized on SPR chips or QCM crystals for label-free detection of biomarkers or pathogens. |
| N-Hydroxysuccinimide (NHS) / EDC | Cross-linking reagents for activating carboxyl groups to form stable amide bonds with proteins [13]. | Standard chemistry for covalent immobilization of antibodies on sensor surfaces (e.g., gold, dextran). |
| Chitosan / Nafion | Biocompatible polymers used for enzyme immobilization and as permselective membranes to block interferents [1]. | Entrapment of enzymes on electrode surfaces; rejection of negatively charged ascorbic acid in glutamate sensors. |
| Quartz Crystal Microbalance (QCM) Chip | Piezoelectric transducer that oscillates at a fundamental frequency sensitive to surface mass changes [16]. | Mass-sensitive platform for detecting binding of cells, proteins, or DNA. |
| Self-Assembled Monolayer (SAM) Thiols (e.g., 11-MUA) | Molecules that form ordered, stable layers on gold surfaces, providing functional groups for further modification [16]. | Creates a well-defined interface for subsequent bioreceptor immobilization on gold electrodes or QCM crystals. |
Workflow and Signaling Visualizations
Generalized Biosensor Workflow
This diagram illustrates the universal operational principle common to all biosensor modalities, from sample introduction to data output.
Electrochemical Sensing Pathway
This diagram details the specific signaling pathway in an enzymatic amperometric biosensor, such as one used for glucose or lactate detection.
Optical SPR Sensing Principle
This visualization depicts the core optical phenomenon of Surface Plasmon Resonance used for label-free biomolecular interaction analysis.
The development of wearable biosensors for continuous health monitoring represents a paradigm shift from reactive to predictive healthcare. This transition is being powered by breakthroughs in advanced materials science, particularly in the realms of graphene, functional nanomaterials, and flexible substrates. These materials are fundamentally redesigning the interface between biological systems and sensing technologies by providing the critical capabilities of mechanical compatibility with biological tissues, enhanced sensing sensitivity, and unprecedented miniaturization. Where traditional rigid electronics fail due to a mechanical mismatch with soft, dynamic human physiology, these advanced materials enable the creation of biosensing platforms that are conformable, stretchable, and even biodegradable [19] [1]. The integration of these materials is accelerating the advancement of biosensors from research curiosities to clinically viable devices capable of providing continuous, medical-grade physiological data outside clinical settings [20] [1].
The global flexible substrates market, projected to grow from USD 931.3 million in 2025 to USD 3,156.3 million by 2034, reflects the significant commercial investment in these enabling technologies [21]. This growth is driven by increasing demands across consumer electronics, healthcare, and automotive sectors. In healthcare specifically, flexible substrates are crucial for next-generation wearable devices that require durability, portability, and adaptability without compromising electronic performance [21]. This review examines the specific roles of graphene, nanomaterials, and flexible substrates in advanced biosensing platforms, providing detailed application notes and experimental protocols to guide research and development in this rapidly evolving field.
Material Properties and Functional Mechanisms
Property Comparison of Advanced Biosensing Materials
Table 1: Functional properties and biosensing applications of advanced materials.
| Material Category | Key Properties | Primary Roles in Biosensors | Example Applications |
|---|---|---|---|
| Graphene | High electrical/thermal conductivity, large surface area, mechanical strength, flexibility [22] [20] | Transducer element, electrode material, sensing interface [22] | Potentiometric FET dopamine sensing, glucose monitoring [19] |
| Metallic Nanoparticles (Au, Ag) | Localized Surface Plasmon Resonance (LSPR), color tunability, high stability [22] [23] | Signal amplification, optical transduction, "hot spot" generation [22] [23] | SERS substrates for food contaminants, biomarker detection [23] [19] |
| Carbon Nanotubes (CNTs) | Large surface area, high electrical conductivity, shock-bearing ability [22] [24] | Electrode modification, signal enhancement, flexible circuitry [22] | Piezoelectric nanogenerators, wearable pressure sensors [24] |
| Quantum Dots (QDs) | Color tunability, size-dependent optoelectronic properties [22] | Fluorescent tags, optical transduction elements [22] | Multiplexed detection, optical sensing platforms |
| Flexible Plastic Substrates (PET, Polyimide) | Mechanical flexibility, light weight, roll-to-roll process compatibility [25] [19] [21] | Structural support, device encapsulation, conformal interfaces [19] [21] | Flexible displays, skin-worn epidermal sensors [19] [21] |
| Cellulose Paper | Porosity, capillary action, biodegradability, low cost [25] [23] | Fluid transport, sample storage, disposable sensor matrix [25] [23] | Lateral flow assays, SERS substrates, point-of-care diagnostics [25] [23] |
Signaling and Enhancement Mechanisms in Nanomaterial-Enabled Biosensing
Advanced materials enhance biosensor performance through distinct physical mechanisms that amplify the biorecognition event into a measurable signal.
Electrochemical Sensing Mechanisms: Graphene and carbon nanotubes enhance electrochemical biosensors through their exceptional electrical properties. When functionalized with biorecognition elements (e.g., enzymes, antibodies), these materials facilitate efficient electron transfer between the bioreceptor and transducer during analyte binding. This results in enhanced sensitivity for amperometric, potentiometric, and impedimetric measurements [22] [19]. For instance, graphene-based field-effect transistors (FETs) can detect dopamine release from cells by measuring conductance changes with minimal interference when bent to a 3 cm radius, demonstrating both sensitivity and mechanical resilience [19].
Optical Sensing Mechanisms: Metallic nanoparticles, particularly gold and silver, enable highly sensitive optical biosensing through localized surface plasmon resonance (LSPR). When these nanoparticles are irradiated with light at suitable wavelengths, they generate coherent electron oscillations that create intense, localized electromagnetic fields known as "hot spots" [23]. This phenomenon forms the basis for Surface-Enhanced Raman Spectroscopy (SERS), where plasmonic nanostructures can enhance Raman scattering signals by factors up to 10¹¹, enabling single-molecule detection [23]. The controlled creation of nanogaps between nanoparticles is critical for maximizing this enhancement effect [23].
Energy Harvesting Mechanisms: For self-powered wearable systems, nanomaterials enable the conversion of ambient energy from the body or environment into electrical power. Piezoelectric nanogenerators incorporating poly(vinylidene fluoride-co-trifluoroethylene) (P(VDF-TrFe)) nanofibers can transform mechanical energy from pulse waves or joint movements into electrical signals for both sensing and power generation [24]. Similarly, triboelectric nanogenerators (TENGs) can harvest energy from movement through contact-separation processes between nanomaterial-based layers with different electron affinities [24].
Figure 1: Signaling pathways in nanomaterial-enabled biosensors. Biological events are transduced into measurable signals through various enhancement mechanisms unique to nanomaterials.
Application Notes: Advanced Materials in Wearable Biosensors
Graphene in Flexible Electrochemical Sensors
Graphene's two-dimensional structure and exceptional electrical properties make it an ideal material for creating highly sensitive, flexible electrochemical biosensors. Devices incorporating graphene-based field-effect transistors (FETs) have demonstrated the capability to detect physiological concentrations of biomarkers like dopamine directly from cell cultures, while maintaining performance when mechanically deformed [19]. This combination of sensitivity and flexibility enables continuous monitoring of neurochemicals in unconventional, body-compliant form factors. The functionalization of graphene surfaces with specific biorecognition elements (enzymes, antibodies, aptamers) creates selective interfaces for target analytes while maintaining graphene's advantageous electronic properties. Manufacturing approaches include the direct transfer of graphene layers onto flexible substrates like polyimide or polydimethylsiloxane (PDMS), or the creation of graphene-polymer composites that offer both conductivity and stretchability [20] [19].
Nanomaterial-Enabled Optical Biosensing Platforms
Metallic nanoparticles functionalized with biorecognition elements serve as the foundation for highly sensitive optical biosensing platforms. Gold nanoparticles (AuNPs) and silver nanoparticles (AgNPs) exhibit strong localized surface plasmon resonance (LSPR) effects that transduce molecular binding events into measurable colorimetric or scattering signals. These nanoparticles can be incorporated into flexible substrates like cellulose paper to create low-cost, disposable biosensors for point-of-care applications [23]. SERS platforms leveraging nanoparticle "hot spots" have achieved enhancement factors up to 10¹¹, enabling detection of analytes at single-molecule levels [23]. Recent advances include the decoration of cellulose fiber networks with plasmonic nanoparticles, creating flexible SERS substrates that can be conformally applied to irregular surfaces for in-situ analysis [23]. These platforms are particularly valuable for detecting food contaminants, environmental pollutants, and disease biomarkers in resource-limited settings.
Flexible Substrates for Conformal Bio-Interfacing
The selection of appropriate flexible substrates is critical for ensuring reliable performance of wearable biosensors in dynamic, real-world conditions. Plastic polymers like polyethylene terephthalate (PET) and polyimide dominate the flexible substrates market, accounting for 46.2% of the global share, due to their excellent flexibility, lightweight nature, and compatibility with roll-to-roll manufacturing processes [21]. These materials provide mechanical support for electronic components while allowing the device to conform to curved body surfaces like the wrist or forehead. Emerging "epidermal" biosensors take this concept further by utilizing ultra-thin, skin-like substrates that can adhere directly to the epidermis for continuous analysis of biomarkers in sweat or interstitial fluid [1]. Beyond synthetic polymers, cellulose-based papers offer unique advantages including biodegradability, porosity for fluid transport, and extremely low cost, making them ideal for disposable diagnostic applications in resource-constrained settings [25] [23].
Experimental Protocols
Protocol: Impedimetric Viral Detection on Flexible Polyester Films
This protocol describes the capture and detection of viruses (e.g., HIV-1) using antibody-conjugated magnetic beads and impedance spectroscopy detection on a flexible polyester film with embedded electrodes [25].
Materials and Reagents:
- Flexible polyester film with two rail silver electrodes in microfluidic channels
- Magnetic beads (2.8 μm diameter)
- Biotinylated polyclonal anti-gp120 antibodies
- Viral samples (e.g., HIV-1 subtypes A, B, C, D, E, G)
- Control samples (virus-free DPBS)
- Glycerol solution (20% in deionized water)
- Lysis buffer (commercial RIPA buffer or equivalent)
- Biological samples (whole blood, plasma) for spiking experiments
Procedure:
- Bead Conjugation: Incubate magnetic beads with biotinylated anti-gp120 antibodies (1-2 μg per 1 mg beads) in DPBS for 1 hour at room temperature with gentle mixing.
- Virus Capture: Mix antibody-conjugated beads with viral samples (spiked into DPBS, whole blood, or plasma) at a ratio of 1 mg beads per 1 mL sample. Incubate for 2 hours with continuous mixing.
- Washing: Separate beads using a magnetic rack and wash four times with 20% glycerol solution to remove non-specifically bound materials.
- Viral Lysis: Resuspend washed beads in 100 μL lysis buffer and incubate for 15 minutes to release viral contents.
- Impedance Measurement:
- Apply 10 μL of lysate to the electrode area of the polyester film platform.
- Measure impedance magnitude and phase spectra over a frequency range of 100 Hz to 1 MHz.
- Focus analysis on impedance magnitude at 1,000 Hz, where maximum signal-to-noise ratio is observed.
- Data Analysis: Compare impedance magnitude of viral lysate samples to control samples. A significant decrease (13-30%) in impedance magnitude indicates positive detection [25].
Validation Notes:
- Specificity Testing: Include controls with unrelated viruses (e.g., Epstein-Barr virus) to confirm specificity of antibody-virus binding.
- Sample Volume Optimization: For low viral concentrations, increase sample volume up to 5 mL while maintaining the same bead quantity to improve detection sensitivity.
- Clinical Validation: Test with clinically relevant viral loads (10⁶-10⁸ copies/mL) matching acute infection stages.
Figure 2: Workflow for impedimetric viral detection on flexible polyester substrates.
Protocol: Cellulose-Based SERS Substrate Fabrication and Application
This protocol details the fabrication of flexible, cellulose-based substrates for Surface-Enhanced Raman Spectroscopy (SERS) and their application in detecting analytes at trace concentrations [23].
Materials and Reagents:
- Cellulose filter paper or nanocellulose film
- Metal precursors (chloroauric acid for gold, silver nitrate for silver)
- Reducing agents (sodium citrate, sodium borohydride)
- Capping agents (polyvinylpyrrolidone, citrate)
- Analyte solutions (e.g., Rhodamine 6G, pesticides, biomarkers)
- Ethanol and deionized water
- Oxygen plasma cleaner (optional)
Procedure:
- Substrate Pretreatment: Treat cellulose paper with oxygen plasma for 5 minutes (optional) to enhance surface hydrophilicity and nanoparticle adhesion.
- Nanoparticle Synthesis:
- For gold nanoparticles: Heat 0.01% chloroauric acid solution to boiling. Add 1% sodium citrate solution (1:10 v/v) with vigorous stirring. Continue heating until wine-red color develops.
- For silver nanoparticles: Add 2 mL of 0.1 M sodium borohydride to 50 mL of 0.1 mM silver nitrate with stirring. Add 1 mL of 1% sodium citrate as stabilizer.
- Substrate Functionalization:
- Immerse cellulose substrate in nanoparticle solution for 2-24 hours.
- Alternatively, drop-cast concentrated nanoparticle solution onto cellulose and dry at 60°C.
- For enhanced uniformity, use vacuum filtration to deposit nanoparticles onto cellulose membranes.
- Characterization: Verify nanoparticle distribution and density using scanning electron microscopy. Optimize "nanogap" distances between particles (typically 2-10 nm) for maximum SERS enhancement.
- SERS Measurement:
- Apply 2-5 μL of analyte solution to functionalized substrate and allow to dry.
- Acquire Raman spectra using appropriate laser wavelength (typically 532 nm or 785 nm).
- Focus laser on areas with high nanoparticle density ("hot spots").
- Enhancement Factor Calculation:
- Calculate Enhancement Factor (EF) using formula: EF = (ISERS / IRaman) × (NRaman / NSERS)
- Where ISERS and IRaman are SERS and normal Raman intensities, and NSERS and NRaman are number of molecules probed.
Technical Notes:
- Nanoparticle size control: Adjust metal-to-reductant ratio to control nanoparticle size (typically 20-80 nm for optimal SERS).
- Homogeneity: Use slow immersion method (24 hours) for more uniform nanoparticle distribution compared to drop-casting.
- Stability: Store functionalized substrates in vacuum desiccator to prevent nanoparticle oxidation.
- Calibration: Use Rhodamine 6G (10⁻⁶ to 10⁻⁹ M) as standard for EF calculation and performance validation.
Protocol: Self-Powered Wearable Sensor Integration
This protocol describes the integration of energy harvesting nanomaterials with biosensors to create self-powered wearable systems for continuous health monitoring [24].
Materials and Reagents:
- Piezoelectric polymer (P(VDF-TrFE) solution)
- Conductive electrodes (Ag nanowires, graphene ink)
- Flexible substrate (PDMS, PET, or polyimide)
- Encapsulation material (Ecoflex, PDMS)
- Biosensing element (enzyme, antibody, according to application)
- Connecting wires/silver epoxy
Procedure:
- Nanogenerator Fabrication:
- Spin-coat P(VDF-TrFE) solution onto flexible substrate at 2000 rpm for 60 seconds.
- Anneal at 120°C for 2 hours to enhance piezoelectric β-phase crystallization.
- Deposit top and bottom electrodes using Ag nanowire networks or graphene ink.
- Poling: Apply electric field (50-100 MV/m) at 80°C for 1 hour to align dipole moments.
- Sensor Integration:
- Fabricate biosensor component (e.g., electrochemical sensor, strain sensor) adjacent to nanogenerator on same substrate.
- Connect nanogenerator output to sensor circuitry using stretchable interconnects.
- System Encapsulation:
- Encapsulate entire device in thin layer of PDMS or Ecoflex (100-500 μm thickness) using spin-coating or lamination.
- Ensure encapsulation maintains flexibility while protecting from moisture and mechanical damage.
- Performance Validation:
- Test energy output by applying simulated body movements (flexion, compression).
- Measure open-circuit voltage and short-circuit current using oscilloscope.
- Verify sensor functionality when powered solely by nanogenerator.
- On-Body Testing:
- Mount device on joint (wrist, knee) or chest for real-world performance assessment.
- Monitor continuous operation duration and power management efficiency.
Optimization Guidelines:
- Energy Output: Incorporate high-aspect ratio nanomaterials (ZnO nanowires, BaTiO₃ nanoparticles) into polymer matrix to enhance piezoelectric coefficient.
- Flexibility: Use porous or fiber-based electrode structures to maintain conductivity during stretching.
- Biocompatibility: Select encapsulation materials with demonstrated skin compatibility for long-term wear.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key research reagents and materials for developing advanced biosensing platforms.
| Category/Item | Specific Examples | Research Function | Application Notes |
|---|---|---|---|
| Flexible Substrates | PET, Polyimide, PDMS, cellulose paper [25] [19] [21] | Structural support enabling bendable, conformal devices | Plastic films dominate market (46.2%); paper offers biodegradability [21] |
| Conductive Nanomaterials | Graphene, CNTs, Ag nanowires [22] [20] [24] | Electrodes, interconnects, transducer elements | Provide conductivity while maintaining flexibility under deformation |
| Plasmonic Nanoparticles | Gold nanospheres, silver nanocubes, Au-Ag core-shell [22] [23] | LSPR generation for optical sensing, SERS "hot spots" | Control nanogap (2-10 nm) for maximum field enhancement [23] |
| Biorecognition Elements | Anti-gp120 antibodies, glucose oxidase, DNA aptamers [25] [22] [1] | Selective target capture and molecular recognition | Stability on flexible/nanomaterial surfaces requires optimization |
| Energy Harvesting Materials | P(VDF-TrFE), BTO-PDMS composites, triboelectric layers [24] | Self-powering from body movement, thermal gradients | Piezoelectric polymers require poling for optimal performance |
| Encapsulation Materials | Ecoflex, PDMS, parylene, polyurethane [19] [1] | Environmental protection, biocompatibility, device integrity | Must balance barrier properties with mechanical flexibility |
The integration of graphene, nanomaterials, and flexible substrates is fundamentally transforming the capabilities of wearable biosensors for continuous health monitoring. These advanced materials enable the creation of devices that successfully overcome the historical limitations of conventional rigid electronics, providing unprecedented mechanical compatibility with biological systems while enhancing sensing performance through unique physical and chemical properties. As research advances, several key challenges and opportunities are emerging that will shape the future development of these technologies.
Future progress will likely focus on enhancing the multifunctionality of these materials systems, creating platforms capable of simultaneously monitoring multiple biomarkers with high specificity and sensitivity. The development of robust self-powering systems through advanced energy harvesting nanomaterials will be critical for achieving truly autonomous operation [24]. Additionally, the transition from proof-of-concept demonstrations to clinically validated tools requires extensive large population studies to establish correlations between biomarker concentrations in easily accessible biofluids (sweat, tears) and blood chemistry [1]. As these technologies mature, interdisciplinary collaboration between materials scientists, engineers, and clinical researchers will be essential to address complex challenges in biocompatibility, signal stability, and manufacturing scalability. With continued advancement, biosensing platforms leveraging these advanced materials have the potential to revolutionize personal healthcare by providing continuous, real-time physiological information that enables truly predictive and personalized medicine.
The advancement of wearable biosensors for continuous health monitoring is fundamentally driven by the convergence of three core enabling technologies: microfluidics, wireless communication, and energy harvesting. These technologies synergistically address the critical challenges of miniaturization, real-time data accessibility, and power autonomy, which are essential for practical, user-friendly biosensing systems. Microfluidic components enable the precise manipulation of minute biofluid samples, such as sweat, tears, or interstitial fluid, directly at the wearer's skin [26] [1]. Wireless communication modules facilitate the seamless transmission of captured physiological data to external devices like smartphones or cloud platforms, enabling real-time analytics and remote patient monitoring [27]. Furthermore, energy harvesting systems provide sustainable power by converting ambient energy from the user's environment or body into electrical energy, thereby reducing or eliminating reliance on traditional batteries and enhancing device longevity [28] [27]. This integration is paving the way for a new generation of autonomous, "lab-on-a-chip" wearable platforms that promise to revolutionize personalized healthcare and continuous physiological monitoring [26] [29].
Technology-Specific Application Notes & Protocols
Microfluidics for Wearable Biosensors
Application Note AN-MF001: On-Body Biofluid Handling and Analysis Microfluidic systems in wearable biosensors are designed for the autonomous sampling, transport, and analysis of epidermal biofluids like sweat. These systems utilize networks of microscale channels, pumps, and valves fabricated from flexible polymers to ensure conformal contact with the curved and dynamic surface of human skin. A critical function is the continuous wicking of freshly secreted sweat to sensing chambers while preventing the accumulation of stale sample, which is achieved through sophisticated channel design and capillary action [26] [1]. The primary challenge is maintaining consistent and reproducible sample transport over extended wear periods, as variations in sweat rate and skin topography can affect sensor performance.
Protocol PR-MF001: Fabrication of a PDMS-Substrate Microfluidic Chip for Sweat Sampling
- Objective: To fabricate a flexible, skin-adherent polydimethylsiloxane (PDMS) microfluidic chip for continuous sweat collection and routing to electrochemical sensor electrodes.
Materials:
- SYLGARD 184 Silicone Elastomer Kit (Dow DuPont)
- SU-8 photoresist and SU-8 developer
- Silicon wafer (4-inch)
- Plasma surface treater
- Oven
- Acetone and Isopropyl Alcohol (IPA)
- Laser printer and transparency film or high-resolution photomask
Procedure:
- Master Mold Fabrication: a. Clean the silicon wafer sequentially with acetone, IPA, and deionized water; dry with nitrogen. b. Spin-coat SU-8 photoresist onto the wafer to achieve a thickness of 100 µm. c. Soft-bake the wafer according to the SU-8 datasheet. d. Expose the photoresist to UV light through a photomask defining the microchannel design. e. Perform a post-exposure bake. f. Develop the wafer in SU-8 developer to reveal the relief structure of the channels. g. Hard-bake the master mold at 150°C for 10 minutes to improve robustness.
- PDMS Chip Casting: a. Mix the PDMS base and curing agent in a 10:1 weight ratio. Degas the mixture in a desiccator until no bubbles remain. b. Pour the PDMS mixture over the master mold placed in a Petri dish. c. Degas again to remove any bubbles introduced during pouring. d. Cure the PDMS in an oven at 65°C for 4 hours. e. Carefully peel the cured PDMS slab, containing the negative imprint of the channels, from the master mold.
- Bonding and Integration: a. Cut the PDMS slab to size and create fluidic inlet/outlet ports using a biopsy punch. b. Treat the PDMS surface and a pre-fabricated sensor substrate (e.g., with screen-printed electrodes) with oxygen plasma for 45 seconds. c. Immediately bring the activated surfaces into contact to form an irreversible seal. d. Post-bake the assembled device at 80°C for 30 minutes to strengthen the bond.
Validation: Verify channel integrity and flow by introducing a colored dye (e.g., food dye) at the inlet and observing its capillary-driven progression through the network to the outlet/sensor zone.
Wireless Communication for Data Transmission
Application Note AN-WC001: Low-Power Telemetry for Physiological Data Wireless communication is indispensable for transforming a wearable sensor into a node in a connected health ecosystem. For wearables, the selection of a wireless technology involves a critical trade-off between data rate, range, and power consumption. Bluetooth Low Energy (BLE) is predominantly favored for consumer wearables due to its low power profile and universal compatibility with smartphones [27]. For applications requiring longer range or operation in challenging environments, protocols like LoRaWAN or Zigbee are employed. A key design principle is the implementation of duty cycling, where the radio is powered on only during data transmission bursts to minimize average power consumption [28].
Protocol PR-WC001: Integration of BLE for Real-Time Data Streaming from a Biosensor Patch
- Objective: To integrate a BLE module with a microcontroller and biosensor to enable wireless streaming of physiological data (e.g., glucose concentration) to a mobile device.
Materials:
- BLE SoC (System-on-Chip), e.g., Nordic Semiconductor nRF52840
- Microfluidic biosensor patch with analog signal output
- Stable power source (e.g., 3.3V button cell battery or embedded energy harvester)
- JTAG/SWD programmer and associated software
- Mobile phone with custom-developed or generic BLE terminal application.
Procedure:
- Hardware Interfacing: a. Connect the analog output pin of the biosensor's potentiostat to an ADC (Analog-to-Digital Converter) input pin on the BLE SoC. b. Establish common ground between the biosensor, SoC, and power supply. c. Ensure stable 3.3V power is supplied to all active components.
- Firmware Development: a. Develop firmware (e.g., in C/C++ using the nRF5 SDK) to initialize the SoC's ADC at a specified sampling rate (e.g., 1 Hz). b. Program the ADC to read the sensor's voltage, which is proportional to the analyte concentration. c. Implement the BLE stack and define a custom GATT (Generic Attribute) service with a characteristic to hold the sensor data. d. Configure the device to advertise itself with a recognizable name and to allow connections from a central device (smartphone). e. Write the digitized and processed sensor reading to the GATT characteristic at the defined sampling interval.
- Mobile Application & Data Logging: a. On the mobile side, develop an app (e.g., using Android's BLE API) that scans for and connects to the sensor's unique BLE address. b. Upon connection, the app should discover services and subscribe to notifications for the data characteristic. c. Implement a data parser to convert the incoming byte stream into numerical values and display them in real-time on the phone's screen. d. Incorporate functionality to log the time-stamped data to a local file or transmit it to a cloud database.
Validation: Measure the current draw of the system during advertising, connected, and sleep states using a precision multimeter to ensure it meets power budget constraints.
Energy Harvesting for System Autonomy
Application Note AN-EH001: Ambient Energy Scavenging for Wearables Energy harvesting technologies liberate wearable biosensors from the limitations of battery capacity by converting ambient energy into electricity. Common strategies include the use of flexible photovoltaic cells to harvest light, thermoelectric generators (TEGs) to convert body heat, and piezoelectric or triboelectric devices to capture energy from body movement [28] [27]. A critical component of any energy harvesting system is the Power Management Unit (PMU), which performs maximum power point tracking (MPPT), regulates the variable harvested power, and manages the charging of a small buffer battery or supercapacitor to handle peak power demands beyond the harvester's continuous output [28].
Protocol PR-EH001: System Integration of a Solar Energy Harvester with a Supercapacitor Buffer
- Objective: To power a wearable biosensor patch by integrating a flexible solar cell with a PMU and a supercapacitor for energy storage.
Materials:
- Flexible amorphous silicon solar cell (e.g., 5V, 10mA under indoor light)
- Power Management IC (PMIC), e.g., BQ25570 from Texas Instruments
- Low-leakage 1 F supercapacitor
- Wearable biosensor platform (load)
- Oscilloscope, multimeter, variable light source.
Procedure:
- Characterization of the Harvester: a. Place the solar cell under a calibrated light source simulating indoor (200 lux) and outdoor (10,000 lux) conditions. b. Using a variable resistor as an electronic load, perform a current-voltage (I-V) sweep to determine the open-circuit voltage (VOC), short-circuit current (ISC), and maximum power point (MPP) for each condition.
- PMU and Storage Integration: a. Solder the solar cell's output to the "VIN" pins of the BQ25570 PMIC evaluation board. b. Connect the 1 F supercapacitor to the "VBAT" pins of the PMIC for energy storage. c. Connect the output of the PMIC ("VOUT") to the power input rail of the biosensor platform. d. Configure the PMIC's resistor settings according to the datasheet to set the MPPT voltage (based on step 1b) and the desired output voltage (e.g., 3.3V).
- System-Level Validation: a. Place the entire system under a light source and monitor the supercapacitor voltage with an oscilloscope to observe the charging profile. b. Once the supercapacitor is charged to the PMIC's turn-on voltage, verify that the biosensor platform powers up and begins normal operation (sensing and wireless transmission). c. Characterize the system's operational lifetime by measuring the time it takes for the supercapacitor to discharge from its maximum voltage to the PMIC's undervoltage lockout threshold under a continuous load.
Validation: The system is validated if it can sustain continuous operation of the biosensor (including its highest power state, e.g., wireless transmission) for a target duration under a defined, cyclic illumination profile (e.g., 12 hours of 200 lux light / 12 hours dark).
Integrated System Workflow
The seamless operation of an advanced wearable biosensor relies on the orchestrated interaction of microfluidics, sensing, energy management, and wireless communication. The following diagram illustrates the logical workflow and data flow from sample collection to user feedback.
Diagram Title: Wearable Biosensor System Workflow
Quantitative Technology Comparison
The selection of appropriate technologies for a wearable biosensor depends on specific application requirements. The tables below summarize key performance metrics and parameters for the discussed enabling technologies.
Table 1: Comparison of Wireless Communication Technologies for Wearable Biosensors
| Technology | Typical Data Rate | Range | Power Consumption | Primary Use Case in Biosensors |
|---|---|---|---|---|
| Bluetooth Low Energy (BLE) | 1-2 Mbps | Short (10-100m) | Very Low | Streaming to smartphone, frequent data updates [27] |
| Near-Field Communication (NFC) | 100-400 kbps | Very Short (<0.2m) | Zero (Powered by Reader) | Patch interrogation, single-read events [27] |
| LoRaWAN | 0.3-50 kbps | Long (2-15 km) | Low | Remote area monitoring, infrequent transmissions [28] |
| Zigbee | 250 kbps | Short (10-100m) | Low | Body area networks, multi-sensor systems [28] |
Table 2: Comparison of Energy Harvesting Modalities for Wearables
| Technology | Typical Power Density | Constraints | Best Suited Application Context |
|---|---|---|---|
| Photovoltaic (Indoor) | 10-100 µW/cm² | Light availability, surface area | Wristwear, headbands [28] [27] |
| Thermoelectric (Body Heat) | 20-60 µW/cm² | Small skin-air ΔT, thermal resistance | Chest patches, tight-fitting bodywear [27] |
| Piezoelectric (Motion) | ~10 µW/cm³ | Dependent on user activity level | Footwear, joint-mounted sensors [27] |
| RF Energy Harvesting | ~0.1 µW/cm² | Very low power, distance from source | Supplementing other sources, passive sensors [28] |
Table 3: Key Market Growth Metrics for Biosensor Technologies (2025-2030)
| Metric | Projected Value / CAGR | Note |
|---|---|---|
| Global Biosensors Market (2030) | USD 54.37 Billion | Projected value [30] |
| Market CAGR (2025-2030) | 9.5% | Compound Annual Growth Rate [30] [31] |
| Wearable Biosensors Segment | Highest Growth CAGR | Within the biosensor product market [30] [31] |
| Optical Biosensor Technology | Highest Growth CAGR | Within biosensor technology segments [30] [31] |
The Scientist's Toolkit: Research Reagent & Material Solutions
Table 4: Essential Materials and Reagents for Wearable Biosensor Development
| Item | Function / Application | Specific Example(s) |
|---|---|---|
| PDMS (Polydimethylsiloxane) | Flexible, biocompatible substrate for microfluidic channels and sensor encapsulation [26] [1] | SYLGARD 184 (Dow DuPont) |
| SU-8 Photoresist | Epoxy-based negative photoresist for creating high-aspect-ratio master molds for soft lithography [26] | SU-8 2050, SU-8 3050 (Kayaku) |
| Screen-Printed Electrodes (SPEs) | Low-cost, mass-producible electrochemical sensor platforms. | Carbon, Ag/AgCl, Gold working electrodes |
| Enzymatic Bioreceptors | Provide high specificity for target analytes (e.g., metabolites) in catalytic biosensors [1] | Glucose Oxidase (for glucose), Lactate Oxidase (for lactate) |
| Aptamers | Synthetic nucleic acid-based bioreceptors for affinity-based sensing of proteins, hormones, etc. [26] [1] | Custom-selected sequences for targets like cortisol or thrombin |
| Ion-Selective Membranes | Enable potentiometric detection of specific electrolytes in biofluids [27] | Valinomycin membrane (for K⁺), TRIEN membrane (for Na⁺) |
| PEDOT:PSS | Conductive polymer used for ion-to-electron transduction, enhancing stability of solid-contact ion-selective electrodes [27] | Clevios PH1000 |
| Nafion | Cation-exchange polymer membrane used to mitigate biofouling and interferent effects in electrochemical sensors [1] | Nafion perfluorinated resin solution |
From Lab to Life: Advanced Applications in Therapeutics and Remote Patient Monitoring
Therapeutic Drug Monitoring (TDM) is undergoing a transformative shift from intermittent, invasive blood draws to continuous, real-time measurement enabled by advances in wearable and implantable biosensor technology. These devices leverage synthetic biology, electrochemical sensing, and intelligent data processing to provide unprecedented insight into pharmacokinetic profiles, enabling truly personalized medicine [32] [33]. This paradigm is particularly impactful for drugs with narrow therapeutic windows, such as anti-Parkinson's agents, antibiotics, and analgesics. This document provides detailed application notes and experimental protocols for implementing these advanced biosensing systems in a research and development context, framed within the broader thesis of wearable biosensors for continuous health monitoring.
Technological Foundations of Continuous TDM
The core of modern TDM lies in biosensors that can operate continuously in situ. A leading example is the SENSBIT (Stable Electrochemical Nanostructured Sensor for Blood In situ Tracking) platform, a microfabricated soft needle that can monitor drug concentrations in flowing blood for up to seven days [32]. This represents a dramatic improvement over previous devices that failed after approximately 11 hours.
Core Sensing Mechanism: The SENSBIT sensor utilizes synthetic antibodies called aptamers that function as molecular switches. Upon encountering a target drug molecule, the aptamer changes its three-dimensional conformation. This structural change generates a measurable electrochemical signal, allowing for precise quantification of the target analyte [32]. The modular design of this technology means it can be adapted to monitor a wide range of therapeutics, from small-molecule antibiotics to complex biologics [32].
Quantitative Performance Data of Featured Platforms
The following tables summarize the key performance metrics and application parameters for the featured TDM technologies, providing a basis for experimental selection and design.
Table 1: Performance Metrics of Representative Biosensors for TDM
| Sensor Platform | Target Analytic | Monitoring Duration | Key Performance Metric | Signal Retention |
|---|---|---|---|---|
| SENSBIT (Implantable) [32] | Kanamycin (Antibiotic) | Up to 7 days | Continuous, real-time data in flowing blood | >70% after 1 month in human serum |
| ACM Wrist Device (Wearable) [34] | Motor symptoms, Sleep, Autonomic function (Parkinson's) | 7 consecutive days | Multidimensional circadian rhythms (A/T Ratio) | N/A (Continuous data stream) |
| ePatch (Wearable) [33] | Heart rhythm (Adverse drug event detection) | >24 hours (Extended) | Wireless ECG data transmission | N/A (Continuous data stream) |
Table 2: Application Parameters for Different Drug Classes
| Drug Class | Example Drug | TDM Need | Compatible Sensor Type | Key Measured Parameter |
|---|---|---|---|---|
| Aminoglycoside Antibiotics | Kanamycin | Narrow therapeutic window [32] | Implantable (e.g., SENSBIT) | Real-time plasma concentration [32] |
| Anti-Parkinson's Agents | Levodopa | Pulsatile dosing; motor fluctuation management [34] | Wearable (e.g., ACM) | Acceleration, Time in Movement, A/T Ratio [34] |
| Analgesics | (To be selected) | Toxicity risk with chronic use | Implantable / Wearable (Platform) | Real-time plasma concentration |
Experimental Protocols for Real-Time TDM
Protocol: Continuous Monitoring of Antibiotics via Implantable Aptamer-Based Sensor
This protocol details the methodology for tracking antibiotic concentrations, such as kanamycin, using an implantable electrochemical sensor [32].
I. Sensor Preparation and Calibration
- Materials: SENSBIT sensor array, target drug (e.g., Kanamycin), artificial serum, potentiostat.
- Procedure:
- Pre-conditioning: Immerse the sensor in a buffer solution (e.g., PBS, pH 7.4) for 30 minutes to stabilize the electrochemical baseline.
- Calibration Curve: Expose the sensor to a series of standard solutions with known concentrations of the target antibiotic (e.g., 0.1 µg/mL to 100 µg/mL) in artificial serum.
- Signal Measurement: Record the electrochemical response (e.g., change in impedance or current) for each standard concentration using a potentiostat.
- Model Fitting: Plot the signal response against concentration to generate a linear calibration model for quantifying unknown samples.
II. In Vivo Monitoring and Data Acquisition
- Materials: Animal model (e.g., rat), surgical suite, infusion pump, data acquisition system.
- Procedure:
- Sensor Implantation: Aseptically implant the calibrated SENSBIT sensor into a target blood vessel (e.g., jugular vein).
- Drug Administration: Administer a bolus dose or initiate a continuous infusion of the antibiotic.
- Continuous Data Collection: Record the electrochemical signal from the sensor continuously at a predefined sampling rate (e.g., 1 Hz) for the duration of the experiment (up to 7 days).
- Data Correlation: Periodically collect and analyze micro-volume blood samples via a separate catheter to validate sensor readings against a gold-standard method (e.g., LC-MS).
Protocol: Multidimensional Monitoring of Anti-Parkinson's Therapy via Wearable Biosensor
This protocol uses a wrist-worn ambulatory circadian monitoring (ACM) device to track the functional effects and circadian disruption associated with anti-Parkinson's drugs like levodopa [34].
I. Device Initialization and Patient Setup
- Materials: ACM device (e.g., Kronowise), base station software, patient logs.
- Procedure:
- Device Configuration: Initialize the ACM device to record motor acceleration, wrist temperature, body position, and light exposure. Set the sampling frequency (e.g., acceleration at 10 Hz, temperature at 1/60 Hz) [34].
- Device Placement: Secure the device on the patient's less-affected wrist (for Parkinson's patients) or non-dominant wrist (for controls) to minimize motion artifacts from intentional activity.
- Baseline Recording: Instruct the patient to wear the device for 24 hours prior to any specific drug challenge to establish a baseline.
II. Data Acquisition and Analysis During Drug Therapy
- Procedure:
- Continuous Monitoring: Patients wear the device for a minimum of 7 consecutive days under free-living conditions while maintaining their standard levodopa regimen.
- Event Logging: Patients use an electronic event marker on the device or a paper diary to record the timing of drug doses, meals, sleep periods, and notable motor symptoms (e.g., "on"/"off" states).
- Data Processing:
- Motor Activity: Calculate the mean acceleration during daytime hours (e.g., 10:00-20:00) as an indicator of bradykinesia.
- Sleep Quality: Calculate the "Time in Movement" during sleep periods as an indicator of sleep fragmentation.
- A/T Ratio: Compute the ratio of daytime Acceleration to sleep-Time-in-movement. A lower A/T ratio indicates greater motor impairment and sleep disruption, a key indicator of suboptimal therapy [34].
- Circadian Rhythm Analysis: Analyze the wrist temperature rhythm to assess autonomic function and overall circadian integrity.
Visualization of Sensing Mechanism and Workflow
The following diagrams, created using the specified color palette, illustrate the core concepts and experimental workflows.
Aptamer-based Drug Sensing Mechanism
Experimental TDM Workflow for Drug Development
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Continuous TDM Research
| Item | Function / Application | Example / Specification |
|---|---|---|
| Synthetic Aptamers | Molecular recognition element for specific drug binding. | DNA/RNA aptamers selected via SELEX; specific for target analyte (e.g., Kanamycin) [32]. |
| Ambulatory Circadian Monitoring (ACM) Device | Wearable multisensor for tracking motor, sleep, and autonomic rhythms. | Records wrist temperature, triaxial acceleration, body position, light exposure over 7+ days [34]. |
| Potentiostat/Galvanostat | Measures electrochemical signals (current, impedance) from implantable sensors. | Required for in vitro calibration and in vivo signal acquisition from electrochemical sensors like SENSBIT [32]. |
| Artificial Serum | Matrix for in vitro sensor calibration and stability testing. | Mimics the ionic and protein composition of human blood; used for calibration curve generation [32]. |
| Levodopa Equivalent Dose (LED) Calculator | Standardizes the dosage of various Parkinson's medications for comparative analysis. | Critical for correlating wearable sensor data (A/T ratio) with total dopaminergic load in clinical studies [34]. |
| Machine Learning Classifiers (e.g., SVM) | For intelligent biosignal processing and feature classification from wearables. | Used to classify biosignals (e.g., EEG, gait) with high accuracy; enables automated analysis [35] [36]. |
Implementation Considerations in Research
The successful deployment of these technologies requires attention to several practical aspects:
- Power Management: For long-term wearability, power is a primary bottleneck. Research is exploring RF power transfer, biofuel cells using sweat, and piezoelectric energy harvesting to enable truly continuous operation [37].
- Biocompatibility: Implantable sensors require materials that are both biocompatible and biofouling-resistant to ensure signal stability over time. Soft, flexible mechanics are also critical for user compliance and tissue integration [37].
- Data Integration and Security: The continuous data streams from these devices must be integrated with electronic health records (EHRs) using standardized formats like HL7. Ensuring data security and patient privacy is paramount, especially when using cloud-based platforms [38].
- Clinical Validation: Sensor readings must be rigorously validated against gold-standard methods (e.g., LC-MS for drug levels, polysomnography for sleep) in the target patient population to establish clinical credibility [34] [33].
The advent of wearable biosensors is revolutionizing modern healthcare by enabling the continuous, non-invasive monitoring of physiological status through the analysis of various biofluids [39] [40]. These devices proficiently assess biomarkers in body fluids like sweat, saliva, tears, and interstitial fluid (ISF), providing significant benefits for illness detection and personalized healthcare [39]. This shift towards peripheral biochemical monitoring represents a paradigm change from intermittent blood testing to a more dynamic, real-time understanding of an individual's health [41]. The core objective of most non-invasive monitoring is to obtain measurements that serve as reliable surrogates for circulating analyte concentrations in blood, thus avoiding the need for frequent invasive blood draws [41]. This document provides a detailed technical overview of the key characteristics of these biofluids, standardized protocols for their collection and analysis, and the essential tools required for research in this rapidly advancing field, all framed within the context of developing robust wearable biosensing platforms.
Biofluid Characteristics & Comparative Analysis
The selection of an appropriate biofluid for a given monitoring application depends on a complex interplay of factors, including the target biomarker's concentration, the physiology of biofluid secretion, and the technical requirements for sensor design [41]. The biofluid itself often presents the greatest challenge, with considerations for sample volumes, secretion rates, variable composition, and potential confounding factors [41]. The table below provides a quantitative comparison of the four primary biofluids used in non-invasive monitoring.
Table 1: Comparative Analysis of Key Biofluids for Non-Invasive Monitoring
| Parameter | Sweat | Saliva | Tears | Interstitial Fluid (ISF) |
|---|---|---|---|---|
| Primary Biomarkers | Electrolytes (Na⁺, K⁺, Cl⁻), lactate, glucose, cortisol, ethanol [41] | Glucose, cortisol, lactate, cytokines, steroid hormones, antibodies, oral disease markers [41] | Glucose, electrolytes, proteins (lysozyme), lactoferrin, cytokines, drugs [40] | Glucose, lactate, hormones, therapeutic drugs [41] |
| Typical Sample Volume | 1 - 50 µL (patch collection) [41] | 50 - 1000 µL (passive drool) | 1 - 10 µL (capillary tube) | 1 - 10 µL (microneedle extraction) [41] |
| Secretion Rate & Stimulation | 1 - 10 nL/min/gland (resting); requires iontophoresis (e.g., pilocarpine) for continuous access [41] | 0.5 mL/min (resting); stimulated by chewing or citric acid [41] | 0.5 - 2.2 µL/min (basal); stimulated by mechanical or chemical irritation | Passive diffusion from capillaries; accessed via microneedles or suction blister [41] |
| pH Range | 4.0 - 6.8 [41] | 6.2 - 7.4 [41] | ~7.4 | ~7.4 [41] |
| Key Advantages | Continuous access via stimulated secretion, relatively large volume | Ease of non-stimulated collection, rich in biomarkers | Direct correlation with some blood constituents (e.g., glucose) | Close correlation with blood plasma for many analytes [41] |
| Key Challenges | Variable salinity, analyte dilution, contamination, low analyte concentration for some markers [41] | Variable viscosity, contamination from food/drink, bacterial breakdown of analytes [41] | Very low sample volume, reflex secretion complicates collection | Requires minimally invasive techniques for access; physiological lag for some analytes [41] |
Experimental Protocols for Biofluid Analysis
Sweat Analysis Protocol: Lactate and Electrolyte Monitoring
This protocol details the collection and analysis of induced sweat for metabolic and electrolyte status assessment, suitable for integration into wearable sweat-sensing patches [41].
1. Reagents and Materials:
- Pilocarpine nitrate solution (1-2%) for iontophoresis
- Sodium chloride (0.9% w/v) for electrode contact
- Deionized water and ethanol for skin cleaning
- Lactate assay kit (enzymatic-amperometric)
- Ion-selective membranes for Na⁺ and K⁺
- Absorbent patches or microfluidic collection device
- Iontophoresis system and Ag/AgCl electrodes
2. Sample Collection Procedure: 1. Skin Preparation: Clean the volar forearm or upper back skin site sequentially with deionized water, 70% ethanol, and again with deionized water. Dry thoroughly with a lint-free cloth. 2. Sweat Stimulation: Assemble the iontophoresis system. Soak the anode electrode in a pilocarpine nitrate solution and the cathode in sodium chloride solution. Apply both to the prepared skin site and deliver a controlled current of 0.2-0.5 mA/cm² for 5 minutes. 3. Sweat Collection: Remove the electrodes. Immediately place a pre-weighed absorbent patch or a soft microfluidic device directly over the stimulated area. Secure the edges with a hypoallergenic medical adhesive. 4. Collection Period: Allow sweat to accumulate for a defined period, typically 15-30 minutes. Note the start and end times. 5. Termination and Storage: Remove the patch/device and seal it in an airtight container to prevent evaporation. Weigh the container to determine the total sweat volume collected (assuming sweat density of 1 g/mL). If not analyzed immediately, store at -80°C.
3. Analytical Procedure: 1. Lactate Measurement (Enzymatic-Amperometric): * For integrated biosensors, the collection patch interfaces directly with a sensor cell containing lactate oxidase enzyme. * The enzymatic reaction produces H₂O₂, which is oxidized at a working electrode (e.g., Pt) held at +0.6V vs. Ag/AgCl reference. * Record the steady-state current, which is proportional to the lactate concentration. Calibrate with standard lactate solutions. 2. Electrolyte Measurement (Potentiometric): * Interface the sweat sample with ion-selective electrodes (ISEs) for Na⁺ and K⁺. * Measure the potential difference between the ISE and a reference electrode. * Determine concentration from a calibration curve constructed using standard solutions.
Saliva Analysis Protocol: Cortisol and Glucose Detection
This protocol describes the collection and analysis of unstimulated whole saliva for biomarkers of stress (cortisol) and metabolic status (glucose) [41].
1. Reagents and Materials:
- Saliva collection aid (e.g., Salivette tube with neutral cotton swab)
- Protease and amylase inhibitors
- Phosphate Buffered Saline (PBS), pH 7.4
- Cortisol Enzyme-Linked Immunosorbent Assay (ELISA) Kit
- Glucose Oxidase reagent kit
- Centrifuge and microcentrifuge tubes
- Spectrophotometer or microplate reader
2. Sample Collection and Pre-processing: 1. Subject Preparation: The subject should not eat, drink, or brush teeth for at least 60 minutes prior to collection. Rinse mouth with water 10 minutes before collection. 2. Unstimulated Collection: Place a neutral cotton swab in the mouth and allow it to passively saturate with saliva for 2-5 minutes without chewing. Avoid stimulating saliva flow. 3. Sample Handling: Place the saturated swab into the insert of a Salivette tube. Centrifuge at 1000 × g for 5 minutes to separate the saliva from the swab into the bottom of the tube. 4. Clarification and Stabilization: Centrifuge the raw saliva at 10,000 × g for 10 minutes at 4°C to pellet debris. Transfer the clear supernatant to a new tube. Add protease inhibitors as per manufacturer's instructions. Aliquot and store at -80°C for long-term storage.
3. Analytical Procedure: 1. Cortisol Analysis (ELISA): * Follow the specific protocol of the commercial high-sensitivity salivary cortisol ELISA kit. * Briefly, add standards and samples to antibody-coated wells. Incubate, then add enzyme conjugate (e.g., cortisol-horseradish peroxidase). Incubate and wash. * Add substrate solution (e.g., TMB) and incubate in the dark. Stop the reaction with stop solution. * Measure the absorbance at 450 nm. Calculate cortisol concentrations from the standard curve. 2. Glucose Analysis (Enzymatic-Colorimetric): * Use a glucose oxidase/peroxidase (GOD-POD) based reagent kit. * Mix saliva sample (or standard) with the working reagent. * Incubate at 37°C for 15-30 minutes. The reaction produces a colored quinoneimine dye. * Measure the absorbance at 490-520 nm. Determine glucose concentration from the standard curve.
Experimental Workflow and Signaling Visualization
The following diagrams, generated using Graphviz and adhering to the specified color palette and contrast rules, outline the core workflows and a key sensing mechanism in biofluid analysis.
Workflow for Biofluid Analysis
Electrochemical Sensing Pathway
The Scientist's Toolkit: Research Reagent Solutions
The development and validation of biosensors for biofluid analysis require a suite of specialized reagents and materials. The following table details key components and their functions.
Table 2: Essential Research Reagents and Materials for Biofluid Biosensor Development
| Reagent/Material | Function/Application | Key Characteristics |
|---|---|---|
| Ion-Selective Membranes | Potentiometric detection of ions (Na⁺, K⁺, Cl⁻) in sweat and tears [41] | Contains ionophore for specific ion recognition; high selectivity coefficient against interfering ions. |
| Enzyme Solutions (e.g., Glucose Oxidase, Lactate Oxidase) | Core recognition element in amperometric biosensors for metabolites [39] [41] | High specific activity, stability, and substrate specificity. Often immobilized on transducer surfaces. |
| Redox Mediators (e.g., Ferrocene derivatives) | To shuttle electrons between enzyme and electrode, improving sensor sensitivity and operating at lower potentials [40] | Reversible electrochemistry, low solubility, and stability in the immobilized state. |
| Nafion Membranes | Polymer coating used to repel negatively charged interferants (e.g., ascorbate, urate) in electrochemical sensors [40] | Cation-exchange properties; improves selectivity of the sensor interface. |
| Microfluidic Chip Substrates (e.g., PDMS) | To fabricate channels for controlled, low-volume transport of biofluids in wearable patches [39] [41] | Biocompatible, gas-permeable, flexible, and easy to fabricate via soft lithography. |
| Microneedle Arrays | Minimally invasive access to ISF for continuous monitoring of biomarkers like glucose [41] | Solid or hollow structures; length < 1 mm; fabricated from polymers, metals, or silicon. |
| Stabilization Cocktails (Protease Inhibitors) | Added to collected biofluids (especially saliva) to prevent degradation of protein-based biomarkers before analysis [41] | Broad-spectrum inhibition of serine, cysteine, and metalloproteases. |
Wearable biosensors represent a transformative technological advancement for the continuous, real-time monitoring of physiological information, moving healthcare from reactive to proactive management. These devices are particularly impactful for chronic diseases such as diabetes and cardiovascular conditions, which require ongoing surveillance to prevent complications. Modern wearable biosensors incorporate biological recognition elements, such as enzymes or antibodies, with physicochemical transducers that convert biorecognition events into quantifiable signals [1]. This integration enables dynamic, non-invasive measurements of chemical markers in biofluids like interstitial fluid (ISF), sweat, and tears, as well as continuous tracking of vital signs. The expansion of these technologies from simple activity tracking to sophisticated health monitoring platforms is reshaping personalized medicine, offering new paradigms for managing diabetes through Continuous Glucose Monitoring (CGM) and enabling unprecedented cardiovascular surveillance through multimodal sensing and artificial intelligence (AI) [42] [43].
Continuous Glucose Monitoring (CGM): Technology and Applications
CGM System Architecture and Operational Flow
Continuous Glucose Monitoring systems have revolutionized diabetes management by providing real-time insights into glucose trends, replacing traditional finger-prick tests [44]. A CGM system is a sophisticated biosensor platform consisting of hardware and software components that work in concert.
The core hardware includes a miniaturized, subcutaneous sensor typically inserted into the abdomen or arm. This sensor measures glucose levels in the interstitial fluid using a biocompatible enzyme (e.g., glucose oxidase) that reacts with glucose to generate an electrical signal proportional to glucose concentration [44] [1]. A connected transmitter wirelessly sends this data to a receiver or smartphone app, which displays real-time readings, trends, and alerts. Advanced software algorithms process the raw sensor data, filtering noise and converting electrical signals into calibrated glucose values. Modern systems increasingly incorporate predictive analytics to forecast future glucose levels, helping users prevent hypo- or hyperglycemic episodes [44].
The diagram below illustrates the continuous data flow and feedback loop in a modern CGM system:
Key CGM Metrics and Clinical Applications
CGM technology provides comprehensive glycemic assessment through standardized metrics that offer significant advantages over traditional hemoglobin A1c (HbA1c) and self-monitoring of blood glucose (SMBG). The following table summarizes the core CGM-derived metrics and their clinical significance:
Table 1: Key CGM-Derived Metrics for Glycemic Assessment
| Metric | Definition | Clinical Significance | Target Population |
|---|---|---|---|
| Time in Range (TIR) | Percentage of time glucose levels remain within target range (typically 70-180 mg/dL for diabetics) | Primary indicator of glycemic control; associated with reduced complication risk | All diabetic populations [45] [46] |
| Time Below Range (TBR) | Percentage of time glucose levels fall below target threshold (<70 mg/dL) | Identifies hypoglycemia risk; guides therapy adjustments | Insulin-treated patients [45] |
| Time Above Range (TAR) | Percentage of time glucose levels exceed target threshold (>180 mg/dL) | Identifies hyperglycemia exposure; correlates with complication risk | All diabetic populations [45] |
| Glycemic Variability | Fluctuation in glucose levels measured by coefficient of variation (CV) | Increased variability associated with oxidative stress and complications | Prediabetes and early T2D identification [46] |
| Mean Sensor Glucose | Average glucose concentration over monitoring period | Complements HbA1c with actual glucose values | All populations [45] |
CGM applications are expanding beyond traditional diabetes management. Recent evidence supports CGM use for prediabetes, where different metrics apply—specifically targeting 95%-98% time in a tighter range of 54-140 mg/dL [46]. The mean amplitude of glycemic excursion (MAGE) is particularly predictive of dysglycemic progression in this population. CGM is also being investigated for diagnosing preclinical type 1 diabetes, where glucose levels above 140 mg/dL predict progression to clinical disease [46].
Advanced CGM Experimental Protocol for Clinical Research
The following protocol outlines a comprehensive methodology for evaluating CGM efficacy in clinical research settings, adapted from contemporary study designs [45].
Study Title: Prospective Cohort Study of Pharmacist-Led CGM Intervention in Type 2 Diabetes
Primary Objective: To determine the impact of pharmacist-led CGM on glycemic control in people with type 2 diabetes (T2D) as measured by change in HbA1c.
Secondary Objectives: To assess changes in CGM-derived glycemic outcomes, health behavior, and safety outcomes.
Study Design:
- Type: 12-week prospective cohort study with historical controls
- Participants: Adults with T2D and HbA1c ≥8%
- Sample Size: 40 participants (20 intervention, 20 historical controls)
- Control Group: Historical cohort using self-monitoring blood glucose (SMBG) only
Intervention Protocol:
- Sensor Deployment: Participants wear FreeStyle Libre 2 CGM sensor for 12 weeks
- Structured Education: Receive diabetes self-management education and support (DSMES) aligned with 2022 National Standards for DSMES
- Pharmacist Visits: Five structured visits at baseline, week 2, week 4, week 6, and week 12
- Data Collection: CGM metrics, HbA1c, vital signs, medication reviews, and behavioral assessments
Table 2: Study Visit Activities and Assessments
| Activity | Visit 1 (Baseline) | Visit 2 (Week 2) | Visit 3 (Week 4) | Visit 4 (Week 6) | Visit 5 (Week 12) |
|---|---|---|---|---|---|
| Informed Consent | ✓ | ||||
| HbA1c Measurement | ✓ | ✓ | |||
| CGM Sensor Placement | ✓ | ||||
| CGM Data Review | ✓ | ✓ | ✓ | ✓ | |
| DSMES Administration | ✓ | ✓ | ✓ | ✓ | ✓ |
| Adverse Event Assessment | ✓ | ✓ | ✓ | ✓ | |
| Behavioral Surveys | ✓ | ✓ |
Outcome Measures:
- Primary Endpoint: Between-group difference in change in HbA1c from baseline to 12 weeks
- Secondary Endpoints: Changes in CGM metrics (TIR, TBR, TAR, glycemic variability), Summary of Diabetes Self-Care Activities measure, and safety parameters
Statistical Analysis:
- Descriptive statistics for baseline characteristics
- Within-group and between-group comparisons using appropriate parametric/non-parametric tests
- Multivariable regression to adjust for potential confounding factors
Cardiovascular Surveillance with Wearable Biosensors
AI-Driven Platforms for Real-Time Cardiovascular Monitoring
Cardiovascular diseases (CVDs) remain the leading cause of mortality worldwide, accounting for approximately 18 million deaths annually [42]. Wearable devices equipped with multimodal sensors offer a promising, noninvasive solution for continuous cardiovascular monitoring, enabling early detection and intervention. AI-driven platforms are essential for analyzing the vast data streams generated by these devices, identifying subtle patterns indicative of cardiovascular stress or disease that might escape human observation [42].
These platforms typically integrate single or multimodal sensors collecting electrocardiography (ECG), photoplethysmography (PPG), heart rate, blood pressure, and mobility data. AI algorithms, trained on historical datasets and optimized for real-time inference, process this information either on the wearable device itself or via cloud-based systems. The analyzed results are then communicated to clinicians, patients, or caregivers, enabling timely interventions to prevent adverse cardiovascular outcomes [42].
The following diagram illustrates the integrated workflow of an AI-driven cardiovascular surveillance system:
Cardiovascular Risk Assessment Protocol for Research Populations
Comprehensive cardiovascular surveillance requires systematic risk assessment and monitoring protocols. The following protocol is adapted from a large-scale study on healthcare workers, demonstrating an effective methodology for early CVD detection in research populations [47].
Study Title: Preventive Health Surveillance Protocol for Cardiovascular Disease Detection
Primary Objective: To determine the prevalence and risk factors of CVDs in a large cohort using a systematic preventive health surveillance protocol.
Study Design:
- Type: Retrospective observational study
- Duration: 3 years
- Participants: 6000 healthcare workers (or comparable research population)
- Setting: Institutional health surveillance program
Risk Assessment Protocol:
- Initial Screening:
- Physical examination and vital signs (BP, HR, height, weight for BMI)
- Blood pressure measurement following ACC/AHA guidelines
- 12-lead electrocardiogram (ECG)
- Blood sampling for lipid profile, glucose, inflammatory markers
Risk Stratification:
- High-Risk Criteria: Pathological CVD history, cardiovascular abnormalities on physical exam, ECG alterations, or new cardiological symptoms
- Low-Risk Classification: No abnormal findings in initial screening
Secondary Evaluation for High-Risk Participants:
- Specialist cardiological examination
- Advanced diagnostic tests as indicated (echocardiogram, stress test, 24-hour ECG monitoring, cardiac MRI, coronary angiogram)
Data Collection and Variables:
- Demographics: Age, sex, occupational category
- Clinical Parameters: BP, BMI, lipid levels, glucose levels
- Cardiovascular Diagnoses: Categorized as rhythm disorders, anatomical-functional disorders, ischemic disorders, hypertensive disorders, and other CVDs
- Risk Factors: Family history, lifestyle factors, occupational exposures
Outcome Measures:
- Prevalence of newly diagnosed CVDs
- Association between risk factors and CVD prevalence
- Performance characteristics of the surveillance protocol
Integration and Interoperability in Wearable Health Monitoring
Modern CGM and cardiovascular monitoring systems prioritize interoperability through standardized data formats and application programming interfaces (APIs). These standards enable seamless integration with electronic health records (EHRs), insulin pumps, and other health devices [44]. Many contemporary platforms support open architectures, allowing third-party applications to access physiological data for personalized insights and remote monitoring.
Compliance with health data standards like HL7 and Fast Healthcare Interoperability Resources (FHIR) ensures secure, HIPAA-compliant data exchange. Manufacturers also implement robust encryption and authentication protocols to protect user privacy [44]. This interoperability fosters a connected health ecosystem, empowering users and clinicians with comprehensive, real-time information for integrated chronic disease management.
The convergence of CGM and cardiovascular monitoring is particularly promising, given the established relationship between glycemic metrics and cardiovascular outcomes. Research demonstrates that higher CGM-measured time in range correlates with lower rates of cardiovascular complications in type 2 diabetes, including reduced mortality [46]. Integrated platforms that combine glucose and cardiovascular monitoring could provide unprecedented insights into the interplay between metabolic and cardiovascular health.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Wearable Biosensor Studies
| Category | Specific Examples | Research Function | Notes/Considerations |
|---|---|---|---|
| CGM Systems | FreeStyle Libre 2 (Abbott), Dexcom G6 | Continuous glucose monitoring in interstitial fluid | FDA-approved; research kits available; consider sensor longevity (10-14 days) [45] |
| Electrochemical Sensors | Enzyme-based biosensors (glucose oxidase), ion-selective electrodes | Detection of metabolites and electrolytes in biofluids | Biocompatibility crucial for implantable components [1] |
| Optical Sensors | Photoplethysmography (PPG) sensors, fluorescence-based systems | Monitoring cardiovascular parameters (heart rate, blood pressure, oxygen saturation) | Signal quality affected by motion artifacts [42] |
| Data Acquisition Platforms | Custom transmitter units, Bluetooth/Wi-Fi modules, cloud integration platforms | Wireless data transmission from wearable sensors | Latency requirements for real-time alerts (<5 seconds) [44] |
| AI/ML Algorithms | Lightweight deep learning models, traditional machine learning classifiers | Real-time analysis of physiological data streams | Optimization for edge computing on wearable hardware [42] |
| Biocompatible Materials | Flexible substrates, medical-grade adhesives, hydrogel membranes | Sensor housing and skin interface for prolonged wear | Minimize skin irritation and sensor biofouling [1] |
| Validation Assays | HbA1c tests, standard lipid panels, reference glucose meters | Ground truth validation of sensor accuracy | Timing synchronization critical for correlation studies [45] |
Continuous Glucose Monitoring and cardiovascular surveillance represent two of the most advanced applications of wearable biosensor technology in chronic disease management. As these technologies evolve, they are converging toward integrated systems that provide a comprehensive picture of metabolic and cardiovascular health. The experimental protocols and methodologies outlined in this document provide researchers with standardized approaches for evaluating these technologies in clinical and research settings. Future directions include developing non-invasive sensors, enhancing AI predictive capabilities, addressing cost and accessibility barriers, and establishing standardized diagnostic criteria based on continuous monitoring data [44] [42] [46]. As the evidence base grows, these technologies are poised to transform chronic disease management from episodic assessment to continuous, personalized health monitoring.
Application Notes
Wearable biosensors have evolved from rudimentary tracking devices into sophisticated platforms for non-invasive, continuous health monitoring. The innovation in form factors—specifically skin-conformal patches, smart contact lenses, and mouthguard sensors—addresses the critical need for comfortable, long-term wear and reliable biomarker access. These devices leverage advancements in flexible materials, microfluidics, and electrochemical sensing to enable diagnostics and personalized medicine outside clinical settings.
Table 1: Comparative Analysis of Innovative Wearable Biosensor Form Factors
| Feature | Skin-Conformal Patches | Smart Contact Lenses | Mouthguard Sensors |
|---|---|---|---|
| Primary Biofluid | Sweat [48] [49] | Tears [48] [50] [40] | Saliva [48] [51] |
| Key Biomarkers | Cortisol, Lactate, Uric Acid, Na+, K+ ions, Estradiol [49] | Glucose, Intraocular Pressure (IOP), Vitamins (B1, B2, B3, E, D), Hormones (Cortisol) [50] [52] | Glucose, Electrolytes, Hormones, Viruses [48] [51] |
| Sensing Modality | Primarily Electrochemical [49] | Electrochemical, Optical [50] | Electrochemical [51] |
| Key Material Substrates | PDMS, PET, PSA, Hydrogels [48] [49] | Oxygen-permeable Hydrogels, PETG [53] [48] | Polyethylene Terephthalate Glycol (PETG) [51] |
| Power & Data Transmission | NFC, Bluetooth, Battery-free via energy harvesting [48] [49] | Wireless power transfer, NFC [48] [52] | Wireless telemetry system (e.g., NFC) [51] |
| Representative Device | Fully integrated wireless patch for sweat oestradiol [49] | Purdue Hydrogel Soft Contact Lens [53] | Cavitas sensor for saliva glucose [51] |
| Limit of Detection (Example) | Cortisol: 88 pM [49] | Information Missing | Glucose in artificial saliva: 5-1000 µmol/L [51] |
Skin-Conformal Patches
Skin-conformal patches represent a paradigm shift in epidermal biosensing. Their ultra-thin, low-modulus elastomeric construction enables conformal contact with the skin, minimizing motion artifacts that plague rigid sensors during strenuous activity [54]. This form factor primarily interfaces with sweat, a biofluid rich with metabolites (lactate, uric acid), electrolytes (Na+, K+), and hormones (cortisol, estradiol) [49]. A critical innovation is the integration of soft microfluidic systems for controlled sweat sampling and transport to embedded biosensors, preventing contamination and handling minute fluid volumes [49]. These patches increasingly employ battery-free operation, leveraging Near-Field Communication (NFC) for both power and data transmission, which enhances user safety and comfort [48] [49].
Smart Contact Lenses
Smart contact lenses (SCLs) transform a common vision correction tool into a powerful platform for continuous, non-invasive health monitoring. They uniquely provide access to tear fluid, which contains biomarkers for systemic conditions like diabetes (glucose) and ocular diseases like glaucoma (intraocular pressure, IOP) [50] [40]. The major engineering challenge has been seamlessly integrating biosensors into hydrogel-based lenses without compromising oxygen permeability, vision, or comfort [53]. Purdue researchers overcame this with an electrochemical printing technique, embedding sensors for IOP and glucose into biocompatible hydrogel lenses [53]. Beyond diagnostics, SCLs are being developed as therapeutic platforms for controlled drug delivery (e.g., for glaucoma or dry eye syndrome) and even feature augmented reality capabilities, though these are largely in the prototype stage [50] [52].
Mouthguard Sensors
Mouthguard sensors, or "cavitas sensors," utilize saliva as a diagnostic biofluid. Saliva contains a wide range of biomarkers, including glucose, electrolytes, and viruses, making it suitable for monitoring oral health and systemic conditions [48] [51]. These devices are fabricated on biocompatible substrates like Polyethylene Terephthalate Glycol (PETG), which is the standard material for mouthguards, ensuring a comfortable and secure fit [51]. A seminal study demonstrated a mouthguard biosensor with integrated Pt and Ag/AgCl electrodes and an immobilized glucose oxidase membrane, capable of wireless, real-time monitoring of saliva glucose for over five hours [51]. This form factor is particularly suited for on-demand or continuous monitoring in a non-obtrusive manner.
Experimental Protocols
Protocol: Fabrication and Testing of an Electrochemical Sweat Patch for Cortisol Monitoring
This protocol outlines the procedure for creating a skin-conformal microfluidic patch for stress monitoring via cortisol detection in sweat, based on recent research [49].
Research Reagent Solutions & Materials
Table 2: Essential Materials for Sweat Patch Fabrication
| Material/Reagent | Function |
|---|---|
| Polydimethylsiloxane (PDMS) | Forms the flexible, transparent substrate and microfluidic channels of the patch [49]. |
| Ti3C2Tx MXene with laser-burned graphene | Serves as the highly sensitive electrode material for the electrochemical sensor [49]. |
| Monoclonal anti-cortisol antibodies | Biorecognition element that selectively binds to the target biomarker, cortisol [49]. |
| Pressure Sensitive Adhesive (PSA) | Creates a thin, skin-conformal layer to adhere the patch to the epidermis [49]. |
| Flexible NFC Module | Enables wireless power harvesting and data transmission to an external reader (e.g., a smartphone) [49]. |
Procedure
- Microfluidic Layer Fabrication: Fabricate the microfluidic channel network on a PDMS substrate using soft lithography or laser cutting. This network will wick and route sweat from the skin to the sensor reservoir [49].
- Sensor Electrode Fabrication & Functionalization: Pattern the working, reference, and counter electrodes on a flexible PDMS layer using the Ti3C2Tx MXene/graphene composite. Functionalize the working electrode by immobilizing the anti-cortisol antibodies to create the immunosensor [49].
- Device Integration: Laminate the following layers in order: the adhesive layer, the PDMS substrate with integrated microfluidics, the functionalized sensor layer, and a top protective layer. Integrate the flexible NFC module into the assembly, connecting it to the biosensor electrodes.
- In-Vitro Calibration: Calibrate the patch by introducing artificial sweat solutions with known cortisol concentrations (e.g., from 1 nM to 1000 nM). Use the NFC reader to record the electrochemical signal (e.g., change in current or impedance) and generate a calibration curve [49].
- On-Body Validation: Deploy the patch on human subjects under controlled conditions (e.g., during exercise to induce sweat). Collect simultaneous sweat samples for validation using a gold-standard method like liquid chromatography-tandem mass spectrometry (LC-MS/MS) to correlate the sensor's readouts with actual cortisol levels [49].
Protocol: Functional Validation of a Glucose-Sensing Smart Contact Lens
This protocol describes the steps for validating the performance of a smart contact lens designed for tear glucose monitoring, drawing from reported technologies [53] [50].
Procedure
- Lens Preparation: Obtain hydrogel-based soft contact lenses with embedded electrochemical biosensors. The working electrode should be functionalized with the enzyme glucose oxidase (GOD), which catalyzes the oxidation of glucose [53] [51].
- In-Vitro Dose-Response: Immerse the lens in a series of artificial tear solutions with varying glucose concentrations (e.g., 5-1000 µmol/L) that mimic the composition of human tears [51]. Record the amperometric (current) response of the sensor at each concentration.
- Selectivity Testing: Challenge the sensor with potential interferents found in tears (e.g., ascorbic acid, lactate, uric acid) to confirm that the enzymatic sensing mechanism is specific to glucose.
- Biocompatibility & Safety Assessment: Conduct cytotoxicity and ocular irritation tests per ISO standards to ensure the lens materials and embedded electronics are safe for prolonged contact with the cornea [50].
- In-Vivo Feasibility (Phantom or Animal Model): Test the lens in a controlled model, such as a phantom jaw that simulates the ocular environment or an appropriate animal model. Verify the wireless functionality and real-time data transmission to an external receiver over several hours [53] [51].
Protocol: Deployment of a Mouthguard Biosensor for Saliva Analysis
This protocol is adapted from a foundational study on a mouthguard-based sensor for continuous saliva glucose monitoring [51].
Procedure
- Mouthguard Fabrication: Machine a mouthguard support from a biocompatible PETG sheet. Pattern Pt (working) and Ag/AgCl (reference/counter) electrodes onto the PETG surface.
- Enzyme Immobilization: Deposit a membrane containing Glucose Oxidase (GOD) onto the surface of the Pt working electrode to create the biosensitive layer [51].
- System Integration with Telemetry: Connect the sensor to a miniaturized potentiostat and a wireless telemetry system (e.g., Bluetooth or NFC module) that can be housed in a small enclosure attached to the mouthguard.
- Performance Characterization in Artificial Saliva: Test the assembled biosensor in artificial saliva containing salts and proteins. Measure the amperometric current response across a physiologically relevant range of glucose concentrations (e.g., 5-1000 µmol/L) to establish sensitivity and linear range [51].
- Real-Time Monitoring Demonstration: Place the sensor-integrated mouthguard in a phantom jaw setup that mimics the oral cavity structure. Continuously flow artificial saliva with dynamic changes in glucose concentration and demonstrate stable, real-time monitoring for an extended period (e.g., >5 hours) via the wireless data link [51].
Visualizations
Biosensing Mechanism Workflow
Smart Contact Lens Functional Components
The convergence of wearable biosensors with digital health frameworks is revolutionizing patient care, enabling a shift from reactive, hospital-centric interventions to proactive, personalized, and continuous health monitoring. This paradigm is built upon the seamless integration of three core components: the wearable biosensors that collect physiological data, the artificial intelligence (AI) that transforms this data into actionable insights, and the telemedicine platforms that facilitate remote clinical decision-making. These integrated systems are particularly vital for managing chronic diseases, enabling remote patient monitoring, and personalizing treatment plans, thereby addressing critical challenges of accessibility and cost in modern healthcare systems [55] [56]. This document provides detailed application notes and experimental protocols to guide researchers and scientists in developing and validating these interconnected systems, with a specific focus on the context of continuous health monitoring research.
Architectural Framework for Integration
The functional integration of wearable biosensors into digital health ecosystems relies on a structured, multi-layered architecture. A typical AI-driven telemedicine system can be decomposed into the following layers [55]:
- Data Acquisition Layer: This layer comprises the wearable biosensors themselves, which are responsible for collecting real-time physiological data. These devices can include smartwatches, skin-worn patches, microneedles, and textiles that measure biochemical markers (e.g., metabolites, hormones) in biofluids like sweat, interstitial fluid, and tears, as well as physical parameters like heart rate and ECG [1] [57] [58].
- Data Transmission Layer: This layer uses encrypted communication protocols (e.g., HL7, FHIR, Bluetooth, Wi-Fi) to securely transmit the acquired patient data from the wearable device to cloud servers or institutional health databases. The ISO/IEC/IEEE 21451 standard family provides a valuable framework for ensuring interoperability and the plug-and-play capability of different devices, even from different manufacturers [59].
- AI Analytics Layer: This is the computational core where machine learning (ML) and deep learning (DL) algorithms process the incoming data streams. This layer is responsible for identifying patterns, predicting health risks, and generating alerts for anomalous readings. For instance, AI models can be trained to interpret complex biosensor data for early warning of health deterioration [55] [60].
- Decision Support Interface: This layer visualizes the AI-generated insights for clinicians through user-friendly dashboards. It often integrates with Electronic Health Records (EHR) to provide a comprehensive view of the patient's history, supporting informed clinical decision-making [55].
- Feedback and Alert System: The final layer involves a closed-loop system where real-time alerts are automatically sent to patients or healthcare providers if abnormal readings are detected, prompting timely intervention. This can be integrated with patient-facing mobile applications [55] [56].
The following diagram illustrates the data flow and logical relationships between these layers:
Diagram 1: Data flow in an AI-driven digital health framework.
AI-Driven Analytics: Protocols and Data Processing
Workflow for Developing an AI Model for Predictive Alerting
Objective: To develop and validate a machine learning model that predicts potential health events (e.g., hypoglycemic episodes) from continuous biosensor data.
Materials:
- Dataset of time-series biosensor readings (e.g., glucose levels, heart rate) with annotated event labels.
- Python programming environment (v3.8+).
- ML libraries: Scikit-learn, TensorFlow/PyTorch, Pandas, NumPy.
- Computing hardware with adequate GPU support for deep learning models.
Protocol:
- Data Preprocessing:
- Cleaning: Handle missing values using interpolation or deletion. Remove high-frequency noise with a low-pass filter (e.g., Butterworth filter) suitable for physiological signals.
- Normalization: Standardize the data to have a mean of zero and a standard deviation of one to ensure model convergence.
- Segmentation: Slice the continuous time-series data into fixed-length windows (e.g., 60-minute segments) that precede a labeled event.
Feature Engineering:
- Extract both time-domain features (e.g., mean, standard deviation, slope, area under the curve) and frequency-domain features (e.g., spectral power in relevant bands) from each data window.
- Incorporate cross-signal features if multiple biosensors are used (e.g., correlation between glucose and heart rate variability).
Model Training & Validation:
- Split the dataset into training (70%), validation (15%), and hold-out test sets (15%). Use stratified splitting to maintain class distribution.
- Train multiple candidate models, such as Random Forests, Gradient Boosting Machines (XGBoost), and Long Short-Term Memory (LSTM) networks.
- Optimize hyperparameters using the validation set via grid search or Bayesian optimization.
- Performance Metrics: Evaluate models on the test set using accuracy, precision, recall, F1-score, and Area Under the Receiver Operating Characteristic Curve (AUC-ROC). The model with the highest F1-score and AUC-ROC should be selected to balance false positives and false negatives.
Deployment & Continuous Learning:
Table 1: Quantitative Impact of AI in Telemedicine (Based on a Multi-Hospital Study) [55]
| Metric | Traditional Telemedicine | AI-Driven Telemedicine |
|---|---|---|
| Diagnostic Accuracy | 76% | 91% |
| Average Consultation Time | 22 min | 15 min |
| Patient Readmission Rate (30-day) | 13.2% | 8.7% |
| Patient Satisfaction Score (out of 5) | 3.8 | 4.6 |
Telemedicine Connectivity and Standardization Protocols
Protocol for Implementing Standardized Biosensor Communication
Objective: To ensure a wearable biosensor can seamlessly integrate and communicate data within a broader telemedicine network using a standardized protocol.
Materials:
- Wearable biosensor prototype with wireless communication capability (e.g., BLE, Zigbee).
- Microcontroller unit (MCU) or system-on-chip (SoC) with a communication stack.
- Reference for the ISO/IEC/IEEE 21451 (Dot 0 & Dot 5) standards [59].
Protocol:
- Define the Transducer Electronic Data Sheet (TEDS): For each biosensor (Transducer Channel - TCh), create a standardized TEDS. This electronic document should describe:
- Meta-TEDS: General sensor information (model, serial number, manufacturer).
- TransducerChannel-TEDS: Specific details for each sensing channel, including unit of measurement, upper/lower range limits, and calibration data.
- User's Transducer Name TEDS: A customizable name for the sensor.
- PhyTEDS: Physical characteristics of the transducer.
- For biosensors, extend the TEDS to include biospecific information, such as the target analyte, bioreceptor type (e.g., enzyme, aptamer), and calibration curve data points to allow for flexible interpolation by the application [59].
Implement the Network-Capable Application Processor (NCAP) and Transducer Interface Module (TIM) Logic:
- The TIM (often on the wearable device or a local hub) interfaces with the physical biosensor, reads its data, and packages it with the TEDS information.
- The NCAP (often a smartphone or gateway device) communicates with one or more TIMs via a standardized transducer-independent interface (TII), such as BLE (as defined in IEEE 21451-5). The NCAP is responsible for transmitting the structured data to the cloud network.
Data Transmission and Security:
- Transmit all health data using encrypted protocols (HTTPS, TLS) to comply with regulations like HIPAA and GDPR [61].
- The data payload should follow a standardized health data format, such as FHIR (Fast Healthcare Interoperability Resources), to ensure semantic interoperability with EHRs and other health IT systems [55].
Diagram 2: Standardized biosensor communication protocol.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Wearable Biosensor Research and Development
| Item / Reagent | Function / Explanation | Example Applications |
|---|---|---|
| Graphene-based Inks | Provides high electrical conductivity, mechanical flexibility, and a large surface area for biomolecule immobilization. Serves as the electrode material. | Fabrication of flexible electrochemical sensors for metabolites (lactate, glucose) in sweat [57]. |
| Bioreceptors (Enzymes, Aptamers) | The biological recognition element that confers specificity to the biosensor. Binds selectively to the target analyte. | Glucose oxidase for glucose sensing; DNA aptamers for specific detection of drugs or proteins [1] [58]. |
| Nafion & Cross-linkers (e.g., glutaraldehyde) | Polymer membrane used to immobilize bioreceptors on the electrode surface and to reject interfering species. Cross-linkers create stable bonds. | Coating on enzyme-based sensors to improve selectivity and bioreceptor stability in complex biofluids [58]. |
| Artificial Sweat / Tears Formulation | A standardized synthetic biofluid used for in-vitro calibration and testing of biosensor performance under controlled conditions. | Validating sensor accuracy and reliability before moving to human trials [1]. |
| Molecularly Imprinted Polymers (MIPs) | "Artificial antibodies"; synthetic polymers with cavities tailored to a specific template molecule. Offer high stability. | Detection of small molecules like hormones (cortisol) or drugs where biological receptors are unstable [58]. |
Challenges and Future Prospects
Despite the significant progress, several challenges remain. Data privacy and security are paramount, requiring robust encryption and governance frameworks to protect sensitive health information [61]. Sensor accuracy and reliability in uncontrolled, real-world environments necessitate ongoing improvements in materials science, such as the use of graphene and other nanomaterials to enhance sensitivity and stability [57] [58]. Algorithmic bias in AI models must be addressed through diverse training datasets and explainable AI (XAI) techniques to build clinician trust [55] [62]. Finally, regulatory approval and standardization require collaborative efforts between researchers, industry, and policymakers to ensure safe and effective devices reach the market [63].
Future directions point towards multi-analyte sensing platforms for a more holistic physiological picture, closed-loop systems (e.g., an artificial pancreas), and the use of federated learning to train AI models on decentralized data, thus preserving patient privacy [55] [63] [58]. The convergence of these technologies holds the promise of truly personalized, predictive, and participatory healthcare.
Navigating Technical Hurdles: Strategies for Enhanced Accuracy, Reliability, and User Compliance
For researchers developing wearable biosensors for continuous health monitoring, three performance metrics are paramount: sensitivity, the ability to detect low concentrations of a target biomarker; specificity, the capacity to distinguish the target analyte from interfering substances in complex biofluids; and long-term stability, the sensor's performance consistency over extended operational periods [1] [58]. Achieving excellence in these metrics ensures that data collected for remote patient monitoring, drug therapy personalization, and clinical research is reliable and clinically actionable [64]. This document outlines standardized protocols and application notes to guide the rigorous evaluation of these critical parameters, with a specific focus on electrochemical biosensing platforms that are predominant in wearable form factors such as patches, microneedles, and smart textiles [58].
The evaluation of wearable biosensors requires a structured approach to quantify key performance metrics. The following table summarizes the core metrics, their definitions, and the standard experimental methods used for their assessment.
Table 1: Key Performance Metrics for Wearable Biosensors
| Metric | Definition | Standard Measurement Method | Target Value/Range |
|---|---|---|---|
| Sensitivity | The change in sensor output signal per unit change in analyte concentration [58]. | Calibration curve generated from analyte solutions of known concentrations [58]. | Slope of the calibration curve (e.g., nA/µM, mV/decade). |
| Limit of Detection (LoD) | The lowest analyte concentration that can be reliably distinguished from a blank sample [1]. | 3σ/slope, where σ is the standard deviation of the blank signal. | Sub-micromolar or nanomolar levels for key biomarkers [1]. |
| Specificity | The sensor's ability to respond only to the target analyte in the presence of potential interferents [58]. | Measuring sensor response in solutions containing structurally similar molecules or common biofluid components (e.g., ascorbic acid, uric acid, lactate) [58]. | >95% signal retention for the target with <5% cross-reactivity. |
| Long-Term Stability | The retention of sensor performance (sensitivity, LoD) over time and continuous operation [1]. | Continuous or repeated measurement in a relevant matrix (e.g., artificial sweat, buffer) over days/weeks; monitoring signal drift. | <5% signal degradation over 72 hours of continuous operation [1]. |
The experimental workflow for a comprehensive sensor evaluation, from fabrication to validation, is outlined in the following diagram.
Detailed Experimental Protocols
Protocol for Sensitivity and Limit of Detection (LoD) Assessment
This protocol describes the procedure for establishing the sensitivity and LoD of an electrochemical wearable biosensor, using amperometry as a primary example [58].
3.1.1 Materials and Equipment
- Potentiostat/Galvanostat
- Fabricated biosensor
- Standard solutions of the target analyte at known concentrations (e.g., 0.1 µM, 1 µM, 10 µM, 100 µM) in 1X PBS, pH 7.4
- Stirring hotplate
3.1.2 Step-by-Step Procedure
- System Setup: Place the biosensor in a electrochemical cell containing 10 mL of 1X PBS, pH 7.4, under constant stirring.
- Applied Potential: Apply the optimal working potential (e.g., +0.6 V vs. Ag/AgCl for H₂O₂ detection in enzymatic sensors).
- Baseline Recording: Allow the current to stabilize and record the baseline for 60 seconds.
- Standard Additions: Sequentially add aliquots of the standard analyte solution to increase the concentration in the cell incrementally. Record the amperometric current (I) after each addition once a stable signal is achieved.
- Data Analysis: Plot the steady-state current (ΔI) against the corresponding analyte concentration. Perform linear regression analysis. The slope of the resulting calibration curve is the sensitivity.
- LoD Calculation: Record the standard deviation (σ) of the baseline current from at least 10 measurements. Calculate the LoD using the formula: LoD = 3σ / S, where S is the sensitivity (slope) of the calibration curve.
Protocol for Specificity and Cross-Reactivity Testing
This protocol evaluates the sensor's specificity by challenging it with common interferents found in the target biofluid (e.g., sweat, ISF) [58].
3.2.1 Materials and Equipment
- Potentiostat/Galvanostat
- Fabricated biosensor
- Standard solution of the target analyte at a mid-range concentration (e.g., 50 µM)
- Solutions of potential interferents (e.g., 100 µM ascorbic acid, 100 µM uric acid, 1 mM lactate) in 1X PBS, pH 7.4
3.2.2 Step-by-Step Procedure
- Initial Response: Place the biosensor in PBS and measure the amperometric response to the addition of the target analyte (50 µM). Record this current response as R_target.
- Interferent Challenge: Rinse the sensor and place it in fresh PBS. Sequentially add each potential interferent and record the sensor response.
- Mixed Solution Test: Create a mixed solution containing the target analyte (50 µM) and all interferents at their expected physiological concentrations. Measure the sensor response, R_mix.
- Data Analysis: Calculate the cross-reactivity for each interferent as (Rinterferent / Rtarget) * 100%. The response in the mixed solution should be compared to Rtarget to assess interference in a complex milieu. A specific sensor will show a response to Rtarget and R_mix, with minimal response to individual interferents.
Protocol for Long-Term Stability and Biofouling Assessment
This protocol assesses the sensor's operational stability and resistance to biofouling, which is critical for continuous monitoring [1] [58].
3.2.1 Materials and Equipment
- Potentiostat/Galvanostat
- Multiple fabricated biosensors (n ≥ 3)
- Artificial sweat or other relevant biofluid simulant
- Incubator maintained at 32°C (skin temperature)
3.2.2 Step-by-Step Procedure
- Initial Calibration: Calibrate all biosensors in PBS as per Protocol 3.1 to establish baseline sensitivity and LoD.
- Continuous Exposure: Immerse the sensors in artificial sweat and incubate at 32°C.
- Periodic Testing: At defined time points (e.g., 0, 6, 24, 48, 72 hours), remove a sensor from the simulant, rinse gently with PBS, and recalibrate in PBS.
- Data Analysis: Plot the normalized sensitivity (Sensitivityt / Sensitivityt=0) against time. Signal drift can be calculated as the percentage change in the response to a standard concentration over time. Biofouling can be assessed visually or via microscopy after the test period.
The Scientist's Toolkit: Research Reagent Solutions
The performance of a wearable biosensor is fundamentally linked to the materials and biorecognition elements used in its construction. The table below details key reagents and their functions.
Table 2: Essential Research Reagents for Wearable Biosensor Development
| Reagent / Material | Function / Application | Key Characteristics |
|---|---|---|
| Graphene-based Nanomaterials [57] [65] | Conductive electrode material for signal transduction. | High electrical conductivity, large surface area, mechanical flexibility, biocompatibility. |
| Glucose Oxidase (GOx) [58] | Model enzymatic bioreceptor for glucose detection. | High catalytic turnover, specificity for β-D-glucose. |
| Aptamers [58] | Synthetic nucleic acid-based bioreceptors for a wide range of targets (ions, drugs, proteins). | High affinity, thermal stability, ease of chemical modification, animal-free production. |
| Molecularly Imprinted Polymers (MIPs) [58] | "Artificial antibody" synthetic receptors. | High chemical/thermal stability, cost-effective production, customizable for diverse targets. |
| Nafion | Permselective membrane coating. | Cation-exchange polymer used to repel negatively charged interferents (e.g., ascorbate, urate). |
| Polyurethane Membranes | Diffusive control and biofouling-resistant layer. | Regulates analyte flux to the sensor and reduces non-specific protein adsorption. |
The selection of an appropriate bioreceptor is a critical first step in sensor design, dictating the strategy for surface functionalization and signal transduction. The following diagram outlines the decision-making workflow for bioreceptor selection and integration.
Data Analysis and Integration with Advanced Frameworks
The complex, multimodal data generated by wearable biosensors requires robust analysis and interpretation frameworks. Artificial Intelligence (AI) and Multimodal Large Language Models (MLLMs) are increasingly pivotal in enhancing data processing, identifying subtle patterns, and providing decision support [64] [66]. For instance, machine learning algorithms can be trained to deconvolute signals from interfering species, thereby improving specificity in post-processing. Furthermore, AI-driven models can correlate real-time biomarker fluctuations with physiological or mental states, such as stress or metabolic events, adding clinical context to the raw analytical data [64] [66]. This integration is essential for transforming continuous sensor data into actionable insights for personalized healthcare and drug development.
Overcoming Biofouling and Sensor Drift in Complex Biofluids
The pursuit of reliable, continuous health monitoring using wearable biosensors is fundamentally challenged by the twin obstacles of biofouling and sensor drift in complex biofluids. These phenomena represent critical barriers to the long-term accuracy and functionality of implantable and on-body sensing platforms [67]. Biofouling refers to the spontaneous, nonspecific adsorption of proteins, cells, and other biological materials onto sensor surfaces upon contact with biofluids, which can trigger a foreign body response (FBR) leading to fibrous encapsulation and analyte blockage [67]. Sensor drift describes the gradual degradation of sensor performance over time, manifesting as decreasing sensitivity, altered baseline signals, and reduced accuracy, often quantified as an increasing Mean Absolute Relative Difference (MARD) between sensor readings and reference values [67].
Within the context of a broader thesis on wearable biosensors, understanding and mitigating these challenges is paramount for translating laboratory proof-of-concept devices into clinically reliable and commercially viable monitoring systems. These limitations currently restrict functional sensor lifetimes to days or weeks, whereas chronic disease management demands months to years of continuous, reliable operation [67]. This document provides detailed application notes and experimental protocols to systematically investigate and counteract these failure modes, enabling more robust biosensor development.
Quantitative Analysis of Biofluid Compositions and Challenges
The composition of target biofluids directly influences both the rate of biofouling and the nature of sensor drift. Understanding the specific environment in which a sensor must operate is the first step in designing effective countermeasures.
Table 1: Key Characteristics of Primary Biofluids for Wearable Biosensing
| Biofluid | Primary Biomarkers | Key Biofouling Components | Typical Sensor Lifetime Challenges |
|---|---|---|---|
| Interstitial Fluid (ISF) | Metabolites (glucose, lactate), proteins, drugs, cytokines [68] | Proteins, lipids, cells [67] | Fibrous encapsulation; biorecognition element inactivation [67] |
| Sweat | Electrolytes (Na+, K+, Cl-), metabolites (lactate, urea), hormones (cortisol) [1] [68] | Proteins, dead skin cells, sebum, environmental contaminants [1] | Variable secretion rates; contamination; epidermal debris accumulation [69] |
| Saliva | Electrolytes, enzymes (amylase), hormones (cortisol), metabolites [68] | Mucins, food debris, oral microbiota [68] | Rapid microbial growth; enzymatic degradation of bioreceptors [68] |
| Tears | Glucose, proteins, proteomic/inflammatory markers [68] | Lysozyme, lipids, mucins [68] | Protein adsorption on smart contact lenses; low analyte concentrations [68] |
| Wound Exudate | pH, temperature, cytokines (IL-6, IL-8, TNF-α), MMPs [70] | Neutrophils, macrophages, bacteria, fibrin, cellular debris [70] | Highly viscous, pro-inflammatory environment; intense biofouling and rapid sensor passivation [70] |
Anti-Biofouling Material Strategies and Experimental Validation
Material selection and surface engineering are the primary defenses against biofouling. The following table summarizes the most promising material strategies, which can be employed passively or actively.
Table 2: Anti-Biofouling Material Strategies for Implantable Biosensors
| Strategy | Mechanism of Action | Key Materials | Reported Efficacy |
|---|---|---|---|
| Zwitterionic Polymers | Forms a hydration layer via electrostatic interactions, creating a physical and energy barrier to protein adsorption [67] | Poly(carboxybetaine) (PCB), Poly(sulfobetaine) (PSB) [67] | >90% reduction in protein adsorption in vitro for up to 3 months [67] |
| Hydrophilic Coatings | Creates a hydration barrier through hydrogen bonding, reducing protein adhesion [67] | Poly(ethylene glycol) (PEG), Poly(2-hydroxyethyl methacrylate) (pHEMA) [67] | Extends functional lifetime in vivo by 2-3 weeks compared to uncoated sensors [67] |
| Biomimetic/Bioinert Materials | Mimics the surface chemistry of the cell membrane to appear "invisible" to the immune system [67] | Lipid bilayers, albumin-based coatings [67] | Shows significant reduction in foreign body response in animal models [67] |
| Drug-Eluting Materials | Locally releases anti-inflammatory or anti-proliferative agents to suppress the immune response [67] | Dexamethasone-loaded polymers, nitric oxide-releasing coatings [67] | Can delay capsule formation for several weeks in rodent subcutaneous implants [67] |
| Stimuli-Responsive Materials | "On-demand" surface refreshment or anti-foulant release triggered by pH, temperature, or external fields [67] | Poly(N-isopropylacrylamide) (pNIPAM), chitosan-based hydrogels [67] | Demonstrated in vitro removal of >80% of adsorbed proteins upon trigger application [67] |
Experimental Protocol: In Vitro Biofouling Challenge and Coating Efficacy Assessment
Objective: To quantitatively evaluate the performance and durability of anti-biofouling coatings under simulated physiological conditions.
Materials:
- Phosphate Buffered Saline (PBS): For baseline stability testing.
- Fetal Bovine Serum (FBS) or Artificial Biofluids: Represents a complex protein-rich environment for accelerated biofouling [67].
- Electrochemical Workstation: For monitoring sensor signal stability.
- Model Analyte: e.g., Glucose, Lactate, Hydrogen Peroxide, at physiologically relevant concentrations [58].
- Quartz Crystal Microbalance (QCM) or Surface Plasmon Resonance (SPR): For real-time, label-free quantification of protein adsorption (optional) [67].
Procedure:
- Sensor Functionalization: Immobilize the requisite bioreceptor (e.g., enzyme, aptamer) on the electrode surface using standard covalent chemistry (e.g., EDC-NHS for enzymes) or physical adsorption [58].
- Coating Application: Apply the test anti-biofouling coating (e.g., via dip-coating, spin-coating, or in-situ polymerization) onto the functionalized sensor. Include an uncoated but functionalized sensor as a negative control.
- Baseline Characterization:
- Calibrate all sensors in PBS and a standard solution of the model analyte.
- Record the initial sensitivity, limit of detection (LOD), and response time.
- Biofouling Challenge:
- Immerse the sensors in FBS (or an appropriate artificial biofluid) at 37°C under gentle agitation.
- Periodically (e.g., every 24 hours), remove sensors, rinse gently with PBS, and re-calibrate in the standard analyte solution.
- Record the change in sensitivity and LOD over time (e.g., 7-30 days).
- Data Analysis:
- Calculate the signal attenuation as:
(Initial Sensitivity - Sensitivity at Time t) / Initial Sensitivity * 100%. - Plot signal attenuation vs. time for each coating strategy. A superior coating will show a slower rate of signal decay and a lower final attenuation.
- Calculate the signal attenuation as:
Understanding and Mitigating Sensor Drift
Sensor drift is a multifactorial problem often linked to, but distinct from, biofouling. It can be abiotic (e.g., electrode corrosion, insulation delamination) or biotic (e.g., inactivation of biorecognition elements, passivation) in origin [67].
Protocol for Isulating and Characterizing Drift Components
Objective: To deconvolute the sources of sensor drift in a controlled environment.
Materials:
- Potentiostat/Galvanostat
- Buffer solutions at varying pH levels (e.g., pH 5.0, 7.4, 9.0)
- Solutions of common interferents (e.g., Acetaminophen, Uric Acid, Ascorbic Acid)
- Redox standard solutions (e.g., Ferricyanide)
Procedure:
- Electrochemical Integrity Testing:
- Perform Cyclic Voltammetry (CV) in a standard redox couple (e.g., 5mM K₃[Fe(CN)₆] in PBS) daily.
- Monitor the shift in peak potential (ΔEp) and the decay in peak current over time. An increasing ΔEp suggests electrode surface fouling or passivation, while a decaying current indicates a loss of electroactive area [58].
- Bioreceptor Stability Assessment:
- For enzymatic sensors, measure the amperometric response to a fixed concentration of analyte and co-substrate daily [58].
- A decaying signal indicates inactivation of the enzyme, which can be due to leaching, denaturation, or chemical degradation.
- Environmental Interference Testing:
- Challenge the sensor with solutions of physiological interferents.
- A growing response to interferents suggests degradation of permselective membranes (e.g., Nafion) designed to block them [67].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Biofouling and Drift Studies
| Item/Category | Function in Research | Example Products/Specifications |
|---|---|---|
| Zwitterionic Monomers | Synthesis of ultra-low fouling polymer brushes and hydrogels via surface-initiated polymerization [67] | Carboxybetaine acrylamide (CBAA), Sulfobetaine methacrylate (SBMA) |
| PEG-Based Crosslinkers | Creating hydrophilic, non-fouling hydrogels and surface coatings; spacer for bioreceptor immobilization [67] | Poly(ethylene glycol) diacrylate (PEGDA), NHS-PEG-NHS |
| Electrochemical Redox Standards | Monitoring electrode surface integrity and fouling status over time [58] | Potassium Ferricyanide (K₃[Fe(CN)₆]), Ruthenium Hexamine (Ru(NH₃)₆Cl₃) |
| Artificial Biofluids | Standardized and consistent medium for accelerated biofouling and drift testing in vitro [67] | Artificial Sweat (ISO 3160-2), Artificial Interstitial Fluid, Artificial Tears |
| Permselective Membranes | Blocking interferents to improve selectivity and reduce drift from false signals [67] [58] | Nafion (cation exchanger), m-Phenylenediamine (o-PD) films |
| Biocompatible Encapsulants | Providing a physical barrier against the biological environment and mitigating FBR [67] | Medical-grade polyurethane, PDMS, Parylene-C |
| Stimuli-Responsive Polymers | Developing active, "self-cleaning" sensor surfaces that release foulants upon trigger [67] | pNIPAM (temperature-responsive), Chitosan (pH-responsive) |
Integrated Experimental Workflow: From In Vitro to In Vivo Validation
A robust validation pipeline is essential to bridge the gap between controlled lab experiments and real-world application.
Protocol: In Vivo Validation and Explant Analysis
Objective: To assess the long-term performance and biocompatibility of biosensors in a live animal model and correlate results with in vitro findings.
Materials:
- Approved Animal Model (e.g., rodent)
- Sensor implantation kit (sterile)
- In vivo data acquisition system (e.g., wireless potentiostat)
- Blood glucose meter or other reference method for correlation
- Tissue fixation and histological staining supplies (H&E, Masson's Trichrome)
Procedure:
- Pre-implantation: Sterilize the biosensors and record final in vitro performance metrics.
- Sensor Implantation: Surgically implant the test and control sensors subcutaneously in the animal subject, following approved ethical protocols.
- Continuous Monitoring: Record sensor signals continuously or at regular intervals via a wireless data acquisition system.
- Reference Sampling: Periodically collect blood samples (or other relevant biofluid) for benchmark analysis using a gold-standard method (e.g., clinical analyzer).
- Data Analysis: Calculate the MARD between the sensor readings and the reference values over the implantation period [67].
- Explant and Histology:
- After a predetermined period (e.g., 2-4 weeks), euthanize the animal and carefully explant the sensors with surrounding tissue.
- Fix the tissue, section, and stain (e.g., H&E for general morphology, Masson's Trichrome for collagen).
- Measure the thickness of the fibrous capsule formed around each sensor. A thinner capsule indicates a more biocompatible, less fouling surface [67].
- Correlation: Correlate the in vivo MARD and final capsule thickness with the in vitro signal attenuation data obtained from Protocol 3.1. This correlation is crucial for predicting in vivo performance from faster, cheaper in vitro tests.
Power Management and Battery Life Optimization for Continuous Operation
For researchers developing wearable biosensors for continuous health monitoring, power management is a pivotal challenge that dictates device viability and reliability. Achieving extended operational lifetime requires a holistic strategy integrating low-power electronic design, advanced battery technologies, and innovative energy harvesting techniques [71] [72]. These approaches are essential for supporting uninterrupted, long-duration clinical trials and enabling robust data collection for healthcare research and drug development [72].
Quantitative Analysis of Power Components
Optimization begins with a thorough understanding of the power budget. The table below summarizes the typical power consumption and characteristics of core subsystems in a wearable biosensor.
Table 1: Power Consumption Profile of Typical Wearable Biosensor Components
| System Component | Typical Power Consumption | Key Power-Influencing Factors |
|---|---|---|
| Microcontroller Unit (MCU) | Varies with architecture & active/sleep mode [72] | Sampling rate (e.g., 20 Hz vs. 100 Hz), FPU usage, duty cycling, operating voltage [72]. |
| Wireless Communication (BLE) | Very Low (optimized for short-range) [71] | Data transmission frequency, payload size, connection interval, use of advertising vs. connected modes [71] [73]. |
| Electrochemical Biosensors | Low (e.g., µW to mW range for amperometric sensors) | Sensing technique (amperometry, potentiometry), measurement frequency, number of active sensors [1] [74]. |
| Inertial Sensors (Accelerometer) | Low | Output data rate (ODR), dynamic range, and active measurement duration [73]. |
Low-Power Microcontroller Design
The MCU is a central power consumer. Selecting an ultra-low-power architecture like the ARM Cortex-M series and meticulously managing its operation is critical. Key strategies include:
- Sampling Rate Optimization: Reducing the MCU sampling rate to the minimum required for the bio-signal (e.g., 20 Hz) can dramatically lower power dissipation compared to higher rates like 100 Hz [72].
- Duty Cycling: Implementing aggressive duty cycling, where the MCU and peripherals are kept in deep sleep or low-power mode for the maximum possible time and are only woken up periodically to perform measurements and data transmission, is a foundational technique [73].
- Dynamic Voltage and Frequency Scaling (DVFS): Adjusting the processor's voltage and clock frequency based on the computational workload can yield significant energy savings [73].
- Edge Processing: Performing data processing and filtering on the device (at the edge) rather than transmitting raw data reduces the volume and frequency of power-intensive wireless transmissions [71] [72].
Power Source Technologies and Performance
Selecting and managing the primary power source is fundamental to achieving long-term operation. The following table compares the key attributes of common and emerging power sources for wearable biosensors.
Table 2: Comparison of Power Sources for Wearable Biosensors
| Power Source | Energy / Power Density | Key Advantages | Key Limitations / Challenges |
|---|---|---|---|
| Lithium-Ion/Polymer Battery | Gravimetric: ~200 W·h/kgVolumetric: ~550 W·h/L [75] | High energy density, mature technology, rechargeable, low self-discharge (~2%/month) [75]. | Finite energy capacity, rigid form factor in standard cells, safety concerns, performance degrades over cycles [76] [75]. |
| Custom/Shaped Batteries | High energy density (e.g., up to 460 Wh/L) [76] | Enables optimal use of device space, flexible and customizable form factors (ultra-thin, curved, etc.) [76]. | Customization cost, may require specialized manufacturing and integration processes. |
| Enzymatic Biofuel Cells (EBFCs) | Low to moderate power density (area for improvement) [77] | Self-powered operation using biofluids (e.g., glucose in sweat/ISF), biocompatible, enables continuous operation [77]. | Low power output, limited operational stability/enzyme lifetime, miniaturization complexity [77]. |
| Thermoelectric Generators (TEGs) | Low conversion efficiency (~1-2% from body heat) [76] | Harvests perpetual body heat, suitable for low-power devices. | Very low power output, highly dependent on ambient temperature and skin contact [76]. |
Battery Management and System Power Regulation
- Battery Management Systems (BMS): A BMS is crucial for monitoring state-of-charge, protecting against over-charging/discharging, and ensuring safe operation, thereby maximizing the effective lifespan of the battery [73].
- Efficient Power Conversion: Using high-efficiency, low-quiescent-current DC-DC switching converters instead of linear regulators is essential for power rail management. Multi-rail DC-DC configurations or switched-capacitor converters can achieve system-wide efficiencies of up to 80% or more [76].
Experimental Protocol for Power Profiling and Optimization
This protocol provides a methodology to empirically characterize and optimize the power consumption of a wearable biosensor platform.
Objective: To measure the total power consumption of a wearable biosensor system, identify the main power-consuming states and events, and validate the efficacy of power-saving strategies to extend operational battery life.
Materials:
- Prototype wearable biosensor board (including MCU, sensors, and wireless module)
- Programmable DC power supply
- Digital Multimeter / Precision current-sense amplifier / Source Measurement Unit (SMU)
- Oscilloscope (optional, for transient analysis)
- Host computer for data logging and device control
Procedure:
- Test Setup: Connect the power supply to the device's battery input terminals, set to the nominal battery voltage (e.g., 3.7 V for Li-Po). Place a precision current-sense resistor (e.g., 1-10 Ω) in series with the power line. Measure the voltage drop across the resistor to calculate current draw.
- Baseline Profiling:
- a. Place the device in its deepest sleep mode and record the baseline current (
I_sleep). - b. Trigger a single measurement cycle (activate sensors, take reading, process data) and capture the current profile, noting peak current and duration.
- c. Activate the wireless module (e.g., BLE) for a data transmission event and capture the current profile.
- a. Place the device in its deepest sleep mode and record the baseline current (
- Duty Cycling Optimization:
- a. Program a fixed duty cycle (e.g., 1%: active for 10 ms, sleep for 990 ms).
- b. Measure the average current consumption over several cycles.
- c. Repeat step 3b for different duty cycles (e.g., 0.1%, 5%) and different active state configurations (sensors on/off, transmission on/off).
- Data Processing vs. Transmission Trade-off:
- a. Measure the energy required to process 1 minute of raw sensor data on the edge MCU.
- b. Measure the energy required to transmit the equivalent 1 minute of raw data via BLE.
- c. Compare the two values to determine the most energy-efficient strategy for a given data payload.
- Battery Life Calculation:
- Using the measured average current (
I_avg) from the optimized profile and the connected battery's rated capacity (C_batin mAh), calculate the projected battery life:Battery Life (hours) = C_bat / I_avg.
- Using the measured average current (
The following workflow outlines the systematic approach to power optimization detailed in this protocol.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for Self-Powered Biosensor Research
| Item / Technology | Function / Application in Research |
|---|---|
| ARM Cortex-M4 MCU | A low-power microprocessor platform for implementing and testing edge processing algorithms and power-saving modes like duty cycling [72]. |
| Bluetooth Low Energy (BLE) Module | A low-power wireless communication module used to study the impact of data payload and transmission intervals on total system power consumption [71] [73]. |
| Enzymatic Biofuel Cell (EBFC) Test Setup | Used to investigate self-powering for continuous monitoring; includes enzymes (e.g., glucose oxidase), mediators, and nanostructured electrodes (carbon nanotubes, graphene) to enhance electron transfer and power density [77]. |
| Custom/Shaped Lithium Polymer Battery | A high-energy-density, form-factor-specific power source used to maximize operational runtime within the constrained volume of a wearable device prototype [76]. |
| Nanostructured Electrode Materials | Materials like carbon nanotubes, graphene, and noble metals are used to modify biosensor electrodes, improving sensitivity and efficiency, which can allow for less power-intensive signal measurement [77] [74]. |
Advanced Energy Harvesting Pathways
For perpetual operation, supplementing or replacing batteries with energy harvesting is a key research frontier. The following diagram illustrates the integration of multiple ambient energy sources into the biosensor's power system.
Enzymatic Biofuel Cells (EBFCs) show significant promise for creating truly self-powered biosensors. They leverage biological catalysts (enzymes) to convert energy from biochemical fuels (e.g., glucose, lactate) in biofluids directly into electricity [77]. Critical research focuses on:
- Electron Transfer Mechanisms: Optimizing Direct Electron Transfer (DET) using nanomaterials to avoid mediators, or engineering efficient Mediated Electron Transfer (MET) systems for higher power output [77].
- Enzyme Immobilization: Techniques like covalent binding, cross-linking, and encapsulation within nanostructured materials are vital to enhance enzyme stability and operational lifespan, which are currently key limitations [77].
Ensuring Mechanical Compliance and Biocompatibility for Long-Term Wear
The successful deployment of wearable biosensors for continuous health monitoring is fundamentally dependent on two core material properties: mechanical compliance and biocompatibility. Mechanical compliance ensures that the device moves and stretches with the human body without impeding natural activity or delaminating from the skin, thereby guaranteeing consistent signal quality [57] [49]. Biocompatibility, on the other hand, ensures that the device does not induce adverse biological reactions—such as irritation, inflammation, or toxicity—during prolonged contact with the skin or other tissues [1] [78]. For researchers and drug development professionals, mastering the protocols for evaluating these properties is crucial for translating laboratory prototypes into reliable, clinically valid tools for longitudinal studies and therapeutic monitoring. This document provides detailed application notes and experimental protocols to standardize these critical assessments.
Material Selection and Key Properties
The selection of substrate and sensing materials dictates the fundamental performance of a wearable biosensor. The ideal materials combine exceptional mechanical flexibility, solid electrical properties, and proven biological safety.
Table 1: Key Material Classes for Wearable Biosensors
| Material Class | Example Materials | Key Properties | Primary Functions | Research Considerations |
|---|---|---|---|---|
| Flexible Substrates | Polydimethylsiloxane (PDMS), Polyimide, Polyurethane, Ecoflex [49] [79] | Low Elastic Modulus, High Stretchability (>>20% strain), Gas Permeability [49] | Device support, Skin interfacing, Encapsulation | PDMS offers transparency and ease of fabrication but may require surface treatments for strong adhesion. |
| Conductive Nanomaterials | Graphene, MXene (Ti₃C₂Tₓ), Gold Nanoparticles (AuNPs), Laser-induced Graphene (LIG) [57] [49] | High Electrical Conductivity, Large Surface Area, Mechanical Durability [57] | Electrode fabrication, Signal transduction, Electrochemical sensing | Graphene and MXene offer excellent conductivity and can be functionalized for specific biomarker detection [57]. |
| Biorecognition Elements | Enzymes (e.g., Glucose Oxidase), Aptamers, Antibodies, Molecularly Imprinted Polymers (MIPs) [49] [1] | High Specificity and Affinity for Target Analyte | Selective biomarker recognition | Long-term stability of biologics (enzymes/antibodies) is a key challenge; MIPs offer superior stability [49]. |
Experimental Protocols
Protocol for In Vitro Cytotoxicity and Biocompatibility Testing
This protocol assesses the biological safety of sensor materials and their extracts using mammalian cell cultures, in line with ISO 10993-5 standards.
1. Reagent Preparation:
- Test Material Extract: Sterilize the sensor material (e.g., a 1 cm² patch) under UV light for 30 minutes per side. Immerse in 5 mL of complete cell culture medium (e.g., DMEM with 10% FBS) in a sterile tube. Incubate at 37°C for 24 hours to prepare the extract.
- Control Groups: Prepare a negative control (medium alone) and a positive control (medium with 1% v/v Triton X-100 or 5% DMSO).
2. Cell Seeding:
- Culture an appropriate mammalian cell line, such as L929 fibroblasts or human keratinocytes (HaCaT).
- Trypsinize, count, and seed cells into a 96-well plate at a density of 10,000 cells per well in 100 µL of complete medium.
- Incub the plate at 37°C in a 5% CO₂ atmosphere for 24 hours to allow cell attachment.
3. Extract Exposure:
- Aspirate the medium from the wells.
- Add 100 µL of the test material extract, negative control, or positive control to the respective wells (n=6 per group).
- Return the plate to the incubator for a further 24 hours.
4. Viability Assessment (MTS Assay):
- Prepare the MTS reagent mixture according to the manufacturer's instructions.
- After the 24-hour exposure, carefully aspirate the extracts and add 110 µL of fresh medium containing 10% MTS reagent to each well.
- Incubate for 1-4 hours at 37°C, protected from light.
- Measure the absorbance at 490 nm using a microplate reader.
5. Data Analysis:
- Calculate the cell viability as a percentage:
(Mean Absorbance of Test Group / Mean Absorbance of Negative Control) × 100. - A material is generally considered non-cytotoxic if cell viability exceeds 70-80% relative to the negative control.
Protocol for Mechanical Compliance and Fatigue Testing
This protocol evaluates the mechanical robustness and electrical stability of the wearable sensor under simulated on-body conditions, including cyclic stretching.
1. Substrate Preparation:
- Fabricate the sensor on the chosen flexible substrate (e.g., a PDMS sheet).
- Mount the sensor specimen firmly onto a uniaxial tensile testing system, ensuring the active sensing area is aligned with the direction of strain.
2. Static Mechanical Characterization:
- Program the tester to perform a tensile test at a constant strain rate (e.g., 1 mm/min) until fracture.
- Record the stress-strain curve to determine the Young's Modulus, ultimate tensile strength, and failure strain of the material system.
3. Dynamic Fatigue Testing:
- Program the tester for cyclic loading. A common regimen is 10,000 cycles at 0.5 Hz, with a strain amplitude representative of body motion (e.g., 15-30% strain for forearm or chest-worn devices) [79].
- Simultaneously, monitor the electrical resistance of the conductive traces in real-time using a multimeter or source meter.
4. Post-Test Analysis:
- Visual Inspection: Examine the sensor under a microscope for cracks, delamination, or permanent deformation.
- Electrical Performance: Calculate the change in baseline resistance before and after cycling. A change of less than 5-10% is typically targeted for stable operation.
- Electrochemical Performance: For electrochemical sensors, re-run calibration curves for key analytes (e.g., glucose, cortisol) after fatigue testing to quantify any signal drift.
Diagram 1: A workflow for validating sensor mechanical and biological safety.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagent Solutions for Wearable Sensor Development
| Reagent / Material | Function / Application | Specific Example / Rationale |
|---|---|---|
| Polydimethylsiloxane (PDMS) | The predominant elastomer for flexible substrates and microfluidic channels due to its biocompatibility and optical clarity [49]. | SYLGARD 184 Silicone Elastomer is widely used. A 10:1 base-to-curing agent ratio is standard [80]. |
| Graphene-based Inks | Forming highly conductive, flexible, and sensitive electrodes for biophysical and biochemical sensing [57]. | Dispersions of graphene oxide (GO) can be inkjet-printed and subsequently reduced (rGO) to enhance conductivity. |
| Molecularly Imprinted Polymers (MIPs) | Synthetic biorecognition elements for detecting specific molecules (e.g., cortisol, oestradiol) with superior long-term stability over antibodies [49]. | A MIP for cortisol can be synthesized using cortisol as a template, methacrylic acid as a monomer, and ethylene glycol dimethacrylate as a crosslinker. |
| Gold Nanoparticles (AuNPs) | Enhancing electrochemical signal amplification and facilitating biomolecule immobilization due to their high surface area and conductivity [81] [49]. | Functionalized AuNPs are used in aptasensors, e.g., for hormone monitoring, to lower the limit of detection. |
| Enzymes (e.g., Glucose Oxidase, Lactate Oxidase) | Biocatalytic recognition elements for continuous metabolite monitoring in sweat or interstitial fluid [1] [78]. | Must be stabilized within a polymer matrix (e.g., Nafion) to retain activity under wearable operating conditions. |
Achieving reliable mechanical compliance and robust biocompatibility is not an ancillary consideration but a central challenge in the development of wearable biosensors for long-term health monitoring. The protocols and materials outlined here provide a foundational framework for researchers to systematically evaluate and iteratively improve their designs. As the field progresses, the integration of advanced materials like graphene and MIPs, coupled with standardized and rigorous testing as described, will be instrumental in moving these innovative devices from laboratory proof-of-concept to trusted tools in clinical research and therapeutic drug development.
Wearable biosensors are revolutionizing continuous health monitoring by providing real-time, dynamic physiological data outside traditional clinical settings [48]. These devices, which can take the form of skin-worn patches, smart contact lenses, or mouthguard sensors, enable the non-invasive sampling of biofluids like sweat, saliva, tears, and interstitial fluid [1] [48]. However, the transition of this technology from validated research prototypes to reliable components of clinical and research workflows hinges on addressing three fundamental standardization challenges: calibration for ensuring data accuracy across diverse conditions, interoperability for seamless data exchange between systems, and security for protecting sensitive physiological information [82] [17] [48]. This Application Note details the specific hurdles within these domains and provides structured protocols to guide researchers and drug development professionals in overcoming them.
Calibration Challenges and Protocols
Calibration presents a multi-faceted challenge for wearable biosensors, primarily due to the dynamic nature of biofluids and the need for long-term sensor stability in uncontrolled environments.
Key Calibration Challenges
The correlation between analyte concentrations in easily accessible biofluids (e.g., sweat, saliva) and blood levels remains a significant obstacle, requiring robust, individualized calibration models [1]. Furthermore, sensor performance is susceptible to environmental factors such as temperature and humidity, as well as user-specific variations like sweat rate, which can dramatically impact signal output [82] [48]. Over time, issues such as sensor drift and biofouling—the accumulation of biological material on the sensor surface—degrade accuracy, necessitating recalibration strategies that are often impractical for end-users [17].
Table 1: Key Calibration Challenges and Impact on Data Quality
| Challenge | Description | Impact on Data |
|---|---|---|
| Variable Biofluid Composition | Analyte concentration in sweat/saliva vs. blood correlation is not always direct or constant [1]. | Affects physiological relevance and clinical validity of measurements. |
| Environmental Influence | Fluctuations in ambient temperature and humidity alter sensor response and biofluid secretion rates [82]. | Introduces noise and inaccuracies, reducing reliability. |
| Sensor Drift | Gradual change in sensor signal over time despite constant analyte concentration [17]. | Leads to a loss of long-term accuracy, requiring frequent recalibration. |
| Biofouling | Accumulation of proteins and cells on the sensor surface, degrading its function [17]. | Causes signal attenuation and eventual sensor failure. |
Experimental Protocol: A Multi-Level Validity Assessment
To systematically evaluate and validate the performance of a wearable biosensor, a standardized, multi-level protocol is essential. The following procedure, adapted from van Lier et al., provides a comprehensive framework [83].
Protocol Title: Multi-Level Validity Assessment for Wearable Biosensors Primary Measured Parameters: Heart Rate (HR), Root Mean Square of Successive Differences (RMSSD), Standard Deviation (SD) of intervals, Skin Conductance Response (SCR) Amplitude. Equipment: Wearable biosensor under investigation (e.g., E4 biosensor), gold-standard reference device (e.g., clinical-grade ECG for HR, laboratory-grade galvanic skin response monitor), controlled stress-inducing stimuli (e.g., cognitive tasks, acoustic startlers), data acquisition software.
Signal-Level Validation (Cross-Correlation)
- Objective: To assess the raw waveform fidelity of the wearable device compared to a gold-standard reference.
- Procedure: Simultaneously record a physiological signal (e.g., photoplethysmogram for HR or skin conductance) from the wearable device and the reference device for a minimum of 30 minutes under resting and controlled stress conditions. Synchronize the data streams temporally. Calculate the cross-correlation coefficient between the two signals across a range of time lags.
- Success Criterion: A high cross-correlation coefficient (>0.9) at a minimal time lag indicates excellent raw signal agreement.
Parameter-Level Validation (Bland-Altman Analysis)
- Objective: To quantify the agreement between derived parameters (e.g., HR, RMSSD) from the wearable and reference devices.
- Procedure: Extract parameters from both devices over consecutive, non-overlapping epochs (e.g., 5-minute intervals). Perform a Bland-Altman analysis by plotting the mean of the two device measurements against their difference for each epoch. Calculate the mean difference (bias) and the 95% limits of agreement (LoA).
- Success Criterion: A small bias and narrow LoA, deemed clinically or scientifically acceptable for the intended application, indicate good parameter-level agreement.
Event-Level Validation (Event Difference Plots)
- Objective: To evaluate the device's ability to detect physiologically meaningful changes in response to external stressors.
- Procedure: Expose participants to standardized, time-locked stressors. For each event, calculate the change in a parameter (e.g., peak SCR amplitude) from a pre-stimulus baseline for both the wearable and reference device. Create event difference plots to visualize the consistency in detecting the magnitude of physiological change across events and devices.
- Success Criterion: The wearable device should consistently detect significant physiological changes with a magnitude and timing comparable to the reference standard, particularly for strong, sustained stressors [83].
The following workflow diagrams the logical sequence of this multi-level validation protocol.
Interoperability and Data Integration
For data from wearable biosensors to be actionable in research and clinical contexts, it must flow seamlessly into data analysis platforms and health records, a process fraught with interoperability challenges.
Interoperability Hurdles
A lack of uniform communication protocols can hinder the direct transfer of data from the device to other systems [82]. Furthermore, the absence of common data formats and semantic standards for representing biomarker data makes it difficult to aggregate or compare datasets from different manufacturers or research studies [48]. Finally, integrating biosensor data into existing clinical infrastructure, such as Electronic Health Records (EHRs), requires secure and standardized APIs that are not yet universally implemented [84].
Table 2: Core Interoperability Standards and Their Applications
| Standard/Technology | Primary Function | Role in Wearable Biosensing |
|---|---|---|
| Bluetooth Low Energy (BLE) | Short-range wireless communication [82]. | Enables real-time data transmission from the sensor to a smartphone or hub. |
| Near-Field Communication (NFC) | Short-range, contactless data transfer [48]. | Used for battery-free operation and initiating data offload by tapping a reader. |
| Standardized APIs | Application Programming Interfaces [82]. | Facilitates integration of sensor data into third-party apps, cloud platforms, and EHRs. |
| Open SDKs | Software Development Kits [84]. | Allows developers to create custom applications and integrate data into broader health management systems. |
Security and Privacy Protocols
The continuous nature of wearable biosensors generates vast amounts of sensitive physiological data, making robust security and privacy protocols non-negotiable.
Security Risks and Countermeasures
The primary risks include data breaches during transmission or storage, and unauthorized access to personal health information [82] [17]. To mitigate these, end-to-end encryption for data in transit and at rest is a fundamental requirement [84]. Additionally, secure authentication protocols are needed to ensure that only authorized users and systems can access the data [17]. From a regulatory perspective, compliance with frameworks like the Health Insurance Portability and Accountability Act (HIPAA) in the U.S. and the General Data Protection Regulation (GDPR) in the EU is mandatory for clinical and research applications [82] [84].
The diagram below illustrates a secure data flow architecture from the sensor to the end-user, incorporating key security measures.
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and validation of wearable biosensors rely on a suite of specialized materials and reagents that enable sensitive, specific, and stable sensing.
Table 3: Key Research Reagent Solutions for Wearable Biosensor Development
| Reagent/Material | Function | Example Application |
|---|---|---|
| Graphene & Carbon Nanotubes | Nanomaterials providing high electrical conductivity, large surface area, and mechanical flexibility [57] [85]. | Used in electrochemical transducers to enhance sensitivity for detecting metabolites like glucose and lactate [57]. |
| Biorecognition Elements | Biological molecules (enzymes, antibodies, aptamers) that provide selective binding to target analytes [1] [86]. | Enzyme (e.g., alcohol oxidase) for alcohol biosensors [82]; antibodies for specific protein/pathogen detection [84]. |
| Supramolecular Hydrogels | Water-swollen polymer networks that are highly biocompatible and can mimic body tissues [86] [85]. | Acts as an interface between the sensor and skin, facilitating analyte sampling in sweat while improving biocompatibility [86]. |
| Flexible Substrates (PDMS, PET) | Polymers (e.g., Polydimethylsiloxane, Polyethylene Terephthalate) that provide flexibility and stretchability [48] [85]. | Serves as the base material for epidermal patches, ensuring conformal contact with the skin and user comfort during long-term wear [48]. |
| Conductive Inks (Silver/Carbon) | Inks containing conductive particles that can be printed onto flexible substrates [85]. | Enables mass fabrication of lightweight, flexible electrodes and circuits for disposable or single-use sensor strips [85]. |
The successful standardization of data from wearable biosensors is a critical enabler for their broader adoption in clinical research and drug development. While significant challenges in calibration, interoperability, and security persist, the frameworks, protocols, and material solutions detailed in this Application Note provide a actionable roadmap for researchers. Addressing these challenges through collaborative, multidisciplinary efforts will unlock the full potential of wearable biosensors to deliver reliable, meaningful health insights, thereby advancing the frontiers of personalized medicine and continuous remote monitoring.
Benchmarks and Market Viability: Evaluating Sensor Performance and Commercial Readiness
Establishing Standardized Evaluation Frameworks for Clinical Validation
In the rapidly evolving field of wearable biosensors for continuous health monitoring, establishing standardized evaluation frameworks is not merely beneficial—it is essential for clinical acceptance and reliable translation from research to practical healthcare applications. The journey from innovative proof-of-concept demonstrations to clinically validated tools requires rigorous, systematic validation protocols to ensure data quality, measurement accuracy, and ultimately, clinical utility [87] [1]. Wearable biosensors have tremendous potential to transform healthcare through continuous, real-time physiological monitoring, yet widespread adoption by medical communities depends heavily on demonstrating validated performance through multidisciplinary collaboration between engineering, biological, and clinical disciplines [1].
The current landscape of wearable biosensor validation suffers from significant challenges, including the use of different (sometimes inappropriate) statistical methods, evaluation on different variable levels, and a critical lack of standardized decision criteria to determine validity [88]. These issues lead to inconclusive and incomparable inferences across studies, hindering clinical acceptance. This application note addresses these challenges by presenting a comprehensive, standardized validation framework specifically designed for wearable biosensors in continuous health monitoring research.
Comprehensive Validity Assessment Protocol
Three-Level Validation Framework
A robust validity assessment protocol for wearable biosensors should operate across three distinct yet complementary levels: signal, parameter, and event. This multi-level approach enables comprehensive evaluation from raw data quality to clinical relevance [88].
Table 1: Three-Level Validity Assessment Framework for Wearable Biosensors
| Validation Level | Assessment Focus | Standardized Statistical Methods | Decision Criteria |
|---|---|---|---|
| Signal Level | Raw data similarity between wearable and reference device | Cross-correlation with time displacement analysis | Cross-correlation > 0.9 with mean difference testing |
| Parameter Level | Physiological parameter accuracy (e.g., heart rate, RMSSD) | Bland-Altman plots with limits of agreement | Agreement within pre-defined clinical acceptability bounds |
| Event Level | Ability to detect physiological changes due to external events | Event difference plots with statistical testing | Significant detection of stressor responses (p < 0.05) |
At the signal level, the most direct form of comparison assesses whether new devices can generate essentially the same raw data as established reference hardware. For electrodermal activity (EDA), this involves comparing skin conductance measurements (in microsiemens) between the wearable and reference device, while accounting for anatomical differences in measurement locations (e.g., wrist versus fingers) [88]. For cardiovascular activity, comparison at the raw signal level is more complex when different measurement techniques are used (e.g., photoplethysmography versus electrocardiography), though derived parameters can still be rigorously compared [88].
The parameter level determines whether a wearable device produces physiologically relevant parameters (e.g., heart rate, heart rate variability metrics) that are equivalent to those derived from reference standards. This level is particularly crucial for clinical applications where specific parameter thresholds inform diagnostic or therapeutic decisions [88].
The event level represents the highest validation tier, assessing the wearable's capability to detect clinically or physiologically relevant events (e.g., physiological responses to stressors, pathological episodes, or treatment effects). This level directly evaluates the wearable's utility for answering research questions or clinical monitoring needs [88].
Visualization of Validation Workflow
Biomarker Validation Considerations
Analytical and Clinical Validation
For wearable biosensors targeting specific biomarkers, the validation framework must address both analytical and clinical performance. Biomarkers—defined as measurable indicators of normal biological processes, pathogenic processes, or biological responses to exposure or intervention—require rigorous validation to establish their clinical utility [89]. The validation approach differs significantly between prognostic biomarkers (which provide information about overall expected clinical outcomes regardless of therapy) and predictive biomarkers (which inform expected clinical outcomes based on specific treatment decisions) [89].
Table 2: Key Metrics for Biomarker Performance Evaluation
| Metric | Description | Interpretation | Application Context |
|---|---|---|---|
| Sensitivity | Proportion of true cases that test positive | Higher values reduce false negatives | Disease detection, screening |
| Specificity | Proportion of true controls that test negative | Higher values reduce false positives | Disease detection, screening |
| Positive Predictive Value | Proportion of test positive patients who actually have the disease | Function of disease prevalence | Diagnostic confirmation |
| Negative Predictive Value | Proportion of test negative patients who truly do not have the disease | Function of disease prevalence | Diagnostic confirmation |
| Area Under ROC Curve | Overall measure of how well marker distinguishes cases from controls | Ranges from 0.5 (coin flip) to 1.0 (perfect) | Overall diagnostic performance |
| Calibration | How well a marker estimates the risk of disease or event | Agreement between predicted and observed risks | Risk prediction models |
Prognostic biomarkers can be identified through properly conducted retrospective studies that use biospecimens collected from cohorts representing the target population. Identification typically involves a main effect test of association between the biomarker and the outcome in a statistical model [89]. In contrast, predictive biomarkers require identification in secondary analyses using data from randomized clinical trials, specifically through an interaction test between the treatment and the biomarker in a statistical model [89].
Methodological Safeguards Against Bias
Bias represents one of the greatest causes of failure in biomarker validation studies. Bias can enter a study during patient selection, specimen collection, specimen analysis, and patient evaluation [89]. Two crucial methodological safeguards must be implemented:
Randomization in biomarker discovery should control for non-biological experimental effects due to changes in reagents, technicians, machine drift, and other factors that can result in batch effects. Specimens from controls and cases should be assigned to testing platforms via random assignment, ensuring equal distribution of cases, controls, and specimen ages across experimental batches [89].
Blinding should be implemented by keeping individuals who generate the biomarker data from knowing the clinical outcomes. This prevents bias induced by unequal assessment of biomarker results and should be incorporated at every possible stage of the validation study [89].
Experimental Protocols
Signal Level Validation Protocol
Objective: To validate that the raw signal from the wearable biosensor sufficiently matches the reference device signal, accounting for potential time delays and scaling differences.
Materials:
- Wearable biosensor device under validation
- Approved reference device (device-specific based on measured parameter)
- Data acquisition system with synchronized timing
- Standardized calibration stimuli (if applicable)
Procedure:
- Simultaneously record signals from both wearable and reference devices for a minimum of 30 minutes under controlled conditions.
- Ensure proper synchronization of timing signals between devices.
- Apply appropriate signal preprocessing (filtering, artifact removal) consistently to both signals.
- Compute cross-correlation function between the two signals to assess similarity and identify systematic time delays.
- Test for mean difference between the two signals if cross-correlation is high (>0.9).
- If a mean difference is found, center the data around this mean to correct for bias.
- Assess systematic differences in variance that may require correction.
Statistical Analysis:
- Cross-correlation analysis with time displacement
- Paired t-test for mean differences
- F-test for variance differences
Decision Criteria:
- Cross-correlation coefficient > 0.9 indicates acceptable signal similarity
- Non-significant mean difference (p > 0.05) after correction
- Documentation of any necessary transformation equations for future applications
Parameter Level Validation Protocol
Objective: To validate that physiological parameters derived from the wearable biosensor demonstrate acceptable agreement with those derived from the reference standard.
Materials:
- Processed signals from wearable and reference devices
- Parameter extraction algorithms (identical for both devices when possible)
- Statistical analysis software with Bland-Altman implementation
Procedure:
- Derive target physiological parameters (e.g., heart rate, RMSSD, number of skin conductance responses) from both wearable and reference device signals using identical algorithms.
- For each parameter, create a Bland-Altman plot displaying the differences between the two measurements against their means.
- Calculate the mean difference (bias) and 95% limits of agreement (mean difference ± 1.96 × standard deviation of differences).
- Visually inspect the Bland-Altman plot for any systematic patterns or relationship between the differences and means.
- Compare the observed limits of agreement to pre-defined clinical acceptability boundaries.
Statistical Analysis:
- Bland-Altman analysis with calculation of bias and limits of agreement
- Intraclass correlation coefficient for consistency assessment
- Linear regression between wearable and reference parameters
Decision Criteria:
- Mean difference not statistically significantly different from zero
- Limits of agreement within clinically acceptable bounds
- Intraclass correlation coefficient > 0.75 indicating good reliability
Event Level Validation Protocol
Objective: To validate that the wearable biosensor can detect physiologically meaningful events or responses with sensitivity equivalent to the reference standard.
Materials:
- Parameter data from wearable and reference devices
- Controlled stimulus protocol for eliciting physiological responses
- Event detection algorithms
- Statistical analysis software
Procedure:
- Design a controlled protocol incorporating standardized stimuli (e.g., stress tests, cognitive tasks, physical maneuvers) expected to elicit measurable physiological responses.
- Collect simultaneous data from wearable and reference devices throughout the protocol.
- For each device, apply event detection algorithms to identify physiological responses to the standardized stimuli.
- Create event difference plots comparing the magnitude and timing of detected responses between devices.
- Statistically compare the detected response magnitudes between devices using appropriate tests.
Statistical Analysis:
- Event difference plots with confidence intervals
- Paired statistical tests (t-tests or non-parametric equivalents) for response magnitudes
- Sensitivity and specificity calculations for event detection
Decision Criteria:
- No statistically significant difference in response magnitudes between devices (p > 0.05)
- Equivalent detection of statistically significant responses to stimuli (both devices show p < 0.05 or both show p > 0.05)
- Documentation of any systematic differences in response characteristics
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagent Solutions for Wearable Biosensor Validation
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Reference Measurement Devices | Gold-standard comparison for validation | Device selection depends on target analyte (ECG for cardiac, laboratory analyzers for biomarkers) |
| Calibration Solutions | Standardize sensor responses across measurement sessions | Concentration series covering physiological range; matrix-matched to biofluid |
| Biorecognition Elements | Target-specific detection (enzymes, antibodies, aptamers) | Selection based on stability, specificity, and compatibility with wearable format |
| Flexible Substrate Materials | Conformable interfaces for body attachment | PDMS, polyethylene terephthalate, polyimide; selected for skin compatibility |
| Conductive Nanomaterials | Signal transduction enhancement | Graphene, carbon nanotubes; provide high surface area and excellent electron mobility |
| Microfluidic Components | Controlled biofluid sampling and transport | Channels, pumps, membranes for sweat, saliva, or tear collection |
| Immobilization Matrices | Secure biorecognition elements to sensor surface | Hydrogels, polymer films; maintain bioreceptor activity and stability |
| Signal Processing Algorithms | Extract meaningful parameters from raw data | Customized for specific sensor output and artifact characteristics |
Advanced Methodological Considerations
Validation in Uncontrolled Environments
A significant challenge in wearable biosensor validation involves demonstrating performance reliability in real-world, uncontrolled environments after establishing validity in laboratory settings. This requires additional methodological considerations:
Dynamic Signal Quality Assessment: Implementation of automated signal quality indices that continuously monitor data integrity during ambulatory use. These algorithms should detect motion artifacts, poor contact, and environmental interference that may compromise data validity [1].
Contextual Validation Protocols: Development of validation protocols that incorporate typical daily activities (e.g., walking, sleeping, eating, exercising) to assess device performance across diverse real-world contexts that generate varying types and levels of artifact [88].
Statistical Power and Sample Size Considerations
Adequate statistical power is crucial for robust validation studies. Key considerations include:
Pilot Testing: Conduct small-scale pilot studies to estimate effect sizes and variability parameters needed for formal sample size calculations.
Event Rate Considerations: For event-level validation, ensure sufficient statistical power by including adequate numbers of events or responses, not just participants.
Multilevel Modeling Approaches: Consider hierarchical or multilevel statistical models that appropriately account for nested data structures (e.g., repeated measurements within participants) common in wearable sensor validation studies.
The establishment of standardized evaluation frameworks is fundamental to advancing wearable biosensors from promising research tools to clinically accepted medical devices. The comprehensive three-level validation protocol presented here—encompassing signal, parameter, and event levels—provides a rigorous methodological foundation for demonstrating device reliability and clinical utility. By implementing these standardized protocols with appropriate statistical methods and decision criteria, researchers can generate comparable, conclusive evidence regarding wearable biosensor performance. This methodological rigor will accelerate the translation of wearable biosensing technologies into clinically impactful tools that enhance personalized healthcare through continuous physiological monitoring.
Wearable biosensors represent a transformative force in continuous health monitoring, enabling real-time, non-invasive tracking of physiological and biochemical parameters. This application note provides a comparative analysis of predominant biosensing technology types—electrochemical, optical, piezoelectric, and physical—delineating their operational principles, strengths, and inherent limitations. Structured for researchers and drug development professionals, the document includes standardized experimental protocols, a curated list of research reagents, and data visualization tools to facilitate the selection, development, and validation of biosensors for specific preclinical and clinical applications.
Wearable biosensors are compact, autonomous devices designed for continuous monitoring of biological signals. They typically consist of a bio-recognition element (e.g., enzymes, antibodies) that interacts with a specific analyte, a transducer that converts the biological interaction into a quantifiable electrical signal, and electronic circuitry for signal processing and wireless data transmission [90]. The convergence of advancements in flexible electronics, nanomaterials (particularly graphene), microfluidics, and wireless communication has propelled the development of highly sensitive, user-comfortable biosensors suitable for long-term monitoring in both controlled clinical trials and real-world environments [91] [57]. Their application is pivotal for advancing personalized medicine, managing chronic diseases, and enabling remote patient monitoring, thereby reducing healthcare costs and improving patient outcomes [63].
Comparative Analysis of Biosensor Technologies
The selection of an appropriate biosensing technology is contingent upon the target analyte, required sensitivity, specificity, and the intended use case. The following table provides a comparative summary of the major biosensor classes.
Table 1: Comparative Analysis of Major Biosensor Technologies
| Technology Type | Working Principle | Key Strengths | Primary Limitations | Ideal Use Cases |
|---|---|---|---|---|
| Electrochemical [91] | Measures electrical changes (current, potential, impedance) from electrochemical reactions of target analytes. | High sensitivity and selectivity for specific molecules; low cost; easily miniaturized. | Susceptible to biofouling; requires calibration; can be influenced by skin pH and temperature. | Continuous glucose monitoring (e.g., using glucose oxidase) [90]; detection of lactate, electrolytes, and other metabolites in sweat. |
| Optical [91] | Detects changes in light properties (absorption, fluorescence, scattering) due to analyte interaction. | Immunity to electromagnetic interference; potential for high spatial resolution. | Susceptible to ambient light; larger size for some form factors; challenges with motion artifacts. | Pulse oximetry (PPG) for heart rate and blood oxygen [92]; ring-type form factors for sleep monitoring [90]. |
| Piezoelectric [91] | Measures changes in mass, pressure, or mechanical stress via the piezoelectric effect (generation of an electric charge). | High sensitivity for mass-based detection; robust for physical sensing. | Sensitive to environmental vibrations; can be non-specific for biochemical sensing. | Monitoring physical activity, respiration rate, and muscle movement [91]. |
| Physical (PPG/ECG) [92] [36] | PPG uses light to detect blood volume changes; ECG measures the heart's electrical activity. | Well-established, non-invasive, continuous monitoring of vital signs. | PPG accuracy affected by motion, skin pigmentation, tattoos [92]; signal quality dependent on skin contact. | Cardiovascular health monitoring, arrhythmia detection (e.g., AFib), hypertension risk assessment [92] [36]. |
The following diagram illustrates the generic workflow of a wearable biosensor, from signal acquisition to data delivery, which is common across different technology types.
Diagram 1: Generalized Workflow of a Wearable Biosensor
Quantitative Data and Market Outlook
The PPG biosensors market, a prominent segment of optical biosensors, is projected to grow from USD 648.5 million in 2025 to USD 3,064.8 million by 2035, reflecting a compound annual growth rate (CAGR) of 16.8% [92]. This growth is fueled by the integration of biosensors into consumer wearables and clinical remote patient monitoring (RPM) systems. Regionally, the Asia-Pacific market is anticipated to be the fastest-growing, driven by affordable consumer wearables and increasing telehealth adoption [92]. The global wearable biosensors market as a whole is also expanding significantly, expected to grow from USD 31,250 million in 2025 to USD 57,521 million by 2033, at a CAGR of 7.925% [93].
Table 2: Projected Regional CAGRs for PPG Biosensors Market (2025-2035) [92]
| Region | Projected CAGR (2025-2035) |
|---|---|
| United States | 17.1% |
| United Kingdom | 16.5% |
| European Union | 16.7% |
| Japan | 16.2% |
| South Korea | 17.3% |
Experimental Protocols for Key Applications
Protocol: Development and Validation of a Graphene-Based Electrochemical Sweat Sensor
This protocol outlines the steps for creating a flexible biosensor to detect metabolites like glucose or lactate in sweat [91] [57].
1. Sensor Fabrication:
- Substrate Preparation: Clean a flexible substrate (e.g., Polydimethylsiloxane (PDMS) or polyethylene terephthalate (PET)) with ethanol and deionized water.
- Electrode Patterning: Deposit a conductive graphene ink onto the substrate using screen-printing or inkjet printing to form the working, counter, and reference electrodes.
- Functionalization: Immobilize the specific biorecognition element (e.g., the enzyme glucose oxidase for glucose sensing) onto the working electrode. This can be achieved via drop-casting followed by cross-linking with glutaraldehyde or by using Nafion membranes. Graphene's large surface area facilitates high enzyme loading, enhancing sensitivity [57].
2. In Vitro Calibration:
- Connect the fabricated sensor to a potentiostat.
- Immerse the sensor in a series of standard solutions with known concentrations of the target analyte (e.g., 0.1 mM to 5.0 mM glucose in artificial sweat buffer).
- Record the amperometric or voltammetric response at a fixed potential.
- Plot a calibration curve of current response versus analyte concentration to determine the sensor's sensitivity, linear range, and limit of detection (LOD).
3. On-Body Validation:
- Secure the sensor on the volunteer's skin (e.g., forearm) using a biocompatible adhesive. Ensure good contact between the sensor and the skin surface for sweat sampling.
- The sensor can be integrated with a microfluidic channel to wick sweat to the sensing area [91].
- Induce sweat through exercise or pilocarpine iontophoresis.
- Simultaneously collect sweat samples for validation using a standard reference method (e.g., HPLC).
- Transmit the sensor's data wirelessly to a smartphone or data logger for real-time monitoring and analysis.
Protocol: Implementing AI for Arrhythmia Detection from a PPG Signal
This protocol describes how to process PPG data from a wrist-worn device to detect atrial fibrillation (AFib) using machine learning [92] [36].
1. Data Acquisition and Preprocessing:
- Collect raw PPG signals from a biosensor module (e.g., using infrared or green LEDs and a photodetector) at a suitable sampling rate (e.g., >100 Hz).
- Apply digital filters (e.g., bandpass filter 0.5 - 5 Hz) to remove baseline wander and high-frequency noise.
- Use algorithms to identify and correct motion artifacts, a significant challenge for PPG signals [92].
2. Feature Extraction:
- Segment the cleaned PPG signal into individual pulses.
- From each pulse, extract features relevant to cardiovascular function, such as:
- Pulse Rate Variability (PRV): Analogous to heart rate variability.
- Pulse Shape Characteristics: Crest time, diastolic time, pulse area, and second derivative features.
- Frequency-Domain Features: Power spectral density in relevant bands.
3. Model Training and Validation:
- Label the data segments with ground truth from simultaneous ECG recordings.
- Train a machine learning classifier (e.g., Convolutional Neural Network, Support Vector Machine) using the extracted features to distinguish between normal sinus rhythm and arrhythmia (e.g., AFib). Studies have achieved accuracies exceeding 98% for such binary classification tasks using deep learning models on physiological data [36].
- Validate the model's performance on a separate, held-out test dataset using metrics like accuracy, sensitivity, specificity, and F1-score.
The following diagram conceptualizes this AI-enhanced signal processing pipeline.
Diagram 2: AI-Driven PPG Signal Processing for Arrhythmia
The Scientist's Toolkit: Research Reagent Solutions
The development and functionality of advanced wearable biosensors rely on a suite of specialized materials and reagents.
Table 3: Essential Research Reagents and Materials for Wearable Biosensor Development
| Reagent/Material | Function in Biosensor Development | Key Characteristics |
|---|---|---|
| Graphene & CNTs [91] [57] | Sensing electrode material; transducer element. | High electrical conductivity, large surface area, mechanical flexibility, biocompatibility. Enhances sensor sensitivity. |
| Glucose Oxidase [90] | Bio-recognition element for glucose biosensors. | Enzyme that catalyzes the oxidation of glucose, producing an electrical signal proportional to concentration. |
| Polydimethylsiloxane (PDMS) [91] | Flexible substrate and microfluidic channel material. | Biocompatible, transparent, gas-permeable, and easily molded. Ideal for skin-conformable patches. |
| Conductive Inks (Ag/CNT) [91] | Printing flexible electrodes and circuits on substrates. | Provide conductivity on flexible materials; enable mass production via screen or inkjet printing. |
| Nafion Membrane | Selective permeable membrane on electrodes. | Reduces interference from anions (e.g., ascorbate, urate) in electrochemical sensors, improving selectivity. |
| Biocompatible Hydrogels [91] | Interface between sensor and skin for biofluid sampling. | Hydrated polymer that facilitates the transport of analytes from sweat to the sensor while improving skin comfort. |
Wearable biosensors are rapidly evolving from fitness trackers to clinically validated diagnostic tools. The optimal technology choice is application-dependent: electrochemical sensors excel in specific molecular detection, optical PPG sensors dominate vital sign monitoring, and piezoelectric sensors are robust for physical activity tracking. Future development will be shaped by trends toward multimodal sensing (combining PPG with ECG and temperature) [92], the integration of AI at the edge for real-time analytics [36], and the use of advanced nanomaterials like graphene to overcome current limitations in sensitivity and flexibility [57]. For researchers and drug developers, addressing challenges related to data privacy, regulatory approval, accuracy across diverse populations, and user adoption will be critical for translating these promising technologies from the lab into mainstream clinical practice and large-scale clinical trials [63].
Market Data Analysis
The wearable biosensor market is experiencing robust global growth, fueled by technological advancements and rising demand for continuous health monitoring solutions. The data, compiled from recent market analyses, shows some variation in specific figures due to differing segment definitions and reporting timelines, but a consistent and strong growth trajectory is evident.
Table 1: Global Wearable Biosensor Market Size and Projections
| Market Segment / Scope | Base Year & Value | Projection Year & Value | Compound Annual Growth Rate (CAGR) | Source / Notes |
|---|---|---|---|---|
| Overall Biosensors Market | USD 34.5 billion (2025) | USD 54.4 billion (2030) | 9.5% (2025-2030) | Includes both wearable and non-wearable biosensors [31]. |
| Wearable Biosensors Market (Projection 1) | USD 72.579 billion (2025) | USD 167.81 billion (2034) | 9.76% (2025-2034) | [94] |
| Wearable Biosensors Market (Projection 2) | USD 1,875.08 million (2024) | USD 9,177.65 million (2033) | 22.4% (2025-2033) | Represents a specific segment of the market [95]. |
| Wireless Wearable Biosensor Market | USD 12.5 billion (2025) | USD 30.2 billion (2032) | 10.5% (2025-2032) | [96] |
Table 2: Key Market Drivers, Trends, and Challenges
| Category | Detail | Supporting Data / Examples |
|---|---|---|
| Primary Drivers | Rising prevalence of chronic diseases & aging population [94] [95] | The global population aged 60+ is expected to rise by 56% by 2030 [94]. |
| Demand for remote & continuous patient monitoring [1] [31] | Over 50% of healthcare professionals favor continuous monitoring devices [94]. | |
| Key Trends | Integration of AI and Machine Learning [91] [95] | Nearly 60% of new wearable biosensors integrate AI algorithms [94]. |
| Miniaturization and multi-sensor platforms [91] [1] | Over 55% of newly approved wearable biosensors in 2023 integrated multi-sensor platforms [94]. | |
| Expansion to non-invasive biofluid analysis [1] [97] | Focus on sweat, tears, saliva, and interstitial fluid (ISF) [1]. | |
| Major Challenges | Data Security and Privacy [94] [95] | ~40% of consumers cite privacy and data security as key adoption barriers [94]. |
| Regulatory Hurdles [1] [31] | Long certification and approval cycles from bodies like the FDA [31]. | |
| Sensor Accuracy and Reliability [1] | Need for high sensitivity and stability in uncontrolled, real-world conditions [1]. |
Application Notes for Research and Development
Note 1: Multiplexed Sensing in Epidermal Biofluids
Objective: To enable the simultaneous, real-time monitoring of multiple biomarkers in sweat for comprehensive metabolic and electrolyte status assessment [91] [1].
Background: Sweat is a complex biofluid containing metabolites (e.g., glucose, lactate), electrolytes (e.g., Na+, K+), and hormones. Its composition provides a window into the body's physiological state. Recent advances in flexible electronics and microfluidics have made it possible to create epidermal (skin-worn) sensors that can collect and analyze sweat in real-time [1]. Multiplexing is critical because it provides a more correlated health picture than single-analyte measurements.
Experimental Protocol: Lactate and Sodium Ion Co-detection in Simulated Sweat
Workflow Overview:
Step 1: Sensor Fabrication
- Microfluidic Layer: Fabricate a polydimethylsiloxane (PDMS) layer using soft lithography. This layer will act as a sweat collection and transport channel [98].
- Electrode Patterning: Use photolithography or screen printing to pattern a three-electrode system (working, reference, counter) onto a flexible polyethylene terephthalate (PET) substrate. Gold (Au) and carbon inks are commonly used [91] [98].
- Bioreceptor Immobilization:
Step 2: Device Assembly & Encapsulation
- Bond the PDMS microfluidic layer to the electrode-patterned PET substrate using oxygen plasma treatment to create a permanent seal [98].
- Ensure the microfluidic channels are perfectly aligned over the functionalized working electrodes.
Step 3: Calibration & Validation
- Connect the sensor to a potentiostat for electrochemical measurements (e.g., Amperometry for lactate, Potentiometry for Na+).
- Calibrate with standard solutions of known lactate (e.g., 0.1-20 mM) and sodium (e.g., 10-100 mM) concentrations to establish a standard curve [1].
Step 4: Sample Analysis & Data Acquisition
- Introduce an artificial sweat sample into the microfluidic inlet.
- Monitor the amperometric current (for lactate) and potentiometric potential (for Na+) simultaneously as the sample wicks over the electrodes.
- Correlate the generated electrical signals to analyte concentrations using the calibration curves.
Note 2: Nucleic Acid-Based Detection for Pathogen Monitoring
Objective: To integrate nucleic acid (NA) assays, such as those using aptamers or CRISPR-Cas, into wearable biosensors for the highly specific detection of pathogens or proteins [98].
Background: Traditional wearable biosensors have relied on enzymes and antibodies. Nucleic acid-based bioreceptors offer advantages in stability, scalability, and programmability [98]. Aptamers (synthetic single-stranded DNA/RNA) can be selected to bind specific targets with high affinity, while CRISPR-Cas systems provide powerful signal amplification.
Experimental Protocol: Aptamer-Based Detection of a Model Protein
Workflow Overview:
Step 1: Aptamer Functionalization
- Immobilize a thiol-modified DNA aptamer (specific to your target, e.g., immunoglobulin E or a viral protein) onto the gold working electrode via gold-thiol self-assembled monolayer chemistry [98].
Step 2: Baseline Measurement
- Using electrochemical impedance spectroscopy (EIS), measure the baseline electron transfer resistance (Rₑₜ) of a redox probe (e.g., [Fe(CN)₆]³⁻/⁴⁻) in buffer. The aptamer layer presents a slight barrier, resulting in a measurable Rₑₜ.
Step 3: Target Binding
- Introduce a solution containing the target protein to the sensor surface.
Step 4: Signal Transduction
- Upon binding to the target, the aptamer may undergo a conformational change or the large protein may create a physical barrier. This further hinders the redox probe's access to the electrode surface, causing a significant increase in Rₑₜ.
Step 5: Data Acquisition
- The magnitude of the increase in Rₑₜ is proportional to the concentration of the target protein in the sample.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for Wearable Biosensor Development
| Item | Function/Description | Example Applications |
|---|---|---|
| Flexible Substrates (PET, PI, PDMS) | Provide a soft, stretchable, and conformal base for sensor construction, ensuring comfort and continuous skin contact [91] [98]. | Epidermal patches, smart textiles [1]. |
| Conductive Inks (Carbon, Silver/Silver Chloride) | Form flexible electrodes for electrochemical sensing and electrical connectivity. Ag/AgCl is crucial for stable reference electrodes [91] [98]. | Screen-printed electrodes (SPEs) for metabolite detection [91]. |
| Bioreceptors (Enzymes, Aptamers, Antibodies) | The core recognition element that provides specificity to the target analyte (e.g., Glucose Oxidase for glucose) [1] [98]. | Enzymatic detection of lactate; aptamer-based detection of cytokines [91] [98]. |
| Nanomaterials (Graphene, CNTs, MXenes) | Enhance sensor sensitivity and selectivity due to their high surface area and excellent electrical/electrochemical properties [91] [97]. | Nanocomposite-based pressure sensors; high-sensitivity electrochemical electrodes [97]. |
| Redox Probes ([Fe(CN)₆]³⁻/⁴⁻) | Mediate electron transfer in electrochemical biosensors, especially when direct electron transfer from the bioreceptor is inefficient [98]. | Used in EIS and voltammetry-based biosensing assays [98]. |
| Microfluidic Master Mold (SU-8 Photoresist) | Used in soft lithography to create the negative pattern for producing PDMS microchannels for biofluid handling [98]. | Fabrication of sweat collection and routing channels on a sensor patch [1] [98]. |
Regulatory Pathways and FDA Approval for Medical-Grade Wearables
The evolution of wearable technology from consumer fitness trackers to clinical-grade medical devices has significantly altered the regulatory landscape. For researchers and drug development professionals, understanding U.S. Food and Drug Administration (FDA) pathways is crucial for integrating these devices into clinical research and therapeutic development. Medical-grade wearables are distinguished from general wellness devices by intended use—specifically, claims to diagnose, monitor, or treat disease—which places them under FDA regulatory scrutiny [99] [100]. The FDA encourages innovation through several policy frameworks while ensuring that devices marketed for medical purposes demonstrate safety and effectiveness through rigorous evaluation [101] [102]. This document outlines the structured regulatory pathways, detailed experimental protocols for validation, and key considerations for successful development and deployment of medical-grade wearables within clinical research settings.
FDA Regulatory Frameworks and Device Classification
Device Classification and Associated Regulatory Pathways
The FDA classifies medical devices based on risk, which determines the regulatory pathway required for marketing. This classification system is foundational for research and development planning [99] [100].
Table: FDA Medical Device Classification and Associated Pathways
| Device Class | Risk Level | Regulatory Controls | Example Pathway | Typical Review Timeline |
|---|---|---|---|---|
| Class I | Low to Moderate | General Controls (e.g., labeling, manufacturing standards) | Mostly Exempt (may not require premarket submission) | N/A |
| Class II | Moderate | General Controls & Special Controls (e.g., performance standards, post-market surveillance) | 510(k) Premarket Notification (Demonstration of Substantial Equivalence to a predicate device) | 90 to 180 days |
| Class III | High | General Controls & Premarket Approval (PMA) (Requires independent demonstration of safety and effectiveness) | Premarket Approval (PMA) (Requires extensive scientific evidence, typically from clinical trials) | 180 days to several years |
Most wearable medical devices, such as those for remote patient monitoring, fall into Class II and typically follow the 510(k) pathway [99]. High-risk devices that support or sustain human life, such as wearable cardioverter defibrillators, are generally Class III devices requiring the most stringent Premarket Approval (PMA) pathway [99] [103].
The General Wellness Policy and Software as a Medical Device (SaMD)
For developers, distinguishing between a wellness product and a medical device is critical. The FDA's General Wellness Policy outlines that low-risk products intended only for general wellness efforts, such as tracking physical activity or sleep patterns without reference to a disease, are not considered medical devices [100]. However, if a wearable's intended use crosses into disease-related claims—for example, "detects atrial fibrillation" or "manages hypertension"—it becomes subject to FDA regulation [100].
Many advanced wearables are considered Software as a Medical Device (SaMD), where the software function itself performs the medical purpose. The FDA aligns with the International Medical Device Regulators Forum (IMDRF) framework for SaMD, which emphasizes a risk-based approach focused on the significance of the information provided by the software to the healthcare decision [100].
Strategic Approach to FDA Submission and Key Considerations
Premarket Submission Pathways in Detail
Navigating the correct premarket pathway is a critical strategic decision. The following diagram illustrates the key decision points and processes for the two primary pathways.
Premarket Notification 510(k) The 510(k) pathway requires a manufacturer to demonstrate that their device is "substantially equivalent" to a legally marketed predicate device [99]. This does not always require new clinical trials if performance testing against the predicate is sufficient. However, for novel wearables, a clinical study is often necessary to establish equivalent performance. The submission must include detailed descriptions of the device's intended use, technological characteristics, and performance testing data [99] [100].
Premarket Approval (PMA) The PMA pathway is the most demanding, requiring valid scientific evidence to affirm the device's safety and effectiveness for its intended use [99]. This typically includes data from one or more prospective clinical investigations and entails a comprehensive review of the device's design, manufacturing, and labeling. The FDA inspection of the manufacturer's facilities also forms part of the PMA process.
Special Considerations for AI-Enabled Wearables
The FDA has issued specific draft guidance for AI-enabled devices, emphasizing a total product lifecycle approach [104]. Key recommendations include:
- Transparency and Description: Labeling should comprehensively explain the AI's role in the device's function, including model inputs, outputs, development, and known limitations [104].
- Bias Evaluation and Mitigation: Development datasets must be representative of the intended population across demographics like race, ethnicity, sex, and age. Sponsors must collect evidence to evaluate performance equity across all relevant demographic groups [104].
- Predetermined Change Control Plans (PCCPs): The FDA encourages using PCCPs to pre-specify and obtain authorization for future, intended modifications to AI models, facilitating iterative improvement without requiring a new submission for each change [104].
Quality Systems and Human Factors
Manufacturers of regulated wearables must comply with the Quality System Regulation (QSR) under 21 CFR Part 820, which encompasses design controls, risk management, and production processes [100]. The FDA is transitioning to the Quality Management System Regulation (QMSR), harmonizing with ISO 13485 [100].
Human factors engineering is critical for wearable devices, where usability directly impacts safety and effectiveness. FDA requires usability validation testing to demonstrate that the device can be used by the target population in the actual use environment without critical use errors [100].
Experimental Protocols for Clinical Validation
Robust clinical validation is the cornerstone of any FDA submission. The following workflow outlines the key stages of this process.
Protocol Development for Analytical Validation
Objective: To verify the wearable device's technical performance against a reference standard in a controlled setting.
Key Methodologies:
- Accuracy and Precision: Conduct repeated measurements across the device's operating range using phantoms or simulators. Compare results to a traceable reference standard. Report mean absolute error, root mean square error, and coefficient of variation [105].
- Limit of Detection (LOD) and Limit of Quantification (LOQ): Determine the lowest signal concentration the device can reliably detect (LOD) and quantify with stated precision (LOQ) [105].
- Interference and Robustness Testing: Expose the device to potential interferents (e.g., motion, ambient light, skin tone variations) and document performance impact. A key focus for optical sensors (PPG) is validation across diverse skin tones to mitigate algorithmic bias [104].
Protocol for Clinical Validation (Pivotal Study)
Objective: To demonstrate the device's safety and effectiveness for its intended use in the target population.
Key Methodologies:
- Study Design: A prospective, single- or multi-center trial is standard. A supervised study may be required where participants use the test and reference devices simultaneously in a clinic. An unsupervised study might be acceptable for home-use devices, requiring careful remote monitoring and data integrity protocols [100].
- Participant Cohort: Recruit a representative sample of the intended use population, ensuring diversity in age, sex, race, ethnicity, and relevant clinical characteristics (e.g., BMI, disease severity). The Apple Hypertension Notification Feature (HTNF) study, for example, enrolled a large, diverse cohort of over 2,000 participants [100].
- Reference Standard: Use an FDA-cleared or clinically accepted gold-standard device as a comparator. For example, a 12-lead ECG or Holter monitor for arrhythmia detection, or a lab-based blood analyzer for glucose monitoring [106] [105].
- Statistical Analysis Plan (SAP): Pre-specify primary and secondary endpoints, success criteria, and statistical methods. Common endpoints include sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). For continuous measures, mean absolute relative difference (MARD) and confidence intervals are critical [106] [105].
Table: Key Performance Metrics for Clinical Validation of Wearables
| Metric | Formula | Interpretation & Benchmark |
|---|---|---|
| Sensitivity (Recall) | True Positives / (True Positives + False Negatives) | Measures ability to correctly identify condition. Target: >90-95% for critical alerts. |
| Specificity | True Negatives / (True Negatives + False Positives) | Measures ability to correctly identify absence of condition. Target: >90-95%. |
| Positive Predictive Value (PPV) | True Positives / (True Positives + False Positives) | Probability that a positive result is truly positive. Highly dependent on prevalence. |
| Negative Predictive Value (NPV) | True Negatives / (True Negatives + False Negatives) | Probability that a negative result is truly negative. Highly dependent on prevalence. |
| Mean Absolute Relative Difference (MARD) | (1/n) * Σ⎮(Valuetest - Valueref) / Value_ref⎮ | Common metric for glucose monitors. Lower values indicate higher accuracy (<10% is excellent). |
| Bland-Altman Analysis | Plots difference between two measures vs. their average | Visualizes bias and limits of agreement between test device and reference standard. |
The Scientist's Toolkit: Research Reagent Solutions
This table details essential materials and tools required for the development and validation of wearable biosensors.
Table: Essential Research Toolkit for Wearable Biosensor Development
| Category / Item | Specific Examples | Function & Application in Research |
|---|---|---|
| Reference Standard Devices | 12-lead ECG Machine, Holter Monitor; Clinical Grade Blood Pressure Monitor; YSI or similar lab blood analyzer | Serves as the non-invasive gold-standard comparator for validating the accuracy of the wearable device's physiological measurements in clinical studies [106] [105]. |
| Signal Simulators & Phantoms | PPG Waveform Simulator; ECG Signal Generator; Motion Platform | Generates precise, reproducible physiological signals with known parameters for initial bench testing and analytical validation of sensors and algorithms, free from biological variability [105]. |
| Data Acquisition & Analysis Software | MATLAB, Python (with SciPy/NumPy); LabVIEW; Cloud Analytics Platforms (e.g., AWS, Google Cloud) | Used for signal processing, algorithm development, feature extraction, and statistical analysis of large, continuous datasets generated by wearable devices during validation studies [107] [105]. |
| Cybersecurity Testing Tools | Static/Dynamic Application Security Testing (SAST/DAST); Network Protocol Analyzers (e.g., Wireshark) | Identifies vulnerabilities in device software, firmware, and data transmission protocols to ensure compliance with FDA cybersecurity guidance and protect patient data [99] [100]. |
Navigating the FDA regulatory landscape for medical-grade wearables demands a systematic and evidence-based approach. Success hinges on a clear definition of intended use, selection of the appropriate regulatory pathway, and execution of rigorous clinical validation that addresses potential biases and real-world usability. For researchers and drug developers, these devices offer unprecedented opportunities to capture dense, real-world physiological data, enabling novel endpoints in clinical trials and more personalized therapeutic interventions [107] [105]. By integrating regulatory strategy early in the development lifecycle and engaging with the FDA through pre-submission meetings, innovators can transform regulatory compliance from a hurdle into a strategic advantage, ultimately accelerating the delivery of trustworthy wearable technologies to the market.
The transition of wearable biosensors from research laboratories to the commercial market represents a critical phase in the evolution of digital health. These devices, which integrate biological recognition elements with physico-chemical transducers to provide continuous, real-time physiological data, have seen growing adoption for healthcare monitoring and chronic disease management [1] [74]. This application note examines prominent commercial successes in the wearable biosensor landscape, analyzing the key factors that have driven their market acceptance and the lessons learned from their development and deployment. Framed within broader research on wearable biosensors for continuous health monitoring, this analysis provides researchers, scientists, and drug development professionals with actionable insights into the technical, regulatory, and commercial considerations essential for successful translation of biosensing technologies. The case studies presented herein focus on devices that have achieved significant clinical impact and market penetration, with particular attention to their technological innovation, validation pathways, and integration into healthcare systems.
Commercial Success Stories in Wearable Biosensing
Analysis of Marketed Wearable Biosensor Products
Table 1: Commercial Wearable Biosensors for Health Monitoring
| Product/Company | Analyte/Sample | Wearable Platform | Monitoring Mechanism | Key Advantages | Regulatory Status/ Market Position |
|---|---|---|---|---|---|
| Freestyle Libre (Abbott) | Glucose in ISF | Patch-type | Electrochemical | 14-day wear, no fingerstick calibration | FDA approved; Market leader in ISF glucose monitoring |
| Dexcom G6 CGM (Dexcom) | Glucose in ISF | Patch-type | Electrochemical | Real-time alerts, compatible with insulin delivery systems | FDA approved; Widely used in diabetes management |
| Eversense (Senseonics) | Subcutaneous ISF glucose | Implantable | Fluorescence | 90-day continuous use, on-body vibratory alerts | FDA approved; First long-term implantable CGM |
| GlucoWatch (Cygnus) | Glucose in ISF | Watch-type | Electrochemical (reverse iontophoresis) | Non-invasive sampling | FDA approved but retracted from market; Valuable lessons from commercial failure |
Key Success Factors and Technical Innovations
The commercial successes in continuous glucose monitoring (CGM) demonstrate several critical technological advancements. The Freestyle Libre system revolutionized glucose monitoring by introducing a factory-calibrated sensor that eliminated the need for routine fingerstick calibration, significantly improving user compliance [1]. Its patch-type design incorporating a flexible filament electrode for interstitial fluid (ISF) access represented a major innovation in minimally invasive sampling. The system's 14-day wear duration addressed a key user concern regarding frequent device changes.
The Dexcom G6 system advanced the field through its real-time data transmission capabilities and interoperability with automated insulin delivery systems [1]. This integration capability has been crucial for developing closed-loop diabetes management systems. The device's alert systems for hypo- and hyperglycemic events provide critical safety features for patients.
Eversense took a fundamentally different approach as the first long-term implantable CGM, utilizing a fluorescent sensing mechanism rather than the electrochemical detection used by most competitors [1]. Its 90-day wear time significantly reduces the burden of frequent sensor replacements, while its on-body vibratory alerts provide discrete notification of glucose excursions even when the mobile display is not accessible.
The GlucoWatch biographer, while ultimately unsuccessful commercially, introduced the innovative concept of non-invasive glucose sampling through reverse iontophoresis [1] [74]. Despite its market withdrawal due to issues with skin irritation and reliability, it provided valuable proof-of-concept for alternative sampling methods that continue to influence the field.
Experimental Protocols and Methodologies
Protocol: In Vivo Performance Validation of Wearable Biosensors
Objective: To evaluate the analytical and clinical performance of wearable biosensors in accordance with regulatory requirements for market approval.
Materials:
- Wearable biosensor prototypes (n≥40)
- Reference analyzer (e.g., YSI 2300 STAT Plus for glucose)
- Venous blood collection supplies
- Controlled conditions facility
- Data recording system
Procedure:
- Participant Recruitment: Enroll 100-150 participants representing the target population (e.g., patients with diabetes for CGM).
- Sensor Deployment: Apply biosensors according to manufacturer instructions by trained clinicians.
- Reference Sampling: Collect venous blood samples at regular intervals (every 15 minutes initially, extending to every 30-60 minutes as values stabilize).
- Comparative Analysis: Conduct paired measurements between sensor readings and reference values across clinically relevant ranges.
- Statistical Evaluation: Calculate mean absolute relative difference (MARD), consensus error grid analysis, and correlation coefficients.
- Adverse Event Monitoring: Document any skin irritation, discomfort, or device failures throughout the study period.
Validation Parameters:
- Accuracy: MARD <10% generally required for clinical use [1]
- Precision: Coefficient of variation <10% across multiple sensors/lots
- Stability: Consistent performance throughout claimed wear duration
- User Evaluation: Feedback on comfort, ease of use, and reliability
Protocol: Biochemical Recognition Element Integration
Objective: To immobilize biological recognition elements (enzymes, antibodies, aptamers) onto transducer surfaces while maintaining bioactivity and stability.
Materials:
- Flexible electrode substrates (e.g., carbon, gold)
- Biorecognition elements (glucose oxidase, antibodies, etc.)
- Cross-linking reagents (glutaraldehyde, EDC/NHS)
- Polymer matrices (Nafion, polyurethane, chitosan)
- Phosphate buffered saline (PBS), pH 7.4
Procedure for Enzyme-Based Sensors (e.g., Glucose):
- Electrode Pretreatment: Clean and functionalize electrode surfaces using plasma treatment or electrochemical activation.
- Enzyme Immobilization:
- Prepare enzyme solution (e.g., 100 U/μL glucose oxidase in PBS)
- Mix with cross-linker (0.25% glutaraldehyde) and polymer matrix (1% Nafion)
- Deposit 2-5 μL mixture onto electrode surface
- Allow to cross-link for 24 hours at 4°C
- Membrane Application: Apply additional permselective membranes (e.g., polyurethane) to limit interferent access.
- Performance Verification: Test sensor response in standard solutions containing target analyte and potential interferents.
Critical Considerations:
- Maintain enzyme activity during immobilization process
- Ensure uniform coating thickness for reproducible response
- Optimize membrane permeability for target analyte selectivity
- Validate stability under storage and operational conditions
Signaling Pathways and Experimental Workflows
Biosensing Principle and Signal Transduction
Diagram Title: Wearable Biosensor Signal Transduction
Product Development Workflow
Diagram Title: Biosensor Commercialization Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Wearable Biosensor Development
| Category | Specific Reagents/Materials | Function | Example Applications |
|---|---|---|---|
| Biorecognition Elements | Glucose oxidase, Lactate oxidase, Antibodies, Aptamers | Selective target binding | Enzyme-based sensors, Immunosensors, Aptasensors |
| Transducer Materials | Carbon nanotubes, Graphene, Conductive polymers, Metal nanoparticles | Signal transduction | Electrode fabrication, enhancing electron transfer |
| Substrate Materials | Polydimethylsiloxane (PDMS), Polyimide, Polyethylene terephthalate (PET) | Flexible support | Conformal skin contact, wearable patches |
| Immobilization Matrices | Nafion, Chitosan, Polyurethane, Hydrogels | Biocompatible encapsulation | Enzyme stabilization, interferent exclusion |
| Reference Electrodes | Ag/AgCl inks, KCl electrolytes | Stable potential reference | Electrochemical cell completion |
| Microfluidic Components | Hydrogel plugs, Capillary channels, Micropumps | Biofluid transport | Sweat collection, sample delivery |
Critical Lessons from Commercial Experience
Technical and User-Centric Design Factors
Successful commercial wearable biosensors have demonstrated that technical performance must align with user needs for widespread adoption. The factory calibration implemented in the Freestyle Libre system addressed a significant usability barrier by eliminating the need for user-initiated calibrations, which was a limitation of earlier systems [1]. This innovation came through understanding that usability barriers could limit adoption even for technically sound devices.
The case of Eversense demonstrates the importance of matching technology to clinical needs. While the requirement for a minor implantation procedure presents a barrier, the extended 90-day wear time provides sufficient value that users accept this trade-off [1]. This illustrates the importance of clinical value proposition in technology adoption.
The failure of GlucoWatch provides cautionary insights regarding real-world reliability. While the device achieved regulatory approval based on clinical data, issues with skin irritation and measurement reliability during sweating limited practical utility [1]. This highlights that laboratory performance does not always translate to real-world conditions, and extensive field testing is essential.
Regulatory and Commercialization Strategy
The successful commercial products have navigated complex regulatory pathways by designing specifically for regulatory requirements from early development stages [108]. This includes implementing robust quality control systems during manufacturing and designing validation studies that adequately address regulatory concerns.
The razor-and-razor-blade business model has proven particularly effective for wearable biosensors, where the primary revenue comes from ongoing sales of consumable sensors rather than the reusable reader [109]. This model aligns well with the continuous monitoring value proposition of these devices.
Reimbursement strategy has been a critical success factor, particularly in the United States market. Demonstration of clinical utility and economic benefits through well-designed health economic studies has been essential for securing insurance coverage [108]. Products like Dexcom G6 have successfully navigated this pathway by generating evidence showing reduced hypoglycemic events and hospitalizations.
The commercial landscape for wearable biosensors provides valuable case studies in successful translation of biomedical technologies from laboratory concepts to clinical implementation. The successes of systems like Freestyle Libre, Dexcom G6, and Eversense highlight the importance of addressing real user needs, ensuring reliability in real-world conditions, and navigating complex regulatory and reimbursement pathways. These examples demonstrate that technical innovation must be coupled with thoughtful implementation strategy to achieve commercial success. As the field advances toward monitoring increasingly diverse biomarkers beyond glucose, these lessons will inform the development of next-generation wearable biosensors for comprehensive health monitoring. For researchers in this field, attention to both technological innovation and the practical considerations outlined in these case studies will enhance the likelihood of successful translation and clinical impact.
Conclusion
Wearable biosensors represent a paradigm shift in healthcare, moving from episodic check-ups to continuous, personalized health monitoring. The synthesis of foundational research, advanced applications, and rigorous validation efforts underscores their potential to revolutionize therapeutic drug monitoring, chronic disease management, and preventive care. Key takeaways include the critical role of material science in enhancing wearability, the power of AI in transforming raw data into actionable insights, and the importance of standardized performance metrics for clinical trust. For researchers and drug development professionals, the future direction is clear: the next frontier lies in developing robust, multi-analyte sensing systems that are validated in large-scale clinical trials. The convergence of wearable biosensors with digital health platforms and AI analytics will not only accelerate personalized medicine but also create a new ecosystem for decentralized clinical trials and real-world evidence generation, fundamentally reshaping the landscape of biomedical research and patient care.
References
- 1. for healthcare monitoring - PMC Wearable biosensors [https://pmc.ncbi.nlm.nih.gov/articles/PMC8183422/]
- 2. Advances in Medical Wearable Biosensors: Design, Fabrication and Materials Strategies in Healthcare Monitoring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8746599/]
- 3. Nanozyme-based colorimetric biosensor with a systemic quantification algorithm for noninvasive glucose monitoring [https://www.thno.org/v12p6308.htm]
- 4. Deep Learning-Enhanced Polymer-Based Wearable For... Biosensors [https://journals.stmjournals.com/jopc/article=2025/view=230426/]
- 5. Fusing Wearable Biosensors with Artificial Intelligence for Mental Health Monitoring: A Systematic Review [https://www.mdpi.com/2079-6374/15/4/202]
- 6. Technologies and emerging trends in wearable biosensing [https://pubmed.ncbi.nlm.nih.gov/40921536/]
- 7. Frontiers | Editorial: Wearable biosensing devices [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1574786/full]
- 8. Wearable Biosensors: An Alternative and Practical Approach in Healthcare and Disease Monitoring - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7867046/]
- 9. Rhythms – Normal Patterns • LITFL • ECG Library Diagnosis Pacemaker [https://litfl.com/pacemaker-rhythms-normal-patterns/]
- 10. All-in-One Self-Powered Wearable : Redefining... Biosensors [https://www.linkedin.com/pulse/all-in-one-self-powered-wearable-biosensors-redefining-ajayan-j-xgobc]
- 11. Printable molecule-selective nanoparticles enable mass... | ScienceDaily [https://www.sciencedaily.com/releases/2025/02/250203142404.htm]
- 12. A wearable electrochemical biosensor for the monitoring of metabolites and nutrients | Nature Biomedical Engineering [https://www.nature.com/articles/s41551-022-00916-z]
- 13. - PMC Optical biosensors [https://pmc.ncbi.nlm.nih.gov/articles/PMC4986466/]
- 14. sciencedirect.com/topics/engineering/ electrochemical - biosensors [https://www.sciencedirect.com/topics/engineering/electrochemical-biosensors]
- 15. : Optical , Types... | RF Wireless World Biosensors Working Principle [https://www.rfwireless-world.com/terminology/optical-biosensors-working-types-applications]
- 16. Chemosensors and Piezoelectric in Medical Diagnostics... Biosensors [https://pmc.ncbi.nlm.nih.gov/articles/PMC11940703/]
- 17. How Wearable Electrochemical Works — In One Simple... Biosensors [https://www.linkedin.com/pulse/how-wearable-electrochemical-biosensors-works-one-u9dze]
- 18. Based Piezoelectric in the Real World: 5 Uses You'll... Biosensors [https://www.linkedin.com/pulse/piezoelectric-based-biosensors-real-world-5-uses-ynqvc]
- 19. The design, fabrication, and applications of flexible biosensing devices - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6310145/]
- 20. Cardiovascular Wearable Driven by Biosensors ... Nanomaterials [https://www.linkedin.com/pulse/wearable-cardiovascular-biosensors-driven-nanomaterials-technological-cvwic]
- 21. Market Size to Reach USD 3,156.3 mn by 2034 Flexible Substrates [https://dimensionmarketresearch.com/report/flexible-substrates-market/]
- 22. A Review on Biosensors and Recent Development of Nanostructured Materials-Enabled Biosensors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7915135/]
- 23. Frontiers | Recent advances in the functionalization of cellulose... [https://www.frontiersin.org/journals/nanotechnology/articles/10.3389/fnano.2025.1599944/full]
- 24. Current development of stretchable self-powered technology based on... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10126507/]
- 25. Paper and Flexible as Materials for Biosensing Platforms... Substrates [https://www.nature.com/articles/srep08719?error=cookies_not_supported]
- 26. Frontiers | Microfluidic for rapid detection of foodborne... biosensors [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2025.1536928/full]
- 27. Technologies and applications in wireless for real-time... biosensors [https://link.springer.com/article/10.1007/s44258-024-00041-3]
- 28. How Energy System For Harvesting Sensor Network Works... Wireless [https://www.linkedin.com/pulse/how-energy-harvesting-system-wireless-sensor-network-works-ppqlf]
- 29. in the Real World: 5 Uses You'll Actually See... Microfluidic Biosensors [https://www.linkedin.com/pulse/microfluidic-biosensors-real-world-5-uses-youll-actually-e0kyf]
- 30. Biosensors Industry worth $54.37 billion by 2030 [https://www.marketsandmarkets.com/PressReleases/biosensors.asp]
- 31. Biosensors Market Size, Share, Trends & Growth 2030 [https://www.marketsandmarkets.com/Market-Reports/biosensors-market-798.html]
- 32. - Real : A New Era for Time Discovery and... Drug Monitoring Drug [https://www.bio-itworld.com/news/2025/07/01/real-time-drug-monitoring-a-new-era-for-drug-discovery-and-development]
- 33. Approaches of wearable and implantable biosensor towards of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11293309/]
- 34. Frontiers | Multidimensional Circadian Monitoring by Wearable ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2018.00157/full]
- 35. Biosensors | Special Issue : Intelligent Biosignal Processing in Wearable and Implantable Sensors [https://www.mdpi.com/journal/biosensors/special_issues/biosignal_processing_wearable]
- 36. Intelligent Biosignal Processing in Wearable and Implantable Sensors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9220953/]
- 37. Wearable devices for continuous monitoring of biosignals: Challenges and opportunities - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9010050/]
- 38. How Therapeutic Test Works — In One Simple Flow... Drug Monitoring [https://www.linkedin.com/pulse/how-therapeutic-drug-monitoring-test-works-one-jwgge]
- 39. -based biosensors: Biofluid for disease detection Analyzing biomarkers [https://pubmed.ncbi.nlm.nih.gov/40683751/]
- 40. : A comprehensive overview Wearable biosensors [https://pubmed.ncbi.nlm.nih.gov/40683741/]
- 41. Accessing analytes in biofluids for peripheral... | Nature Biotechnology [https://www.nature.com/articles/s41587-019-0040-3?error=cookies_not_supported]
- 42. JMIR mHealth and uHealth - AI-Driven Real-Time Monitoring of... [https://mhealth.jmir.org/2025/1/e73846/]
- 43. Reshaping healthcare with wearable biosensors | Scientific Reports [https://www.nature.com/articles/s41598-022-26951-z]
- 44. How Continuous ( Glucose ) Works — In One... Monitoring CGM [https://www.linkedin.com/pulse/how-continuous-glucose-monitoring-cgm-works-cih0c]
- 45. Impact of Pharmacist-Led Continuous on... Glucose Monitoring [https://www.researchprotocols.org/2025/1/e67014]
- 46. : For Insulin Users and Beyond Continuous Glucose Monitoring [https://www.medscape.com/viewarticle/continuous-glucose-monitoring-insulin-users-and-beyond-2025a10007mx]
- 47. An innovative approach based on health surveillance for the... [https://www.nature.com/articles/s41598-025-93527-y?error=cookies_not_supported&code=f15e7b87-f31f-48fc-82a0-e635f082a175]
- 48. A comprehensive review of wearable devices for non-invasive biosensing - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0165993625002936]
- 49. Biomedical sensing applications of soft, wearable microfluidic systems [https://www.oaepublish.com/articles/ss.2025.45]
- 50. archiv euromedica | vol. 15 | num. 2 [https://journal-archiveuromedica.eu/archiv-euromedica-02-2025/2-Smart-Contact-Lenses-for-Health-Monitoring-Innovations-in-Personalized-Medicine.html]
- 51. Mouthguard biosensor with telemetry system for monitoring of saliva glucose: A novel cavitas sensor - PubMed [https://pubmed.ncbi.nlm.nih.gov/26725934/]
- 52. These smart prototypes could convince... | TechRadar contact lens [https://www.techradar.com/health-fitness/these-smart-contact-lens-prototypes-could-convince-future-me-to-ditch-my-glasses-thanks-to-wireless-power-transfer-and-eye-health-biosensing]
- 53. Revolutionize Smart by Contact Data... Lenses Eye Health Monitoring [https://engineering.purdue.edu/BME/AboutUs/News/2025/chi-hwan-lee8217s-smart-contact-lenses-revolutionize-eye-health-by-monitoring-vital-data-in-real-time]
- 54. - Skin , soft material-enabled bioelectronic system with... conformal [https://pubmed.ncbi.nlm.nih.gov/31999588/]
- 55. - AI : Enhancing Remote Diagnostics and Patient... Driven Telemedicine [https://rsisinternational.org/journals/ijriss/articles/ai-driven-telemedicine-enhancing-remote-diagnostics-and-patient-monitoring/]
- 56. Revolutionizing healthcare in 2025 : From AI to telemedicine [https://blogs.opentext.com/revolutionizing-healthcare-in-2025-from-ai-to-telemedicine/]
- 57. for Wearable : advances in... biosensors health monitoring [https://pubs.rsc.org/en/content/articlehtml/2025/nh/d5nh00141b]
- 58. Wearable Electrochemical Biosensors for Advanced Healthcare Monitoring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11727287/]
- 59. Wearable Biosensor Standardization: How to Make Them Smarter [https://www.mdpi.com/2305-6703/2/3/25]
- 60. Artificial intelligence biosensors: Challenges and prospects - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0956566320304061]
- 61. From Regulation to Reality: A Framework to Bridge the Gap in Digital Health Data Protection [https://www.mdpi.com/2079-9292/14/13/2629]
- 62. Digital health equity frameworks and key concepts: a scoping review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12012343/]
- 63. Editorial: Current development on wearable biosensors towards biomedical applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10442947/]
- 64. Artificial intelligence in wearable biosensing: Enhancing data ... analysis [https://pubmed.ncbi.nlm.nih.gov/40921531/]
- 65. Wearable biosensors for health monitoring: advances in graphene-based technologies - Nanoscale Horizons (RSC Publishing) [https://pubs.rsc.org/en/content/articlelanding/2025/nh/d5nh00141b]
- 66. Fusing Wearable Biosensors with Artificial Intelligence for Mental Health Monitoring: A Systematic Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025234/]
- 67. Anti-Biofouling Strategies for Long-Term Continuous Use of Implantable Biosensors [https://www.mdpi.com/2227-9040/8/3/66]
- 68. Autonomous wearable sensing enabled by capillary microfluidics: a review - Lab on a Chip (RSC Publishing) DOI:10.1039/D5LC00536A [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d5lc00536a]
- 69. Biomedical sensing applications of soft, wearable microfluidic systems [https://www.oaepublish.com/articles/ss.2025.45?to=comment]
- 70. Advances in Wearable Biosensors for Wound Healing and Infection Monitoring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11940385/]
- 71. How Embedded Systems Enable Smart Medical Wearables [https://promwad.com/news/how-embedded-systems-enable-smart-medical-wearables]
- 72. Requirements of Power -Based Biosensor Wearables [https://www.powersystemsdesign.com/articles/power-requirements-of-biosensor-based-wearables/22/15435]
- 73. technology and health monitoring systems | Fiveable Wearable [https://fiveable.me/embedded-systems-design/unit-16/wearable-technology-health-monitoring-systems/study-guide/XB3XNyXo1cLVb315]
- 74. Wearable Biosensors: An Alternative and Practical Approach in Healthcare and Disease Monitoring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7867046/]
- 75. Energy Solutions for Wearable Sensors: A Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8197793/]
- 76. How to optimize system wearable ? power management [https://www.grepow.com/blog/how-to-optimize-wearable-system-power-management.html]
- 77. Recent Advances in Enzymatic Biofuel Cells to Power Up Wearable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12024621/]
- 78. Implantable and Wearable | Sensors ... | Fiveable Biomedical [https://fiveable.me/biomedical-engineering-ii/unit-3/implantable-wearable-sensors/study-guide/4xwyBhs4zQ1RoDz7]
- 79. Review of Flexible Wearable Devices for Sensor ... Biomedical [https://pubmed.ncbi.nlm.nih.gov/36144018/]
- 80. Combined optical-electromechanical wearable sensors for cardiac health monitoring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12152588/]
- 81. Critical overview on the application of sensors and biosensors for clinical analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7112812/]
- 82. How Wearable Alcohol Biosensors Works — In One Simple Flow... [https://www.linkedin.com/pulse/how-wearable-alcohol-biosensors-works-one-simple-flow-dwo7e]
- 83. A standardized validity assessment protocol for physiological signals... [https://research.utwente.nl/en/publications/a-standardized-validity-assessment-protocol-for-physiological-sig]
- 84. : Real-Time STD Diagnostics Wearable Biosensors [https://www.thryve.health/blog/wearable-biosensors-std-diagnostics]
- 85. Advances in Wearable Biosensors for Healthcare: Current Trends, Applications, and Future Perspectives - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11592256/]
- 86. Point-of-Care Wearable for Biomolecular... - Yesil Science Biosensor [https://yesilscience.com/wearable-point-of-care-biosensor-for-biomolecular-assay-in-health-monitoring/]
- 87. : An Alternative and Practical Approach in... Wearable Biosensors [https://pubmed.ncbi.nlm.nih.gov/33535493/]
- 88. A standardized validity assessment protocol for physiological signals... [https://link.springer.com/article/10.3758/s13428-019-01263-9]
- 89. Discovery and Biomarker : Statistical Considerations - PMC Validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 90. and Their Applications | The Scientist Wearable Biosensors [https://www.the-scientist.com/wearable-biosensors-and-their-applications-71360]
- 91. Advances in Wearable Biosensors for Healthcare: Current Trends, Applications, and Future Perspectives [https://www.mdpi.com/2079-6374/14/11/560]
- 92. PPG Biosensors Market Size & Trends 2025 to 2035 [https://www.futuremarketinsights.com/reports/ppg-biosensors-market]
- 93. Global Wearable Market Report Biosensors Edition, Market Size... 2025 [https://www.cognitivemarketresearch.com/wearable-biosensors-market-report]
- 94. Wearable Biosensors Market Size [2034], Share & Trend Report [https://www.businessresearchinsights.com/market-reports/wearable-biosensors-market-107432]
- 95. Trends and Forecast, Wearable -2033 Biosensors Market 2025 [https://www.marketgrowthreports.com/market-reports/wearable-biosensors-market-100386]
- 96. Wireless Wearable : What’s Fueling Growth in Biosensor ? Market 2025 [https://www.linkedin.com/pulse/wireless-wearable-biosensor-market-whats-fueling-np0pf]
- 97. Flexible and Wearable Biosensors for Monitoring Health Conditions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10296135/]
- 98. Recent Advances, Opportunities, and Challenges in Developing Nucleic Acid Integrated Wearable Biosensors for Expanding the Capabilities of Wearable Technologies in Health Monitoring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9688223/]
- 99. Smart Wearables : Medical vs. Consumer Devices for RPM [https://drkumo.com/choosing-the-right-smart-wearables-a-clinical-comparison-of-medical-grade-vs-consumer-wearables-for-rpm/]
- 100. Navigating FDA in the Age of Regulations Wearables [https://www.linkedin.com/pulse/navigating-fda-regulations-age-wearables-geena-george-6vr3c]
- 101. Medical Devices that Incorporate Sensor-based Digital Health Technology | FDA [https://www.fda.gov/medical-devices/digital-health-center-excellence/medical-devices-incorporate-sensor-based-digital-health-technology]
- 102. Guidances with Digital Health Content | FDA [https://www.fda.gov/medical-devices/digital-health-center-excellence/guidances-digital-health-content]
- 103. 2.0: Clinical-Grade Medical Devices Wearables [https://www.delveinsight.com/blog/wearables-2-0-clinical-grade-medical-devices]
- 104. FDA Issues Draft Guidance on AI-Enabled Medical Devices [https://www.orrick.com/en/Insights/2025/01/FDA-Issues-Draft-Guidance-on-AI-Enabled-Medical-Devices]
- 105. Wearable Devices in Clinical Trials: Hype and Hypothesis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6032822/]
- 106. new Fitbit FDA heart rate approves algorithm continuous monitoring [https://newatlas.com/health-wellbeing/fda-approves-fitbit-heart-rate-monitoring-arterial-fibrillation/]
- 107. –2030: Strategic Outlook - Developex Medical Wearables 2025 [https://developex.com/blog/medical-wearables-market-outlook/]
- 108. 7 Crucial Steps for Biosensor Development Success in Med Device [https://intricon.com/7-steps-for-biosensor-success/]
- 109. Size and Economics for Market - PMC Biosensors [https://pmc.ncbi.nlm.nih.gov/articles/PMC7152385/]